The pandemic exacerbated job stress and burnout among nurses, increasing turnover and intentions to leave, in a workforce struggling with severe shortages. Shortages and turnover are associated with decreased quality of care, poor nurse health, and increased costs. This article reports the findings of a study that sought to identify characteristics of the job, work environment, and psychosocial health outcomes that may predict nurses’ intent to stay at their current nursing position within the next year. Utilizing a cross-sectional design, we electronically surveyed working nurses (n = 629) during the summer of 2020 across 36 states. Demographics, work characteristics, and validated measures of anxiety, insomnia, and depressive symptoms were assessed. Logistic regression models identified factors associated with nurses’ intent to stay at their jobs. Colleague support, organizational support, and organizational pandemic preparedness were associated with increased odds of intent to stay, while both mild and moderate/severe depressive symptoms were associated with decreased odds of intent to stay. Because over a quarter of nurses surveyed reported moderate to severe depressive symptoms, which were strongly associated with turnover intention, organizational leadership should examine mental health resources available to nurses and work characteristics that could be contributing to nurses’ poor psychosocial health. Additionally, further research is needed to assess the meaning of organizational support to nurses in a post-COVID-19 context, as well how to create a work environment in which nurses are able to provide support to their colleagues.
Key Words: Nursing, nurses, turnover, turnover intention, intent to stay, COVID-19, mental health, work environment, occupational health, conceptual models, mixed methods design
The ability of healthcare organizations to provide high-quality patient-centered care depends on their ability to maintain an adequate nursing staff (Zaranko et al., 2023). However, high rates of job turnover among registered nurses (RNs) have presented increasingly challenge. In 2022, the staff nurse turnover rate in United States (U.S.) hospitals was 22.5%, compared with a pre-pandemic rate of 15.9% in 2019; and hospitals are experiencing high RN vacancy rates, with an average of 17% across the US (NSI Nursing Solutions, 2023). Over half of hospitals reported RN vacancy rates above 15%. The costs of nursing turnover to healthcare organizations are high, with the average cost of turnover for a bedside nurse estimated at $52,350; each percent change increase in RN turnover costs the hospital an average of $380,600 per year (NSI Nursing Solutions, 2023).
The ability of healthcare organizations to provide high-quality patient-centered care depends on their ability to maintain an adequate nursing staff
Background
Nurse Turnover
Higher nurse turnover rates have profound implications across multiple stakeholders, such as patients and families, nurses, healthcare administrators, and leaders. Turnover has been linked to decreased patient safety and patient satisfaction (Bae, 2022). Indeed, nursing shortages lead to higher nurse-to-patient ratios, which have long been associated with increased burnout, increased job dissatisfaction, and greater turnover intention (Aiken et al., 2002). Poor staffing is also associated with poor patient outcomes, including increased risk of falls and other hospital-acquired conditions (Shin et al., 2019), post-operative sepsis (Flanagan et al., 2020), and mortality (Aiken et al., 2014). Further, nurses report poor staffing as a major workplace concern, driver of burnout, and a reason to seek employment elsewhere (Medvec et al., 2023).
Turnover has been linked to decreased patient safety and patient satisfaction
Strategies to retain nurses and evidence regarding predictors of turnover are timely, with greater emphasis on the topic likely in the coming years. Prior to the COVID-19 pandemic, health services researchers were sounding the alarm about the growing shortage of nurses that would only continue to worsen as a large portion of the nursing workforce prepares for retirement (Buerhaus et al., 2017). The latest data from nationwide nursing workforce surveys are beginning to reflect this change. According to the 2022 National Nursing Workforce Survey, the median age of RNs is 46 years, compared with 52 in 2020 (Smiley et al., 2023). Nurses over the age of 60 make up 22.1% of the nursing workforce, compared with 31.2% in 2020 (Smiley et al., 2023). This decrease in median age is associated with an estimated loss of over 200,000 experienced RNs from the workforce. Additionally, almost 29% of RNs reported that they plan to retire within the next 5 years, compared with 22% in 2020, suggesting that these workforce losses will continue to grow (Smiley et al., 2023). The U.S. Bureau of Labor Statistics (2019) projects 175,900 open nurse positions each year through 2029. This potential shortage will challenge healthcare organizational leaders’ ability to appropriately staff their facilities.
..nurses report poor staffing as a major workplace concern, driver of burnout, and a reason to seek employment elsewhere.
Mental Health Concerns
Healthcare leaders have struggled to maintain adequate nurse staffing levels with the onset of the COVID-19 pandemic. While many hospitals were successful in adding or reallocating beds to accommodate surges of patients with COVID-19 in the first two years of the pandemic (Weiner-Lastinger et al., 2021), nurses and other healthcare workers remained in short supply, resulting in increased workload strain for frontline healthcare workers (Lucchini et al., 2020). In addition to the sheer volume of patients, frontline nurses also dealt with some of the sickest patients they have ever encountered (Hu et al., 2020). These circumstances have resulted in a nursing workforce who suffer from increased adverse mental health outcomes. A meta-analysis on mental health outcomes for nurses globally during the COVID-19 pandemic showed high levels of anxiety, depression, insomnia, trauma, and stress (Varghese et al., 2021). Collectively, the effects of the pandemic on the nursing workforce are considerable both for nurses’ health, patient outcomes, and healthcare organizations.
Collectively, the effects of the pandemic on the nursing workforce are considerable both for nurses’ health, patient outcomes, and healthcare organizations.Even as the public health crisis has been lifted and healthcare organizations begin to find a new normal, early evidence has suggested that poor mental health outcomes continue to impact nurses. A study conducted in 2023 of over 18,000 nurses found that 81% of respondents reported experiencing high levels of stress, 77% reported feeling emotionally drained, and 70% reported worrying that their job is affecting their health (AMN Healthcare, 2023). These percentages are higher than those in 2021, suggesting that nurses’ wellbeing has actually declined further since the height of the pandemic. Similarly, a recent study by the American Nurses Association found that 34% of nurses reported that they did not consider themselves emotionally healthy as a consequence of the pandemic, with 50% reporting that they are considering leaving their current position (American Nurses Foundation, 2022).
Knowledge Gap and Study Aim
While there is a wealth of literature that identifies factors influencing nurses’ intent to stay in their current position (Halter et al., 2017; Hayes et al., 2012; Nei et al., 2015), these factors need re-examined due to changes caused by the pandemic. There has been an increased research focus on nurses’ psychosocial health and its relationship to job turnover during the COVID-19 pandemic; the majority of prior studies have focused on stress, anxiety, and burnout (Falatah, 2021; Poon et al., 2022; Tolksdorf et al., 2022). Few studies have examined the impact of depressive symptoms or insomnia/sleep disturbances on nursing turnover during the COVID-19 pandemic. There is also a paucity of literature that examines the relationship between intent to stay and contextual factors related to the COVID-19 pandemic, particularly factors beyond availability of personal protective equipment (PPE).
These percentages are higher than those in 2021, suggesting that nurses’ wellbeing has actually declined further since the height of the pandemic.
To help healthcare organizations retain their nursing workforce both now and in any future public health crises, it is vital to build our understanding of how these factors impact nurses’ turnover intentions. The aim of this study was to identify individual and work-related factors that predict intent to remain at one’s current nursing job within the next year, including psychosocial health factors and contextual factors specific to the COVID-19 pandemic.
Study Methods
In this model, conditions of work, worker proximal outcomes, and worker outcomes can all impact enterprise outcomes, including turnover.Theoretical Support and Research Questions
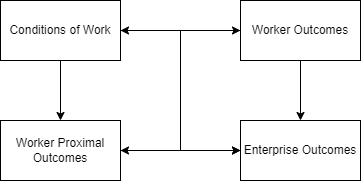
This study was guided by Harvard’s Center for Work, Health and Wellbeing’s conceptual model for integrated approaches to protect and promote worker health (Sorensen et al., 2016). This framework identifies pathways through which working conditions may influence health and safety processes, behaviors, and outcomes. In this model, conditions of work, worker proximal outcomes (such as health and safety behaviors), and worker health outcomes can all impact enterprise outcomes, including turnover (see Figure).
Figure. Adapted Conceptual Model for Integrated Approaches to the Protection and Promotion of Worker Health and Safety
Our research questions were:
- Which demographic factors are associated with nurses’ intent to stay at their current job for the next year?
- Which working conditions, including COVID-19 contextual factors, are associated with nurses’ intent to stay at their current job for the next year?
- Which worker proximal outcomes, including pandemic-specific health and safety behaviors, are associated with nurses’ intent to stay at their current job for the next year?
- Which psychosocial health outcomes are associated with nurses’ intent to stay at their current job for the next year?
Design
We conducted an exploratory, descriptive study with a convergent mixed methods design to understand how the pandemic impacted nurses’ psychosocial health and work-related outcomes. This article will only report the quantitative portion of the data. The quantitative data were captured in a cross-sectional survey using a secure cloud-based platform for data collection and management (Harris et al., 2019).
Sampling
Recruitment for this study was conducted in June-August 2020 through multiple methods. Recruitment letters were sent via email to nursing program directors at National Institute for Occupational Safety and Health (NIOSH)-funded Education and Research Centers (ERCs) and regional professional nursing organizations, which sent them out to member list servs. This strategy produced a sample that was geographically diverse to represent the differing degrees of COVID-19 infections and hospitalizations in the United States in the early stages of the pandemic. We also recruited using social media platforms (e.g., Facebook, Instagram, LinkedIn, and Twitter) on the authors’ individual and university accounts. Eligibility criteria for participation included being a registered nurse, currently working as a nurse in the US, and having at least 6 months of work experience since initial nurse licensure.
Data Collection and Analysis
The authors’ institutional review board approved this study prior to the start of data collection. The survey was composed of three sections. In the first section, we collected participant sociodemographic information (e.g., age, marital status, gender) and work characteristics (e.g., unit type, work schedule, shift length). These questions were similar to the National Survey of Registered Nurses, a survey conducted every four years by the Health Resources and Services Administration ([HRSA], 2018) In the second section, we used questions developed by the investigators to assess pandemic response, resources, and support. Finally, we assessed psychosocial health using valid and reliable measures for anxiety, insomnia, and depressive symptoms. The Insomnia Severity Index (ISI) is a 7-item measure of insomnia symptoms (Morin et al., 2011). The Generalized Anxiety Disorder (GAD-7) is a 7-item measure of anxiety (Spitzer et al., 2006), and the Patient Health Questionnaire (PHQ-9) is a 9-item survey measuring depressive symptom severity (Kroenke et al., 2001). See Table 1 for a table of variables names, descriptions, and how variables were coded for analysis.
Table 1. Study Variable Names and Descriptions
|
Variable |
Measure |
Recoding |
|---|---|---|
|
Dependent Variable |
||
|
Intent to Stay at Current Job |
Do you plan to be with your current employer one year from now? |
“Yes” coded as intending to stay, “no” or “unsure” coded as not intending to stay |
|
Independent Variables Work Environment |
||
|
Work Setting |
Please specify your work setting. |
Responses coded as “inpatient” or “other” |
|
Job Title |
Which one of the following best describes your job title in your primary work setting? |
Responses coded as “bedside nurse” or “other” |
|
Shift Length |
Which one of the following best describes the shift you typically work? |
Responses coded as “12-hour shift” or “<12-hour shift” |
|
Schedule |
Please specify the shift you typically work? |
Responses coded as “Day”, “Night”, “Evening”, or “Rotating” |
|
Work Status |
For the primary job you held on March, 15, 2020, what best describes your work status? |
Responses coded as “Full-time” “Part-time” or “PRN/Per Diem” |
|
Patients Per Nurse |
During the most recent shift you worked, how many patients did you care for? |
A mean across participants was calculated, and then responses coded as “Above sample average” or “below sample average” |
|
Work hours per week |
In a typical week, how many hours do you work in your primary job? |
Coded as “≤ 40 hours” or “> 40 hours” |
|
Caring for COVID-19 Patients |
Have you provided direct patient care to a known or suspected COVID-19 positive patient since March 15, 2020? |
“Yes” coded as caring for COVID-19 patients, “No” or “Unsure” coded as not caring directly for COVID-19 patients |
|
PPE Shortage (Yes/No) |
Since March 15, 2020, what shortages of PPE have your organization/unit faced? (Select all that apply- Disposable gowns, face shields, gloves, foot covers, etc.) |
Checking any of the options was coded as “yes”, checking none of the options was coded as “no” |
|
PPE Shortage (above or below average) |
See above. |
For each participant, the number of PPE item shortages were summed, then responses were coded as “above sample average” or “below sample average” |
|
Pandemic Preparedness |
How prepared is your organization for providing care for known or suspected COVID-19 positive patients? |
Responses of “Very prepared” or “Prepared” were coded as prepared for the pandemic, responses of “Neither prepared nor unprepared”, “unprepared”, or “very unprepared were coded as not prepared for the pandemic |
|
Colleague Support |
How supported do you feel by your colleagues/coworkers to cope with the COVID-19 pandemic? |
Responses of “Very supported” or “Supported” were coded as supported by colleagues, responses of “Neither supported nor unsupported”, “Unsupported”, or “Very supported” were coded as not supported by colleagues |
|
Organizational Support |
How supported do you feel by your organization to cope with the COVID-19 pandemic? |
Responses of “Very supported” or “Supported” were coded as supported by colleagues, responses of “Neither supported nor unsupported”, “Unsupported”, or “Very supported” were coded as not supported by colleagues |
|
Worker Proximal Outcomes |
||
|
Confidence in caring for COVID-19 patients |
Currently, how confident are you in your ability to provide care to a known or suspected COVID-19 positive patient? |
Responses of “Very confident”, “Confident” and “Somewhat confident” were coded as confident, responses of “Not confident” or “Not at all confident” were coded as not confident |
|
Used suboptimal PPE |
Have you provided care to any isolation patient since March 15, 2020 using less than optimal PPE? |
Responses of “Yes” were coded as using suboptimal PPE in isolation, responses of “No” or “Unsure” were coded as not using suboptimal PPE in isolation |
|
Prepared to use PPE |
How prepared do you feel to use PPE, e.g., donning (putting on) and doffing (taking off) PPE? |
Responses of “Very prepared” or “Prepared” were coded as prepared to use PPE, responses of “neither prepared nor unprepared”, “unprepared” or “very unprepared” or coded as unprepared to use PPE |
|
Worker Outcomes |
||
|
Anxiety |
Generalized Anxiety Disorder 7-items (GAD-7) |
Per the scoring instructions for this measure, those with a score of 0-4 were coded as minimal anxiety, those with a score of 5-9 were coded with mild anxiety, those with scores of 10 or greater were coded as moderate/severe anxiety. |
|
Depression |
Patient Health Questionnaire-9 items, (PHQ-9) |
Per the scoring instructions, those with a score of 0-5 were coded as minimal depressive symptoms, those with a score of 5-9 were coded as mild depressive symptoms, and those with scores of 10 or greater were coded as moderate/severe depressive symptoms |
|
Insomnia |
Insomnia Severity Index |
Per the scoring instructions, scores of 0-5 were coded as no clinical insomnia, scores of 6-10 were coded as mild insomnia, scores of greater than 10 were scored as moderate/severe insomnia |
Data analysis included inspection of all variables for distribution, outliers, and missing data. The missing data did not exceed 5% for any of the included variables. Intent to stay at current job in the next year was recoded as a binary variable, with those responding “Agree” or “Strongly Agree” to the item, “I intend to remain at my current nursing job for the next 12 months” coded as intending to stay. A number of predictor variables were similarly recoded as binary, including colleague support, organizational support, and organizational pandemic preparedness (see Table 1 for detailed descriptions of variable recoding). After cleaning the data, we calculated descriptive statistics.
Because our outcome variable had been recoded as binary variable, we next conducted bivariate logistic regressions to test the associations between each potential predictor and intent to stay at current nursing job for the next year. These predictors were selected using the conceptual model, and included demographics, working conditions, worker proximal outcomes, and worker outcomes. Demographic variables tested included age, gender, race, ethnicity, marital status, and having children in the home. Working conditions tested included work setting, position (or job title), schedule, shift length, providing direct care for COVID-19 patients, organizational pandemic preparedness, Personal Protective Equipment (PPE) shortages, colleague support, organizational support, weekly work hours, and patients per nurse.
Worker proximal outcome variables tested included confidence in caring for COVID-19 patients, using suboptimal PPE in isolation settings, and feeling well prepared to don/doff PPE. Worker health outcome variables tested include anxiety, insomnia, and depressive symptoms. These logistic regression models provided odds ratios (OR), which indicate odds of reporting intent to stay compared to a reference group (i.e., the odds of someone with severe anxiety reporting intent to stay at their current job compared to someone with minimal anxiety). Lastly, all the variables found to be statistically significant predictors of intent to stay in the bivariate logistic regression models were used in a final multiple logistic regression model predicting intent to stay.
Results
Descriptive statistics of the analytic sample (n = 629) are presented below in Tables 2, 3, and 4. The sample characteristics were similar to those of the 2018 National Sample Survey of Registered Nurses (NSSRN), with a slightly younger average age and a greater proportion working in the hospital setting (HRSA, 2018). Demographic sample data indicated that 93% of the sample were female, 79% were white, 65% were married or partnered, and 50% had children living in the home. The sample demographics also The majority of respondents were bedside nurses (79%), working 12-hour shifts (59%), and working full time (82%). showed that participants were highly educated, with 78% having a bachelor’s degree or higher. The majority of respondents were bedside nurses (79%), working 12-hour shifts (59%), and working full time (82%). The vast majority reported a shortage of at least one type of PPE at their workplace (95%), while 77% reported having cared directly for patients with COVID-19 before, and 79% reported that their organization was prepared to care for such patients. The majority also reported feeling supported by their colleagues in getting through the pandemic (79%), while 59% reported feeling supported by their organization.
Table 2 Sample Demographic Characteristics
|
|
Total Sample |
Intends to be with employer in 1 year |
Does not intend to be with employer in 1 year |
|---|---|---|---|
|
Age Less than 30 years old 31-40 years old Over 40 years old |
135(22.6%) 153(25.6%) 309(51.8%) |
82(19.1%) 108(25.1%) 240(55.8%) |
53(31.7%) 45(27%) 69(41.3%) |
|
Gender Female Male |
549(92.9%) 39(6.6%) |
389(91.8%) 33(7.8%) |
160 (95.8%) 6 (3.6%) |
|
Ethnicity Hispanic Non-Hispanic Unknown |
41(7%) 542(92.2%) 5(0.8%) |
31(7.3%) 389(92%) 3(0.7%) |
10(6.1%) 153(92.7%) 2(1.2%) |
|
Race White Non-white |
468(78.7%) 127(21.3%) |
332(77.4%) 97(22.6%) |
136(81.9%) 30(18.1%) |
|
Marital Status Married/Partnered Widowed/Divorced Never Married |
389(65.5%) 76(12.8%) 129(21.7%) |
292(68.2%) 54(12.6%) 82(19.2%) |
97(58.4%) 22(13.25%) 47(28.3%) |
|
Children Children at home No children at home |
298(50.5%) 292(49.5%) |
233(55%) 191(45%) |
65(39.2%) 101(60.8%) |
|
Educational Level Diploma in Nursing Associate’s Degree Bachelor’s Degree Master’s Degree Doctorate |
12(2%) 116(19.5%) 352(59.1%) 99(16.6%) 17(2.9%) |
11(2.6%) 87(20.3%) 244(56.9%) 72(16.8%) 15(3.5%) |
1(0.6%) 29(17.4%) 108(64.7%) 27(16.2%) 2(1.2%) |
|
Note. n=597 |
|||
Table 3. Descriptive Statistics of Working Conditions
|
|
Total Sample |
Intends to be with employer in 1 year |
Does not intend to be with employer in 1 year |
|---|---|---|---|
|
Work Setting Inpatient setting Other setting |
458(76.7%) 139(23.3%) |
324(75.4%) 106(24.6%) |
134(80.2%) 33(19.8%) |
|
Job Title Bedside Nurse Other |
498(79.4%) 129(29.6%) |
327(72.2%) 102(23.8%) |
146(88%) 20(12%) |
|
Shift length 12-hour shift Other |
351(58.8%) 246(41.2%) |
232(54) 198(46) |
119(71.3%) 48(28.7%) |
|
Schedule Day Night Evening Rotating |
413(69.8%) 119(20.1%) 28(4.7%) 32(5.4%) |
304(71.4%) 80(18.8%) 19(4.5%) 23(5.4%) |
109(65.7%) 39(23.5%) 9(5.4%) 9(5.4%) |
|
Work status Fulltime Parttime Per Diem/PRN |
489(82.1%) 84(14.1%) 23(3.9%) |
349(81.4%) 64(14.9%) 16(3.7%) |
140(83.8%) 20(12%) 7(4.2%) |
|
Patients per nurse Over sample average Under sample average |
254 (42.5%) 343 (57.5%) |
198 (46.1%) 232(53.9%) |
56(33.5%) 111(66.5%) |
|
Work hours per week Less than or equal to 40 hours Greater than 40 hours |
420(70.4%) 177(29.6%) |
299(69.5%) 131(37.5%) |
121(72.5%) 46(27.5%) |
|
Caring for Covid patients Yes No |
462(77.4%) 135(22.6%) |
322(74.9%) 108(25.1%) |
140(83.8%) 27(16.2%) |
|
PPE Shortages Yes No |
566(94.8%) 31(5.2%) |
403(93.7%) 27(6.3%) |
163(97.6%) 4(2.4%) |
|
PPE Shortage Above sample average Below sample average |
285(47.7%) 312(52.3%) |
190(44.2%) 240(55.8%) |
95(56.9%) 72(43.1%) |
|
Preparation of organization for COVID-19 pandemic Prepared Not prepared |
470(79.4%) 122(20.6%) |
368(86.6%) 57(13.4%) |
102(61.1%) 65(38.9%) |
|
Colleague Support Yes No |
457(76.8%) 138(23.2%) |
361(84%) 69(16%) |
96(58.2%) 69(41.8%) |
|
Organizational Support Yes No |
350(58.7%) 246(41.3%) |
301(70.2%) 128(29.8%) |
49(29.3%) 118(70.7%) |
|
Note. n=597 |
|||
Table 4. Descriptive Statistics of Worker Outcomes
|
|
Total Sample |
Intends to be with employer in 1 year |
Does not intend to be with employer in 1 year |
|---|---|---|---|
|
Worker Proximal Outcomes |
|||
|
Confidence in caring for Covid-19 patients Confident Not entirely confident |
390(65.9%) 202(34.1) |
291(68.3%) 135(31.7%) |
99(59.6%) 67(40.4%) |
|
Used suboptimal PPE Yes No |
289(48.7%) 305(51.3) |
185(43.3%) 242(56.7%) |
104(62.3%) 63(37.7%) |
|
Prepared to use PPE Yes No |
532(89.3%) 64(10.7%) |
391(91.1%) 38(8.9%) |
141(84.4%) 26(15.6%) |
|
Worker Outcomes |
|||
|
Depressive Symptoms Minimal Mild Moderate/Severe |
241(40.4%) 187(31.3%) 169(28.3%) |
202(47%) 135(31.4%) 93(21.6%) |
39(23.4%) 52(31.1%) 76(45.5%) |
|
Anxiety Minimal Mild Moderate/Severe |
277(46.4%) 183(30.7%) 137(22.9%) |
216(50.2%) 138(32.1%) 76(17.7%) |
61(36.5%) 45(27%) 61(36.5%) |
|
Insomnia Minimal Mild/moderate Moderate/Severe |
258(43.2%) 228(38.2%) 111(18.6%) |
206(47.9%) 157(36.5%) 67(15.6%) |
42(31.1%) 71(42.5%) 44(26.4%) |
|
Note. N=597 |
|||
Table 5. Multiple logistic regressions on the impact of demographics, working conditions, and worker outcomes on odds of intent to stay at current job in the next year
|
|
Odds Ratio |
Standard Error |
95% Confidence Interval |
p-value |
|---|---|---|---|---|
|
Age (vs. <31 years old) 31-40 years old Over 40 years old |
1.17 1.41 |
0.38 0.44 |
0.62-2.21 0.77-2.61 |
0.627 0.264 |
|
Marital Status (vs. married/partnered) Widowed/Divorced Never married |
0.77 1.22 |
0.26 0.40 |
0.40-1.49 0.69-2.18 |
0.437 0.492 |
|
Children at home |
1.60 |
0.38 |
1.01-2.55 |
0.047* |
|
Job Title Bedside nurse/Nurse Practitioner |
0.95 |
0.38 |
0.47-1.92 |
0.884 |
|
12-hour shift (vs. other) |
0.70 |
0.20 |
0.40-1.22 |
0.213 |
|
Direct care for Covid Patients |
1.08 |
0.34 |
0.59-2.01 |
0.795 |
|
Organization well-prepared for COVID-19 |
1.72 |
0.47 |
1.02-2.94 |
0.044* |
|
PPE Shortage above sample average |
0.99 |
0.23 |
0.63-1.57 |
0.973 |
|
Supported by colleagues |
1.90 |
0.49 |
1.14-3.16 |
0.014* |
|
Supported by organization |
2.42 |
0.65 |
1.43-4.08 |
0.001*** |
|
Patients per nurse over sample average |
1.22 |
0.30 |
0.75-1.99 |
0.412 |
|
Confident in caring for Covid-19 patients |
0.80 |
0.20 |
0.50-1.30 |
0.373 |
|
Used suboptimal PPE in isolation |
0.90 |
0.22 |
0.55-1.46 |
0.672 |
|
Well prepared to don/doff PPE |
1.48 |
0.50 |
0.77-2.85 |
0.245 |
|
Depression (vs. minimal depression) Mild Moderate/Severe |
0.50 0.27 |
0.16 0.10 |
0.28-0.94 0.13-0.57 |
0.031* 0.001*** |
|
Anxiety (vs. minimal anxiety) Mild Moderate/Severe |
1.63 1.04 |
0.50 0.38 |
0.90-2.99 0.51-2.12 |
0.109 0.921 |
|
Insomnia (vs. minimal insomnia) Mild Moderate/Severe |
1.09 1.48 |
0.33 0.58 |
0.61-1.97 0.69-3.17 |
0.759 0.318 |
|
Note. n=570 *p<0.05, **p<0.01, ***p<0.001 |
||||
In examining worker outcomes, most participants felt prepared to don and doff PPE (89%), but almost 50% reported having to use suboptimal PPE in isolation. Interpretation of descriptive statistics also suggested poor psychosocial health outcomes, with 28% reporting moderate/severe depressive symptoms, 23% reporting moderate/severe anxiety, and 19% reporting moderate/severe insomnia. Interpretation of descriptive statistics also suggested poor psychosocial health outcomes...
Bivariate logistic regression models were conducted to test the association between each demographic, work, psychosocial health, and COVID-19 specific variable and intent to stay at current nursing job in the next year. Of the variables tested in these bivariate models, 16 were statistically significant predictors of intent to stay (See linked Supplemental Digital Content 1).
All statistically significant predictors of intent to stay were included in the final multiple logistic regression model (Table 4). In this model, having children at home (OR 1.60, 95% CI = 1.01-2.55, p = 0.046), colleague support (OR 1.90, 95% CI = 1.14-3.16, p = 0.014), organizational support (OR 2.42, 95% CI = 1.43-4.08, p = 0.001), and perception of organization as well prepared to care for COVID-19 patients (OR 1.72, 95% CI = 1.02-2.94, p = 0.044) remained statistically significant predictors of increased odds of intent to stay, while both mild (OR 0.50, 95% CI 0.28-0.94, p = 0.031) and moderate/severe depressive symptoms (OR 0.26, 95% CI = 0.13-0.57, p<0.001) remained statistically significant predictors of decreased odds of intent to stay.
Discussion
...conditions of work, worker proximal outcomes, and worker health outcomes all impacted nurse turnover intentions.This study identified numerous individual and work-related factors associated with nurses’ intent to stay in their current nursing position. Aligned with our theoretical framework, conditions of work, worker proximal outcomes, and worker health outcomes all impacted nurse turnover intentions. Findings on the relationship between turnover intention and individual demographic variables were consistent with previous research (Hayes et al., 2012); for example, having children living in the home was associated with greater conditions of work, worker proximal outcomes, and worker health outcomes all impacted nurse turnover intentions.odds of intent to stay, compared with those who did not have children living in the home. It is notable that this relationship is consistent with prior turnover research despite the context of the COVID-19 pandemic, which may have had an impact on nurses’ work-life balance and childcare responsibilities, as well as concern over transmission of the virus to their children.
Demographic Factors
These findings are consistent with other studies conducted on the experiences of nurses, which suggest that while nurses did report anxiety over transmitting COVID-19 to their children, as well as fear of contracting the virus themselves and dying and leaving their children without a parent, they also felt a strong sense of professional responsibility and love of nursing that may account for the lack of change in the relationship between parental status and intent to stay (Coşkun Şimşek & Günay, 2021). Additionally, these data were collected in summer 2020, when most children would not typically be in school, meaning that parents would have had to make childcare arrangements regardless, since school was not in session.
Therefore, it is possible that childcare responsibilities did not change significantly for nurses during this period of the pandemic. It is also possible that when these data were collected, many nurses with children in the household were likely to have a spouse or partner who was working remotely, again making it possible that childcare responsibilities did not change significantly. However, recent literature (Çakmak & Öztürk, 2021) has suggested that parenting stress increased significantly for healthcare and workers during the COVID-19 pandemic; data collected later in the pandemic on the impact of being a parent on intent to stay may show a change in this relationship.
...organizational leaders could strengthen their ability to retain nurses by proactively preparing for future public health crises
Conditions of Work
Our findings also identified COVID-19 specific variables related to intent to stay in bivariate regression models, including providing direct care for COVID-19 patients, organizational preparedness for COVID-19 response, PPE shortages, preparation to use PPE correctly, and confidence in caring for COVID-19 patients, with perceived organizational preparedness for the pandemic remaining significant in the final multivariable model. This suggests that organizational leaders could strengthen their ability to retain nurses by proactively preparing for future public health crises, and clearly communicating plans to their nursing staff.
However, in the multivariable regression analysis, the strongest predictors of increased odds of intent to stay were colleague and organizational support. Those who reported feeling supported by their colleagues were nearly twice as likely to report intent to stay compared with those who did not report feeling this colleague level of support (OR 1.90, 95% CI 1.14-3.16, p = 0.014). Those who reported feeling supported by their organization showed 2.4 times higher odds of reporting intent to stay compared with those who did not report feeling organizational support (OR 2.42, 95% CI 1.43-4.08, p = 0.001). This suggests that these support systems are more important to turnover intention than COVID-19 Those who reported feeling supported by their colleagues were nearly twice as likely to report intent to stay compared with those who did not report feeling this colleague level of supportcontextual factors. These findings are supported by other studies conducted during the COVID-19 pandemic, with systematic reviews of turnover intention during the COVID-19 pandemic finding that organizational, leadership, supervisor, and colleague support are consistently associated with lower turnover intention among nurses (Falatah, 2021; Poon et al., 2022; Tolksdorf et al., 2022).
Worker Health Outcomes
In bivariate analyses, depressive symptoms, anxiety, and insomnia were all associated with decreased odds of intent to stay, but in the final multivariate model, only mild and moderate/severe depressive symptoms remained significant. Those with mild depressive symptoms had 50% lower odds of reporting intent to stay compared to those with minimal depressive symptoms, while those with moderate/severe depressive symptoms had 73% lower odds of reporting intent to stay. Considering that 60% of participants reported some level of depressive symptoms, this has significant implications for healthcare organizational leaders focused on retaining their nursing workforce. The most recent state of the science evaluation of depression in nurses revealed a multi-decade investigation into the risk factors, protective factors, prevalence, and impact on worker health and productivity (Brandford & Reed, 2016). These findings align with the results of this investigation, which noted that nurses are at nearly twice the risk of depression compared to other professions, with risk factors including female gender, shift work, and working in acute care setting.
Additionally, though the impact of the pandemic on the day-to-day for hospitals in the United States has decreased significantly and the public health crisis was lifted in May 2023 (CDC, n.d.), there are still concerning signs that nurses’ mental health continues to suffer. A survey conducted by the American Nurses’ Foundation (2022) found that 30% of nurses surveyed reported that they are “not emotionally healthy,” with younger nurses particularly likely to report poor emotional health. Nurses under the age of 35 were also more likely than their peers to report feeling anxious (66%), depressed (43%), and burned out (66%). ...there are still concerning signs that nurses’ mental health continues to suffer.
Occupational health psychologists have documented the significant conceptual overlap between depression/depressive symptoms and the emotional exhaustion component of occupational burnout, and indeed, some of the items used to measure depressive symptoms and burnout are quite similar. For example, both capture feelings of being fatigued and drained of energy (Quick & Tetrick, 2011). It is therefore possible that the high percentage of nurses reporting moderate/severe depressive symptoms (e.g., 28% compared with the national average of 2.8-4.2%) is related to exhaustion and burnout from prolonged elevated workloads and extended working hours during the pandemic (Villarroel, 2020). Given the well-established relationship between burnout and nurse turnover/turnover intention, it would also be unsurprising to find a similar relationship between depressive symptoms and intent to stay (Dall’Ora et al., 2020). Further research is warranted to understand more about these relationships and potential causation.
Implications for Research and Practice
Additional research is needed to assess more specifically what organizational support means to nurses in the pandemic and post-pandemic context. Research about how healthcare organizations and nursing management can facilitate colleague support systems and foster a work environment that is conducive towards nurses supporting each other could also be beneficial for workforce and organizational health. Next, research efforts should be directed toward determining how nursing work environments can be modified to protect against depressive symptoms, which has potential to improve retention, particularly in the context on an ongoing global healthcare worker crisis.
Additional research is needed to assess more specifically what organizational support means to nurses in the pandemic and post-pandemic context.
In practice, healthcare leaders should assess the adequacy of the mental health resources provided for nurses, as well as potential barriers to accessing these resources, since nurses and other healthcare workers have historically been poor users of such services (Gold et al., 2016; Lee et al., 2020; Mensik, 2021). Healthcare organizations and leadership can support both the health of the nursing workforce and the entire organization by prioritizing mental healthcare and striving to reduce stigma. Occupational health staff at healthcare organizations are particularly well positioned to help reduce depressive symptoms in the nursing staff and improve retention. Occupational health staff who work for healthcare organizations can provide mental health screening, as well as clinical support, education, and advocacy in the workplace for RNs experiencing depression or other mental health concerns (Brandford & Reed, 2016).
Healthcare organizations and leadership can support both the health of the nursing workforce and the entire organization by prioritizing mental healthcare and striving to reduce stigma.
In addition to providing support for RNs on an individual basis, both occupational health staff and organizational leaders should focus on promoting healthy work environments and advocating for organizational level policies and practices that protect nurses against depression, burnout, and other poor mental health outcomes. Notably, a recent study by Aiken et al. (2023) found that nurses reported that interventions designed to improve patient care delivery were more important to their mental health than interventions designed specifically to improve their mental health (e.g., wellness programs and resilience training); 87% of nurses surveyed identifying improving nurse staffing as the highest ranked intervention (Aiken et al., 2023). This signals that while hospital leadership should certainly make sure nurses have access to adequate mental health resources, it is equally, if not more important, to assess how the workplace might be impacting staff mental health and engage in a process of continuous improvement.
...nurses reported that interventions designed to improve patient care delivery were more important to their mental health than interventions designed specifically to improve their mental health
Study Limitations
There were limitations to this study. The period of data collection captured a particular moment in time during the COVID-19 pandemic, which has been a rapidly changing landscape for healthcare workers. It is possible that if the data had been collected during a different period of the pandemic, results could be different. Additionally, the cross-sectional, nonexperimental design and of the data collection limits our ability to draw strong conclusions on causality. Conclusions could be strengthened with longitudinal studies on this topic. Lastly, intention to leave is our best indicator of future turnover, but it is not a perfect measure (Vandenberg & Nelson, 1999). It is possible that as work environments have improved due to progress in the effort to mitigate the COVID-19 pandemic, nurses who reported intending to leave their jobs in fact stayed. Conversely, it is possible that as the pandemic endured, nurses’ psychosocial health continued to decline, and nurses who reported intent to stay actually left their jobs.
Conclusion
To adequately staff healthcare facilities and provide high-quality patient care, it is critical to work towards reducing nurse turnover. Given the aforementioned high rates of job turnover among RNs and the predicted increase in nursing shortages, leaders of healthcare organizations and are facing serious challenges to recruit and retain nurses. To adequately staff healthcare facilities and provide high-quality patient care, it is critical to work towards reducing nurse turnover. The results from this study indicated that healthcare organizational leaders should invest in pandemic preparedness and promote interventions to support mental health for nurses to work towards nurse retention. It is important as well to foster work environments where nurses feel supported by their colleagues and their organization.
Acknowledgements/Funding
The datasets generated during the current study are not publicly available due to ongoing analyses but are available from the corresponding author on reasonable request. This study was funded by New York University’s COVID Catalyst Grant (Witkoski Stimpfel).The authors have no relevant financial or non-financial interests to disclose.
Authors
Kathryn Leep-Lazar, BSN, RN
Email: kl3901@nyu.edu
ORCID ID: 0000-0002-7946-3694
Kathryn Leep-Lazar is a 4th year doctoral student at New York University, Rory Meyers College of Nursing. Her doctoral training is partially funded by the National Institute for Occupational Safety and Health (NIOSH) (T42-OH-008422). She earned a BA in psychology from Oberlin College and a BSN from the University of Maryland. Her research interests include the nursing workforce, career trajectories, and modifiable characteristics of the work environment that influence nursing turnover.
Amy Witkoski Stimpfel, PhD, RN
ORCID ID: 0000-0001-5724-0601
Amy Witkoski Stimpfel is an assistant professor at NYU Rory Meyers College of Nursing and the Program Director of the doctoral training program in occupational and environmental health nursing, part of the NY/NJ ERC, funded by the National Institute for Occupational Safety and Health (NIOSH) (T42-OH-008422). Broadly, her research expertise centers on how to optimize nurses’ work environments to improve nurse well-being and clinical outcomes. She earned a BSN from Villanova University and a PhD from the University of Pennsylvania, where she also completed a post-doctoral fellowship in health outcomes and policy research.
References
Aiken, L. H., Clarke, S. P., Sloane, D. M., Sochalski, J., & Silber, J. H. (2002). Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. JAMA, 288(16), 1987–1993. https://doi.org/10.1001/jama.288.16.1987
Aiken, L. H., Lasater, K. B., Sloane, D. M., Pogue, C. A., Fitzpatrick Rosenbaum, K. E., Muir, K. J., & McHugh, M. D. (2023). Physician and Nurse Well-Being and Preferred Interventions to Address Burnout in Hospital Practice. JAMA Health Forum, 4(7), e231809. https://doi.org/10.1001/jamahealthforum.2023.1809
Aiken, L. H., Sloane, D. M., Bruyneel, L., Van den Heede, K., Griffiths, P., Busse, R., Diomidous, M., Kinnunen, J., Kózka, M., Lesaffre, E., McHugh, M. D., Moreno-Casbas, M. T., Rafferty, A. M., Schwendimann, R., Scott, P. A., Tishelman, C., van Achterberg, T., & Sermeus, W. (2014). Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet, 383(9931), 1824–1830. https://doi.org/10.1016/S0140-6736(13)62631-8
American Nurses Foundation. (2022). COVID-19 Two-Year Impact Assessment Survey. American Nurses Foundation. https://www.nursingworld.org/~4a2260/contentassets/872ebb13c63f44f6b11a1bd0c74907c9/covid-19-two-year-impact-assessment-written-report-final.pdf
AMN Healthcare. (2023). The Pandemic’s Consequences: 2023 Survey of Registered Nurses. AMN Healthcare.
Bae, S.-H. (2022). Noneconomic and economic impacts of nurse turnover in hospitals: A systematic review. International Nursing Review, 69(3), 392–404. https://doi.org/10.1111/inr.12769
Brandford, A. A., & Reed, D. B. (2016). Depression in Registered Nurses: A State of the Science. Workplace Health & Safety, 64(10), 488–511. https://doi.org/10.1177/2165079916653415
Buerhaus, P. I., Auerbach, D. I., & Staiger, D. O. (2017, May 3). How Should We Prepare For The Wave Of Retiring Baby Boomer Nurses? | Health Affairs. Health Affairs ForeFront. https://www.healthaffairs.org/do/10.1377/forefront.20170503.059894/full/
Çakmak, G., & Öztürk, Z. A. (2021). Being Both a Parent and a Healthcare Worker in the Pandemic: Who Could Be Exhausted More? Healthcare, 9(5), Article 5. https://doi.org/10.3390/healthcare9050564
Centers for Disease Control and Prevention. (n.d.). End of the federal COVID-19 public health emergency (PHE) declaration. Centers for Disease Control and Prevention. https://archive.cdc.gov/#/details?url=https://www.cdc.gov/coronavirus/2019-ncov/your-health/end-of-phe.html
Coşkun Şimşek, D., & Günay, U. (2021). Experiences of nurses who have children when caring for COVID-19 patients. International Nursing Review, 68(2), 219–227. https://doi.org/10.1111/inr.12651
Dall’Ora, C., Ball, J., Reinius, M., & Griffiths, P. (2020). Burnout in nursing: A theoretical review. Human Resources for Health, 18(1), 1–41. https://doi.org/10.1186/s12960-020-00469-9
Falatah, R. (2021). The Impact of the Coronavirus Disease (COVID-19) Pandemic on Nurses’ Turnover Intention: An Integrative Review. Nursing Reports (Pavia, Italy), 11(4), 787–810. https://doi.org/10.3390/nursrep11040075
Flanagan, J. M., Read, C., & Shindul-Rothschild, J. (2020). Factors Associated With the Rate of Sepsis After Surgery. Critical Care Nurse, 40(5), e1–e9. https://doi.org/10.4037/ccn2020171
Gold, K. J., Andrew, L. B., Goldman, E. B., & Schwenk, T. L. (2016). “I would never want to have a mental health diagnosis on my record”: A survey of female physicians on mental health diagnosis, treatment, and reporting. General Hospital Psychiatry, 43, 51–57. https://doi.org/10.1016/j.genhosppsych.2016.09.004
Halter, M., Boiko, O., Pelone, F., Beighton, C., Harris, R., Gale, J., Gourlay, S., & Drennan, V. (2017). The determinants and consequences of adult nursing staff turnover: A systematic review of systematic reviews. BMC Health Services Research, 17(1), Article 1. https://doi.org/10.1186/s12913-017-2707-0
Harris, P. A., Taylor, R., Minor, B. L., Elliott, V., Fernandez, M., O’Neal, L., McLeod, L., Delacqua, G., Delacqua, F., Kirby, J., Duda, S. N., & REDCap Consortium. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. https://doi.org/10.1016/j.jbi.2019.103208
Hayes, L. J., O’Brien-Pallas, L., Duffield, C., Shamian, J., Buchan, J., Hughes, F., Laschinger, H. K. S., & North, N. (2012). Nurse turnover: A literature review – An update. International Journal of Nursing Studies, 49(7), 887–905. https://doi.org/10.1016/j.ijnurstu.2011.10.001
Health Resources & Services Administration. (2018). 2018 National Sample Survey of Registered Nurses. http://bhw.hrsa.gov/healthworkforce/index.html
Hu, D., Kong, Y., Li, W., Han, Q., Zhang, X., Zhu, L. X., Wan, S. W., Liu, Z., Shen, Q., Yang, J., He, H.-G., & Zhu, J. (2020). Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine, 24, 100424. https://doi.org/10.1016/j.eclinm.2020.100424
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Lee, E., Jeong, Y. M., & Yi, S. J. (2020). Nurses’ Attitudes Toward Psychiatric Help for Depression: The Serial Mediation Effect of Self-Stigma and Depression on Public Stigma and Attitudes Toward Psychiatric Help. International Journal of Environmental Research and Public Health, 17(14), 5073. https://doi.org/10.3390/ijerph17145073
Lucchini, A., Iozzo, P., & Bambi, S. (2020). Nursing workload in the COVID-19 era. Intensive & Critical Care Nursing, 61, 102929. https://doi.org/10.1016/j.iccn.2020.102929
Medvec, B. R., Marriott, D. J., Khadr, L., Ridge, L. J., Lee, K. A., Friese, C. R., & Titler, M. G. (2023). Patterns and Correlates of Nurse Departures From the Health Care Workforce: Results From a Statewide Survey. Medical Care, 61(5), 321. https://doi.org/10.1097/MLR.0000000000001837
Mensik, H. (2021, April 7). Healthcare workers say they need mental health services, but many aren’t getting them. Healthcare Dive. https://www.healthcaredive.com/news/frontline-worker-mental-health-survey-KFF/597916/
Morin, C. M., Belleville, G., Bélanger, L., & Ivers, H. (2011). The Insomnia Severity Index: Psychometric Indicators to Detect Insomnia Cases and Evaluate Treatment Response. Sleep, 34(5), 601–608. https://doi.org/10.1093/sleep/34.5.601
Nei, D., Snyder, L. A., & Litwiller, B. J. (2015). Promoting retention of nurses: A meta-analytic examination of causes of nurse turnover. Health Care Management Review, 40(3), 237–253. https://doi.org/10.1097/HMR.0000000000000025
NSI Nursing Solutions. (2023). 2023 NSI National Health Care Retention & RN Staffing Report. NSI Nursing Solutions, Inc.
Poon, Y.-S. R., Lin, Y. P., Griffiths, P., Yong, K. K., Seah, B., & Liaw, S. Y. (2022). A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: A systematic review with future directions. Human Resources for Health, 20(1), 70. https://doi.org/10.1186/s12960-022-00764-7
Quick, J. C., & Tetrick, L. E. (2011). Handbook of Occupational Health Psychology (2nd ed.). American Psychological Association.
Shin, S., Park, J.-H., & Bae, S.-H. (2019). Nurse staffing and hospital-acquired conditions: A systematic review. Journal of Clinical Nursing, 28(23–24), 4264–4275. https://doi.org/10.1111/jocn.15046
Smiley, R. A., Allgeyer, R. L., Shobo, Y., Lyons, K. C., Letourneau, R., Zhong, E., Kaminski-Ozturk, N., & Alexander, M. (2023). The 2022 National Nursing Workforce Survey. Journal of Nursing Regulation, 14(1, Supplement 2), S1–S90. https://doi.org/10.1016/S2155-8256(23)00047-9
Sorensen, G., McLellan, D. L., Sabbath, E. L., Dennerlein, J. T., Nagler, E. M., Hurtado, D. A., Pronk, N. P., & Wagner, G. R. (2016). Integrating worksite health protection and health promotion: A conceptual model for intervention and research. Preventive Medicine, 91, 188–196. https://doi.org/10.1016/j.ypmed.2016.08.005
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Tolksdorf, K. H., Tischler, U., & Heinrichs, K. (2022). Correlates of turnover intention among nursing staff in the COVID-19 pandemic: A systematic review. BMC Nursing, 21(1), 174. https://doi.org/10.1186/s12912-022-00949-4
U.S. Bureau of Labor Statistics. (2019). Occupation Snapshot: Registered Nurses, 2015-2019. U.S. Bureau of Labor. https://www.bls.gov/iif/oshwc/case/osn-registered-nurses-2015-19.htm
Vandenberg, R. J., & Nelson, J. B. (1999). Disaggregating the Motives Underlying Tiarnover Intentions: When Do Intentions Predict Thrnover Behavior? Human Relations, 52(10), 1313–1336. https://doi.org/10.1177/001872679905201005
Varghese, A., George, G., Kondaguli, S. V., Naser, A. Y., Khakha, D. C., & Chatterji, R. (2021). Decline in the mental health of nurses across the globe during COVID-19: A systematic review and meta-analysis. Journal of Global Health, 11, 05009. https://doi.org/10.7189/jogh.11.05009
Villarroel, M. A. (2020). Symptoms of Depression Among Adults: United States, 2019. 379, 8.
Weiner-Lastinger, L. M., Dudeck, M. A., Allen-Bridson, K., Dantes, R., Gross, C., Nkwata, A., Tejedor, S. C., Pollock, D., & Benin, A. (2021). Changes in the number of intensive care unit beds in US hospitals during the early months of the coronavirus disease 2019 (COVID-19) pandemic. Infection Control and Hospital Epidemiology, 1–5. https://doi.org/10.1017/ice.2021.266
Zaranko, B., Sanford, N. J., Kelly, E., Rafferty, A. M., Bird, J., Mercuri, L., Sigsworth, J., Wells, M., & Propper, C. (2023). Nurse staffing and inpatient mortality in the English National Health Service: A retrospective longitudinal study. BMJ Quality & Safety, 32(5), 254–263. https://doi.org/10.1136/bmjqs-2022-015291


