COVID-19 exposed significant supply issues and operating challenges in hospital labor markets. Travel contingent workers, both local and out-of-state, are utilized by healthcare facilities to fill gaps in full-time staffing during periods of increased patient demand or labor shortages. Registered nurses (RNs), or travel nurses, are an essential component of this group. The increase in patient demand for nursing services related to COVID-19 has exacerbated existing RN labor challenges among full-time RN staff leading to an exponential increase in the national demand for contingent RN labor. Existing workplace issues and burnout have also contributed to increased attrition from hospital roles and from the nursing profession altogether leading to additional increased demand for labor from the contingent RN labor force over and above COVID-19 driven demand. Analyzing data from a major digital travel nursing job marketplace illustrates the significant increase in travel nursing pay rates and their relationship with COVID-19 infection rates. Median ICU travel nurse hourly pay increased 55.4% from 2019 to 2023 leading to unsustainable financial strain on hospitals. As health system leaders aim to re-build their nursing workforce following COVID-19, it is It is essential for public health professionals and policymakers to understand the labor market dynamics at play in these two distinct, but intertwined labor markets to implement evidence-based policy and administrative solutions.
Key Words: Nurse workforce, contingent labor, hospital staffing, care delivery, ICU nurse, med surgical nurse, nursing, COVID-19 pandemic, health policy, travel nurses
Hospital leaders in the United States (U.S.) have noted significant fluctuations in patient demand across service lines from 2020 to 2023 due to the COVID-19 pandemic (Messner, 2022). Contingent clinical staff (also known as travel clinicians), both local and out-of-state, are utilized by healthcare facilities to fill gaps in clinical staffing during periods of increased patient demand. Travel registered nurses (RNs) are an essential and majority component of this contingent workforce, which also includes licensed practical/vocational nurses and allied health professionals.
Travel registered nurses...are an essential and majority component of this contingent workforce...
Travel nurses typically accept 13-week jobs and relocate over 50 miles from their designated home location to be considered a “traveler.” This labor market exists because healthcare organizations often cannot recruit and hire the number and specialty-type of full-time staff nurses needed from local geographic areas (Faller et al., 2017). The travel nurse market existed, and likely exhi bited distinct characteristics, from the full-time, local market for RN labor prior to the COVID-19 pandemic. However, the pandemic challenges revealed the unique characteristics of this “dual labor market” for RNs marked by higher wages compared to the full-time market, a higher degree of wage sensitivity to patient demand, and a national recruitment scope in contrast to the commonly understood local, or state-based RN labor markets. Until recently, a lack of data has made this market difficult to assess; the emergence of online travel nurse marketplaces has provided the basis for the analysis in this paper.
Travel nurses typically accept 13-week jobs and relocate over 50 miles from their designated home location to be considered a “traveler.”
The COVID-19 pandemic exacerbated existing local nursing shortages leading to an exponential increase in the national demand for travel RNs as well as an increase in regional and facility-level competition for contingent RN labor at the national level. In the initial wave of the pandemic in March 2020, New York experienced a 74% increase in hourly pay for travel nurses from pre-pandemic rates (Longyear et al., 2020). In the later months, pay rates for travel RNs increased so much that hospitals anecdotally reported significant losses of full-time staff departing to take contingent jobs, due to higher wages in the travel RN market, further amplifying local, full-time staffing shortages (Bernstein, 2021). Thus, hospitals were losing lower cost full-time labor and simultaneously hiring higher cost contingent labor via staffing agencies from essentially the same labor pool of RNs.
The COVID-19 pandemic exacerbated existing local nursing shortages leading to an exponential increase in the national demand for travel RNs...
These effects led to unsustainable costs for hospitals and subsequent calls for policy intervention such as investigation into anti-competitive practices, price gouging, (American Hospital Association, 2021) regulation through travel nursing rate limits (Bonner, 2021) and reduced or delayed minimum staffing ratio policies designed to protect patients (Dinki, 2022). Policy solutions should seek to address both short-term impacts of the COVID-19 pandemic on the nursing workforce and prioritize evidence-based, long-term solutions to bolster the workforce, reduce facility-level attrition, and prevent general RN labor force drop-out.
These effects have led to unsustainable costs for hospitals and subsequent calls for policy intervention...
Workforce problems in the staff nurse market are established and well known. Issues such as intentional and unintentional understaffing and increased workload can lead to nurse burnout (Lasater et al., 2021b) and moral injury, which further leads to higher turnover rates (Kelly et al., 2021). These concerns can ultimately lead to worse patient outcomes (Jun et al., 2021), a major concern for both public health leaders and hospital administrators.
Despite the integral role of travel nurses in U.S. based healthcare services, there is little information on the travel nurse workforce and contingent labor market, as well as potential policy mechanisms available to support the U.S. health system resilience as it relates to RN labor considering the emergence of this “dual market observation.” Most RN labor policy focuses on the archetype of a local, full-time RN labor market centered around hospital recruitment and employment. The goal of this article is to illustrate the rate trends in the contingent U.S. RN labor market from 2020 to 2023 and to outline a clear relationship between the COVID-19 pandemic and contingent RN pay rates. We suggest that the trends are further evidence of exacerbated and unsustainable underlying challenges in the full-time, local nurse workforce. Policy and administrative interventions will be discussed, given these observations.
Most RN labor policy focuses on the archetype of a local, full-time RN labor market centered around hospital recruitment and employment.
The Contingent RN Labor Market
Healthcare organizations, primarily hospitals, contract with temporary labor staffing agencies that recruit and employ the travel RNs to access the contingent market. This is an important distinction as RNs seeking employment in the full-time, local RN market typically work directly with the employing hospital facility. Staffing agencies charge facilities an hourly bill rate that represents the sum of the nurses’ W-2 taxable wage pay rate, food and housing per diem rates (untaxable stipends), the agency’s profit margin, nurse benefits cost, state and federal taxes, and workers’ compensation costs. In this analysis, we consider the sum of the W-2 wage and non-taxable stipends in the hourly equivalent wages reported as it represents the total compensation provided to the travel RNs. Importantly, the untaxable portion of the travel RN wage also serves to increase the effective wage of the payments, furthering any disparity with standard W-2 staff RN wages.
Healthcare organizations, primarily hospitals, contract with temporary labor staffing agencies that recruit and employ the travel RNs to access the contingent market.
The U.S. healthcare staffing industry in total was estimated at $24 billion (Alvarez, 2021) in size in 2020 and growing to an estimated $64 billion in 2022 (Staffing Industry Analysts, 2023). Large staffing agencies known as managed service providers (MSPs) dominate the market acting as both the staffing contract holder with the hospital and as the staffing operations providers (e.g., recruiting activities). MSPs, such as AMN Healthcare (~12 percent market share), Aya Healthcare (~14 percent market share), and Cross-Country Nursing (~4% market share) act as recruiters, the official employer of record, and “gatekeepers” that maintain supplier relationships with additional external travel nurse staffing agencies. Should an MSP not be able to fill a requisitioned nursing position within a specified period, it will take a two to seven percent fee on top of an external agency’s successful placement of a nurse. Thus, the travel nurse supply chain often has several organizational and profit-taking intermediaries.
...the travel nurse supply chain often has several organizational and profit-taking intermediaries.
The growth of travel nursing pre-2020 can be attributed to the existing well-documented nursing shortage (HRSA, 2017) and the uneven geographic distribution (HRSA, 2013) of nurses across the country. When patient demand for services increases (e.g., flu season), the demand for nursing labor does as well. In addition, burnout among staff RNs is well-documented (Bogue & Bogue, 2020; Raso et al., 2021) and was exacerbated during the pandemic. This has led to further exodus from the profession, thus increasing facility demand for contingent labor.
...federal and state disaster aid programs also likely contributed to the rate elevations as a form of a subsidy that increased the facilities’ ability to pay higher market rates over and above those rates...Higher travel nurse rates are also hypothesized to increase attrition of full-time RN positions on units where travel nurses are common due to inconsistent unit culture, nurses learning of higher pay opportunities, and more challenging patient assignments (Bernstein, 2021; Yang & Mason, 2022). This created a positive feedback loop where a departure of a nurse from a full-time role resulted in increased facility demand for a contingent nurse to fill that role, thus bidding up rates in the contingent market which attracted additional full-time staff into the contingent RN market. This effect, coupled with elevated patient demand due to exponential viral infection patterns, resulted in periods of exponential growth in travel RN wages from 2020 to 2023 (see Figure). It is important to note that federal and state disaster aid programs also likely contributed to the rate elevations as a form of a subsidy that increased the facilities’ ability to pay higher market rates over and above those rates that could be sustained under normal operating finances.
Figure. All RN Specialties Median Total Hourly Pay (January 2020 to March 2023)
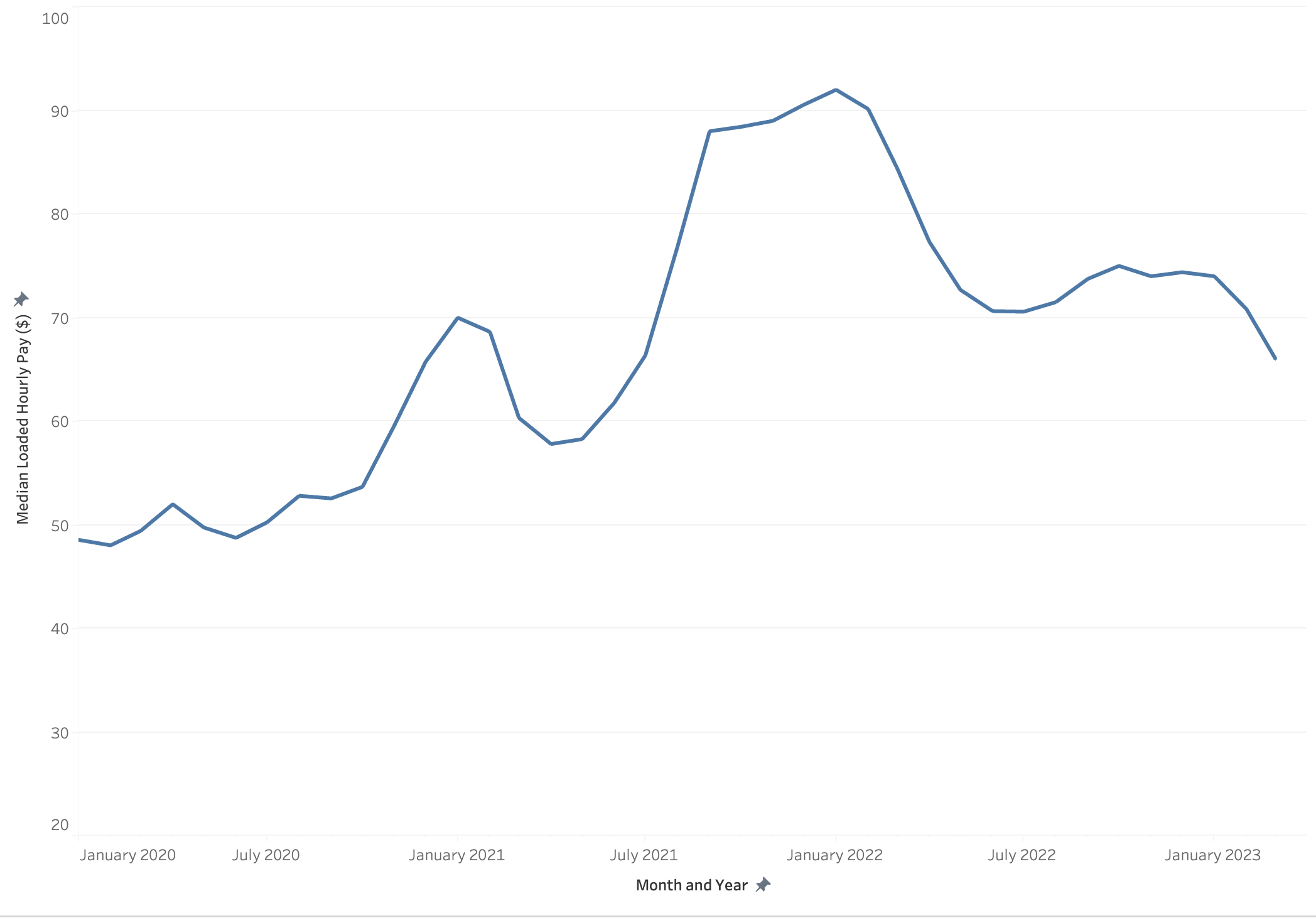
Source: Wanderly Data (n.d.); Author’s Analysis
Components of a Travel Nurse Bill Rate
Staffing Industry Analysts, a contingent staffing market research firm, in collaboration with the National Association of Travel Healthcare Organizations performs an annual benchmarking survey. Results from their 2019 survey in Table 1 illustrate the breakdown of a travel nursing agency bill rate to hospitals (Chang, 2019).
Table 1. Travel Nurse Bill Rate Components 2019
|
Description |
2019 |
|---|---|
|
Bill Rate Revenue |
100% |
|
Wages, Bonuses, Payroll Taxes |
38% |
|
Traveler Housing |
1.2% |
|
Housing Stipends Paid |
20.4% |
|
Meals & Incidentals |
11.7% |
|
Professional Liability Insurance |
0.2% |
|
Workers Compensation (AVG) |
0.6% |
|
Other direct expense |
3.1% |
|
Gross Profit |
24.8% |
|
SG&A |
13.9% |
|
EBITDA |
10.9% |
Methods and Data
Wanderly (n.d.) is a travel nurse staffing marketplace. Wanderly job data from >100 travel nurse staffing agencies and directly from hospitals and MSPs, represent a significant portion of the national market and provides data on travel contingent nursing pay rates from 2019 to 2023. Approximately 1.5 million individual travel nurse job postings were included in this analysis. These real-time rates can provide an important indicator of demand and strain in the national nursing labor market—unlike the Bureau of Labor Statistics (BLS) data set that has well established limitations and time lag (Foley et al., 2014). BLS data for hospital employed (NAICS 622000) RNs is included in Table 2, below, for comparison purposes. The BLS data are a proposed measure of the wages in the full-time, local RN labor market and the Wanderly data represent the national, continent labor market.
Results and Trends in the Travel RN Pay Rates
A temporal relationship between COVID-19 infection incidence rate and the pay rates for travel intensive care unit (ICU) nurses has been established (Longyear et al., 2023). There is a clear directly proportional relationship between COVID-19 infection rates and the number of contingent nursing jobs available, indicating increased hospital demand due to an expected or actual elevation of inpatient admissions. Similarly, as more jobs were advertised (an indication of demand), pay rates increase as well as facilities and staffing agencies competing for a limited supply of RNs (See Figure).
There is a clear directly proportional relationship between COVID-19 infection rates and the number of contingent nursing jobs available...
Table 2 shows the percent increase in median pay rates for full-time, hospital employed RNs (BLS All RN), all travel RNs as well as four major nursing specialties: ICU, emergency room (ER), medical/surgical (MedSurg), and operating room (OR). Median hourly pay rates for all RNs in 2023 remained elevated 54% percent from 2019, but down 12% from the 2022 peak, which was 62% above 2019 baseline numbers. During 2020 to 2022, ICU rates were most elevated indicating the RN specialty most in demand (Table 2) due to increased patient demand for ICU services (Sandhu et al., 2022).
Of note, operating room (OR) nurse pay trends moved with the same relationship to COVID-19 as ICU rates, but with a much smaller magnitude as elective procedure volume fell due to infection risk in 2020 and 2021 (Mattingly et al., 2021). After 2020, OR rates increased drastically and remain elevated into 2023 as facilities sought to increase elective procedure volume to catch up on backlogged cases and improve profitability (Lindrooth et al., 2013) from key surgical service lines. In 2023, OR rates remained the most elevated from 2019 indicating continued and high relative demand for contingent RN labor specializing in operating room-based procedures. Importantly, as shown in Figure 1 and Table 2, RN rates in the contingent labor market have decreased with COVID-19 incidence rates and hospitalizations.
Table 2. RN Specialties Pay Distribution in 2019 to 2023
|
Specialty |
Median Total Pay Rates by Year and Percent Change from 2019 Baseline |
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
2019 |
2020 |
%D |
2021 |
%D |
2022 |
%D |
2023 |
%D |
|
|
BLS All RN |
$36.07 |
$36.94 |
2% |
$37.53 |
4% |
$39.54 |
10% |
N/A |
N/A |
|
All RN |
$46.94 |
$51.52 |
10% |
$71.70 |
53% |
$76.00 |
62% |
$67.00 |
43% |
|
Emergency Dept. |
$46.93 |
$51.18 |
9% |
$74.97 |
60% |
$76.93 |
64% |
$67.67 |
44% |
|
Intensive Care |
$47.42 |
$56.60 |
19% |
$80.86 |
71% |
$78.61 |
66% |
$67.56 |
42% |
|
Medical Surgical |
$43.29 |
$47.75 |
10% |
$71.17 |
64% |
$71.66 |
66% |
$64.06 |
48% |
|
Operating Room |
$50.09 |
$51.89 |
4% |
$70.65 |
41% |
$84.00 |
68% |
$75.07 |
50% |
Source: Wanderly Data (n.d.); Authors Analysis, 2023 only includes January through July 25th. Percentages are rounded to nearest whole number.
Comparing travel nurse wages to BLS data between 2019 and 2022, full-time, hospital-employed RNs realized a 10% increase in wages whereas travel RNs received 62% increases in the median pay advertised during that same time.
Implications and Opportunities for Policy and Administration
Policy discussions surrounding the nursing workforce can be framed under both short-term policy responses and long-term interventions. The continued elevated demand for travel RNs shown above illustrates an ongoing local shortage of full-time nurses available to U.S. healthcare facilities. Hospitals do not seek to hire from the contingent market if they have sufficient supply of less expensive labor in the local, full-time market. As discussed above, full-time nurses are leaving bedside roles for a variety of well-established reasons (Duffield et al., 2004) including burn-out, COVID-19 sickness driven absenteeism (Sakr et al., 2023), moral injury (Čartolovni et al., 2021), and childcare issues (Rabinowitz & Rabinowitz, 2021). Also a factor is a growth of alternative employment opportunities outside of acute-care centers (e.g., virtual care companies) offering work-from-home opportunities as these may be attractive options when compared to the bedside work environment (Joo, 2022). These factors are in addition to general projected labor force shortages in certain geographies (HRSA, 2017). Each of these factors was exacerbated or catalyzed by the emergence and effects of COVID-19.
Hospitals do not seek to hire from the contingent market if they have sufficient supply of less expensive labor in the local, full-time market.
Administrators and policymakers must seek evidence-based solutions to address workforce issues aimed at stemming the outflow from full-time roles and bolstering the RN labor force participation rate across all care settings, but specifically hospitals. While contingent rates have decreased with COVID-19 incidence, demand in the contingent labor market is still well elevated above 2019 and the wage disparity likely still attracts full-time RNs into contingent jobs. In addition to the elevated pay, contingent roles provide more control and work flexibility to RNs compared to full-time employment (Yang & Mason, 2022).
In addition to the elevated pay, contingent roles provide more control and work flexibility to RNs compared to full-time employment...
Despite the elevated cost, the contingent labor market is essential for facilities to fill staffing needs and serves an important function. The evidence suggests that the high rates in the market are largely due to significant elevations in patient demand wherein the contingent market functions in a more competitive manner than the full-time staff market (i.e., increased wages with more demand). Policy solutions aimed at curtailing rates in the contingent market without addressing the underlying issues in the full-time, local market will not necessarily increase the availability of nurse labor to hospitals. Higher rates in the contingent market may actually retain nurses in bedside hospital roles who might otherwise drop out of the labor force entirely.
Despite the elevated cost, the contingent labor market is essential for facilities to fill staffing needs...
Policy interventions should focus on bolstering the national nursing workforce by increasing educational capacity, improving bedside workforce participation rates, and promoting a more equal distribution of the labor force across the United States, particularly in rural areas. Addressing nurse workplace concerns such as working conditions, burnout, moral injury, and violence should be prioritized by administrators in both the short- and long-term solutions (Kelly et al., 2021). Importantly, policymakers cannot only push to increase newly educated nurses output without working to reduce RN labor force drop out issues. Finally, it is essential that administrators and policymakers understand the values of the new generation of nurses (i.e., Generation Z), as policies and organizational change should also optimize for the bedside retention of this group (Hampton & Welsh, 2019).
...policymakers cannot only push to increase newly educated nurses output without working to reduce RN labor force drop out issues.
Short-Term Policy Considerations
Federal Rate Caps and Staffing Ratio Waivers
Sharp contingent nursing pay rate increases have brought calls from hospitals and policymakers for “rate caps” at both the state and federal levels, and, similarly, recommendations to delay or waive safer nurse-to-patient staffing ratio legislation (Bump, 2021; Scales, 2020). While the labor cost pressures for healthcare facilities during the COVID-19 pandemic staffing shock was (and remains) unsustainable, any form of pay-contingent RN rate regulation enacted at the state level will inhibit that state’s hospitals’ ability to attract labor from the competitive national contingent RN market.
It is important to note that the labor market for travel nurses draws from a national pool of RNs who often travel between states.
It is important to note that the labor market for travel nurses draws from a national pool of RNs who often travel between states. A state that legislates rate caps will likely reduce that state’s healthcare facilities’ access to contingent RNs (i.e., nurses will travel to states with the highest pay). Federal rate limits would not have the same draw backs, but this policy is one that risks losing nurses to non-bedside roles and impacting nurse labor force participation rates as the higher wages compensate nurses for the comparatively unfavorable working environment and likely draws some nurses back to the bedside. Waivers of safe staffing ratio legislation would potentially impact patient safety and care quality, which would not be desired outcomes from a health policy perspective.
Improved Workplace Culture and Safety
The COVID-19 pandemic has led to a renewed focus on nurse workplace issues and safety. Nearly half a million workers have left the healthcare workforce since February 2020 citing working conditions and burnout (BLS, 2022). Nurse leaders have long advocated for improved workplace policies including guaranteed mental health support, minimum staffing ratios, paid time off to treat mental health issues, and improved access to nursing education financing support. Similarly, nurses have also long sought policies that would protect them from increased instances of violence, abuse, or physical assault (The Joint Commission, 2018) with little systemic or national improvement.
Financial Incentives
Retention bonuses with time-of-service requirements and elevated hazard pay may also be used to incentivize nurses to stay in full-time positions for extended periods (Bass, 2001). Bonus programs can reduce the immediate pay disparities between travel RN contracts and staff positions. State and federal governments could support this process through targeted funding. The wage disparity between full-time RN and travel RN wages began to decrease in 2023, but policymakers and administrators should consider strategies to close the gap further over the intermediate term to retain and attract nurses into full-time roles. Inhibiting the positive feedback loop dynamic between the two labor markets to the extent that it exists is essential. Evidence suggests that additional compensation for nurses may be a useful tool to reduce burnout-driven retention issues (Ali et al., 2023).
Bonus programs can reduce the immediate pay disparities between travel RN contracts and staff positions.
Others have also identified increased compensation as an essential solution (Pappas et al., 2023). Our analysis supports the concept that staff nurses are often willing to return to the beside for higher travel nurse wages despite a willingness to leave full-time staff nurse jobs in substantially equivalent working conditions. Core labor economic principles (Borjas, 2016) have suggested that labor markets can be self-correcting in that increased wages resulting from increased demand for labor provide a signal for workers to supply an increased quantity of labor hours to employers. Interestingly, this analysis suggests that the contingent RN wage may be serving as the market wage correction mechanism due to the monopsonist features of the full-time local RN labor market (Allegretto & Graham-Squire, 2023).
...this analysis suggests that the contingent RN wage may be serving as the market wage correction mechanism...
Long-Term Policy Implications
Improving Distribution of Labor and License Portability
The Nurse Licensure Compact (NLC) is an interstate licensure compact which offers eligible Licensed Practical/Vocational Nurses (LPN/LVNs) and RNs a multistate license valid for practice in all participating states (currently 41). A nurse holding a multistate license may practice in-person or via telehealth in any NLC state. In non-participating states, separate licensure application processes can deter or delay nurses from practicing. The NLC allows states with comparatively lower nurses per capita to access nursing labor from the national pool.
The NLC allows states with comparatively lower nurses per capita to access nursing labor from the national pool.
The benefits of the multistate license will be fully realized when all 50 states have joined the NLC, allowing the United States to minimize administrative and financial barriers for nurses, resulting in better workforce access for facilities. In practice, this also means that rural and other designated shortage areas can access nursing services via telehealth from areas with a greater concentration of nurses. The NLC contributes to the national elevation of nurse labor competition and may help alleviate some geographic maldistribution issues while potentially supporting the growth of the contingent labor market.
Growing the Nursing Workforce
Several policy options are available to both grow and retain the nursing workforce. Federal loan and tuition repayment programs can increase the number of nurses by reducing the financial barriers to nursing education, as well as bolster the racial, ethnic, economic, and geographic diversity of the labor force. Federal and state funds may be used to increase the capacity of nursing schools to expand class size and improve technological resources such as simulation labs. Previous workforce investment programs have been successful at increasing graduation output from nursing schools through funding for students and increased education of nursing educators (Yoo et al., 2017). Expanding the nurse-educator workforce is also essential in this approach due to a recognized shortage (Stamps et al., 2021). Federal grant programs could also be designed to support the launch or expansion of hospital-affiliated nursing schools to increase availability of practicum locations, such as the one operated by HCA Healthcare, Galen (HCA Healthcare, 2020).
Previous workforce investment programs have been successful at increasing graduation output from nursing schools...
Encourage Safe Implementation of Telenursing Services and Work-from-home Opportunities
Telenursing services may also provide support for both retaining nurses in clinical roles and expanding geographic access to the nursing labor force, particularly in rural areas (McVey, 2023). If preferences for work-from-home in the RN population match that of the general population (Chen et al., 2023), widespread adoption could support retention. Early evidence (Kats & Shmueli, 2023) suggests positive attitudes towards telenursing among nurses. Policymakers and administrators can explore existing models of telenursing across the continuum of care and include models that augment in-person, hospital-based nursing. These models involve nursing surveillance to remotely monitor inpatients to free up in-person unit staff from certain monitoring functions thus reducing workload (Rincon & Henneman, 2018). Similarly, during the pandemic, large scale demonstration projects also experimented with hospital-at-home models for patients, further providing a work-from-home opportunity for RNs (Leff et al., 2022).
If preferences for work-from-home in the RN population match that of the general population, widespread adoption could support retention.
Explore Nursing Reimbursement Models
The current Medicare Part A DRG-based prospective payment system (Yakusheva & Rambur, 2023). encourages hospitals to minimize labor costs via a lack of direct relationship with the intensity and provision of nursing services. Nurse labor represents a significant line item on hospital budgets and therefore the systemic incentives (Paulsen, 2018) encourage understaffing and potentially unsafe patient-to-nurse ratios (Lasater et al., 2021a). New reimbursement models should be explored to better align management incentives with safe and effective levels of staffing that also reduce individual nurse workload (Pappas et al., 2023).
Profession Awareness
Increasing awareness about the nursing profession and related financing opportunities for nursing education is also essential. Nursing campaigns have been referenced as strategies to improve media representation and the image of nurses among the general population (Auerbach et al., 2017;Johnson & Johnson, 2016). Job training initiatives such as the High Growth Job Training Initiative (HGJTI) (Eyster et al., 2012 ) are national grant programs administered by the U.S. Department of Labor Employment and Training Administration. These programs provide demand-driven job training to meet workforce challenges and have been used to support the enhancement of the nursing workforce. Similarly, the Biden Administration, in 2023, announced funding for programs focused on upskilling other healthcare workers, such as LPNs, to become RNs through career pathways and development programs (U.S. Department of Health and Human Services, 2023).
The COVID-19 pandemic exacerbated long-standing issues in the nursing workforce and workplaces.
Conclusions
The COVID-19 pandemic exacerbated long-standing issues in the nursing workforce and workplaces. The pandemic led to a nurse labor demand shock that provided a glimpse into and a further catalyst for the emergence of a large-scale dual labor market for RNs marked by significant rate disparities between short-term (contingent) and long-term (full-time) job markets. It is arguable that this dual market is not a market inefficiency, or problem with the use of travel nurses, as some believe, but rather evidence of the underlying workforce challenges plaguing our nation’s healthcare services organizations with respect to the role of full-time, staff nurses.
The contingent labor market appears to be marked by more competition and sensitivity to the patient demand for services and may contribute to the stabilization of the nursing workforce through its elevated wages. While unsustainable for hospitals under the current healthcare payment landscape, it is essential that policymakers and healthcare administrators work together to innovate to protect, retain, and grow the country’s “most trusted profession” via evidence-based and emerging technological solutions.
Authors
Robert L. Longyear, BS
Email: rll57@georgetown.edu
ORCID ID: 0000-0003-1025-5149
Robert Longyear is VP Digital Health and Innovation at Wanderly, an innovative nursing technology company. Robert was a researcher at the Institute for Medicaid Innovation where he published on high-risk care coordination models, social determinants of health policy. His research work has been published by the American Psychological Association, NEJM Catalyst, and Routledge, Taylor, and France. Robert is the author of A Virtual Care Blueprint (Routledge) a book focused on nursing-led remote-patient monitoring programs. Robert holds a BS in healthcare management and policy from Georgetown University’s School of Nursing and Health Studies.
James R. Puente, MS, MJ, CAE
Email: jpuente@ncsbn.org
Jim Puente has over 30 years of experience in healthcare and has led the successful Nurse Licensure Compact as its Director since 2009. In addition to responsibility for the day-to-day operations of the Nurse Licensure Compact, Jim is also the driving force behind the development and implementation of strategies for regulatory compliance and the Nurse Licensure Compact Commission’s strategic plan. Jim holds an undergraduate degree from the University of Notre Dame, an MS degree in Public Service Management from DePaul University and a Master of Jurisprudence degree in Health Law & Policy from Loyola University School of Law. Jim is also a Certified Association Executive (CAE). Over his extensive history addressing regulatory processes and compliance, Jim has developed key expertise related to critical elements for public protection, strategic implementation of licensure compacts, and the need for a strong workforce, enabled by the removal of barriers to cross-border practice. He often shares his wisdom and experience with other licensed professions and stakeholders seeking to develop and facilitate effective interstate compacts and is widely known as a leader of education and development for associations and regulatory boards.
References
Ali, H., Fatemi, Y., Hamasha, M., & Modi, S. (2023). The cost of frontline nursing: Investigating perception of compensation inadequacy during the COVID-19 pandemic. Journal of Multidisciplinary Healthcare, 16, 1311–1326. https://doi.org/10.2147/JMDH.S402761
Allegretto, S., & Graham-Squire, D. (2023, January 5). Monopsony in professional labor markets: Hospital system concentration and nurse wages. Institute for New Economic Thinking. https://ssrn.com/abstract=4357420
Alvarez, K. (2021, September 7). Healthcare staffing revenue to grow 24% this year: Sia forecast. Staffing Industry Analysts. https://www2.staffingindustry.com/Editorial/Healthcare-Staffing-Report/Sept.-9-2021/Healthcare-staffing-revenue-to-grow-24-this-year-SIA-Forecast
American Hospital Association. (2021, February 4). AHA urges FTC to examine anticompetitive behavior by nurse-staffing agencies and commercial insurers. Advocacy. https://www.aha.org/lettercomment/2021-02-04-aha-urges-ftc-examine-anticompetitive-behavior-nurse-staffing-agencies-and
Auerbach, D. I., Buerhaus, P. I., & Staiger, D. O. (2017). Millennials almost twice as likely to be registered nurses as baby boomers were. Health Affairs, 36(10), 1804–1807. https://doi.org/10.1377/hlthaff.2017.0386
Bonner, T. R. (2021, November 5). Registration and Oversight of Contract Health Care Service Agencies. House co-sponsorship memoranda, Pennsylvania House of Representatives. https://www.legis.state.pa.us/cfdocs/Legis/CSM/showMemoPublic.cfm?chamber=H&SPick=20210&cosponId=36461
Bass, J. L. (2001). Hospitals should replace “sign on bonuses” with “retention bonuses.” Journal of Emergency Nursing, 27(2), 111–112. https://doi.org/10.1067/men.2001.114723
Bernstein. L. (2021). As covid persists, nurses are leaving staff jobs — and tripling their salaries as travelers. The Washington Post. https://www.washingtonpost.com/health/covid-travel-nurses/2021/12/05/550b15fc-4c71-11ec-a1b9-9f12bd39487a_story.html
Bogue, T. L., & Bogue, R. L. (2020). Extinguish burnout in critical care nursing. Critical Care Nursing Clinics of North America, 32(3), 451–463. https://doi.org/10.1016/J.CNC.2020.05.007
Borjas, G. (2016) Labor Economics (7th Edition). McGraw-Hill Education.
Bump, B. (2021, November 9). Amid labor shortage, hospital association asks to delay minimum staffing rules. Times Union. https://www.timesunion.com/news/article/Amid-labor-shortage-hospital-association-asks-to-16603033.php
Čartolovni, A., Stolt, M., Scott, P. A., & Suhonen, R. (2021). Moral injury in healthcare professionals: A scoping review and discussion. Nursing Ethics, 28(5), 590–602. https://doi.org/10.1177/0969733020966776
Chang, A. (2019, July 16). Sia Natho benchmarking survey provides insights into travel nurse trends. Staffing Industry Analysts. https://www2.staffingindustry.com/Editorial/Healthcare-Staffing-Report/Archive-Healthcare-Staffing-Report/2019/July-18-2019/SIA-NATHO-Benchmarking-Survey-provides-insights-into-travel-nurse-trends
Chen, Y., Cortés, P., Koşar, G., Pan, J., & Zafar, B. (2023). The impact of Covid-19 on workers’ expectations and preferences for remote work. National Bureau of Economic Research. http://www.nber.org/papers/w30941
Dinki, T. (2022, January 22). Hochul delays nursing home safe staffing law, profit cap for at least a month. NPR. https://www.wbfo.org/health-wellness/2022-01-03/hochul-delays-nursing-home-safe-staffing-law-profit-cap-for-at-least-a-month
Duffield, C., Pallas, L. O., & Aitken, L. M. (2004). Nurses who work outside nursing. Journal of Advanced Nursing, 47(6), 664–671. https://doi.org/https://doi.org/10.1111/j.1365-2648.2004.03155.x
Faller, M., Dent, B., & Gogek, J. (2017). A single-hospital study of travel nurses and quality: What is their impact on the patient experience? Nurse Leader, 15(4), 271–275. https://doi.org/10.1016/J.MNL.2017.03.016
Foley, M., Ruser, J., Shor, G., Shuford, H., & Sygnatur, E. (2014). Contingent workers: Workers’ compensation data analysis strategies and limitations. American Journal of Industrial Medicine, 57(7), 764–775. https://doi.org/10.1002/ajim.22302
Hampton, D., & Welsh, D. (2019). Work values of generation z nurses. JONA: The Journal of Nursing Administration, 49(10). https://journals.lww.com/jonajournal/fulltext/2019/10000/work_values_of_generation_z_nurses.7.aspx
HCA Healthcare. (2020). Galen College of Nursing. Locations. https://careers.hcahealthcare.com/pages/galen-college-of-nursing
Johnson & Johnson. (2016, February 23). The Johnson & Johnson Campaign for Nursing's Future celebrates fourteen years. Nursing. https://nursing.jnj.com/the-johnson-johnson-i-campaign-for-nursings-future-i-celebrates-fourteen-years
The Joint Commission. (2018, April 17). Physical and verbal violence against health care workers. Sentinel Event Alert, 59. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_59_workplace_violence_4_13_18_final.pdf
Joo, J. Y. (2022). Nurse-led telehealth interventions during COVID-19: A scoping review. CIN: Computers Informatics Nursing, 40(12). https://doi.org/10.1097/CIN.0000000000000962
Jun, J., Ojemeni, M. M., Kalamani, R., Tong, J., & Crecelius, M. L. (2021). Relationship between nurse burnout, patient and organizational outcomes: Systematic review. International Journal of Nursing Studies, 119, 103933. https://doi.org/10.1016/j.ijnurstu.2021.103933
Kats, S., & Shmueli, L. (2023). Nurses’ perceptions of videoconferencing telenursing: comparing frontal learning vs. online learning before and after the COVID-19 pandemic. MedRxiv. https://doi.org/10.1101/2023.05.22.23290291
Kelly, L. A., Gee, P. M., & Butler, R. J. (2021). Impact of nurse burnout on organizational and position turnover. Nursing Outlook, 69(1), 96–102. https://doi.org/10.1016/j.outlook.2020.06.008
Lasater, K. B., Aiken, L. H., Sloane, D., French, R., Martin, B., Alexander, M., & McHugh, M. D. (2021a). Patient outcomes and cost savings associated with hospital safe nurse staffing legislation: an observational study. BMJ Open, 11(12), e052899. https://doi.org/10.1136/bmjopen-2021-052899
Lasater, K. B., Aiken, L. H., Sloane, D., French, R., Martin, B., Reneau, K., Alexander, M., & McHugh, M. D. (2021b). Chronic hospital nurse understaffing meets COVID-19: An observational study. BMJ Quality & Safety, 30(8). https://doi.org/10.1136/bmjqs-2020-011512
Leff, B., DeCherrie, L. V, Montalto, M., & Levine, D. M. (2022). A research agenda for hospital at home. Journal of the American Geriatrics Society, 70(4), 1060–1069. https://doi.org/10.1111/jgs.17715
Lindrooth, R. C., Konetzka, R. T., Navathe, A. S., Zhu, J., Chen, W., & Volpp, K. (2013). The impact of profitability of hospital admissions on mortality. Health Services Research, 48(2pt2), 792–809. https://doi.org/10.1111/1475-6773.12026
Longyear, R., Boxer, R., & Johnson, K. (2020). Travel ICU nurse concerns across COVID-19 hot spots. NEJM Catalyst, 1(5). https://doi.org/10.1056/CAT.20.0504
Eyster, L., Nightingale, D. S., Barnow, B. S., O’Brien, C. T., Trutko, J., & Kuehn, D. (2012, January 9). Implementation and Early Training Outcomes of the High Growth Job Training Initiative: Final Report. Urban Institute. https://www.urban.org/research/publication/implementation-and-early-training-outcomes-high-growth-job-training-initiative-final-report
Mattingly, A. S., Rose, L., Eddington, H. S., Trickey, A. W., Cullen, M. R., Morris, A. M., & Wren, S. M. (2021). Trends in US surgical procedures and health care system response to policies curtailing elective surgical operations during the COVID-19 pandemic. JAMA Network Open, 4(12), e2138038–e2138038. https://doi.org/10.1001/jamanetworkopen.2021.38038
McVey, C. (2023). Telenursing: A concept analysis. CIN: Computers, Informatics, Nursing, 41(5), 275-280. https://journals.lww.com/cinjournal/fulltext/2023/05000/telenursing__a_concept_analysis.4.aspx
Messner, W. (2022). Disparities in demand for COVID-19 hospital care in the United States: Insights from a longitudinal hierarchical study. Health Science Reports, 5(1), e441. https://doi.org/10.1002/HSR2.441
Pappas, S., Brosius, W., Hayes, R., Lawrence, M., McMichael, B., Zimmermann, D., & McCauley, L. (2023). Maximizing the potential value of the nursing workforce. Nursing Outlook, 72(1), 102016. https://doi.org/10.1016/j.outlook.2023.102016
Paulsen, R. A. (2018). Taking nurse staffing research to the unit level. Nursing Management, 49(7), 42-48. https://doi.org/10.1097/01.NUMA.0000538915.53159.b5
Rabinowitz, L. G., & Rabinowitz, D. G. (2021). Women on the frontline: A changed workforce and the fight against COVID-19. Academic Medicine, 96(6), 808-812. https://doi.org/10.1097/ACM.0000000000004011
Raso, R., Fitzpatrick, J. J., & Masick, K. (2021). Nurses’ intent to leave their position and the profession during the COVID-19 pandemic. JONA: The Journal of Nursing Administration, 51(10), 488-494. https://doi.org/10.1097/NNA.0000000000001052
Rincon, T. A., & Henneman, E. (2018). An introduction to nursing surveillance in the tele-ICU. Nursing2020 Critical Care, 13(2), 42-46. https://doi.org/10.1097/01.CCN.0000527223.11558.8a
Sakr, C. J., Fakih, L., Melhem, N. M., Fakhreddine, M., Musharrafieh, U., Banna, H., Doudakian, R., Zahreddine, N. K., Tannous, J., Kanj, S. S., Slade, M., Redlich, C. A., & Rahme, D. (2023). COVID-19 infections and predictors of sickness related absences among healthcare workers: The experience of a tertiary care center with the COVID-19 pandemic. Journal of Occupational and Environmental Medicine, 65(7), 590-594. https://doi.org/10.1097/JOM.0000000000002857
Sandhu, P., Shah, A. B., Ahmad, F. B., Kerr, J., Demeke, H. B., Graeden, E., Marks, S., Clark, H., Bombard, J. M., Bolduc, M., Hatfield-Timajchy, K., Tindall, E., Neri, A., Smith, K., Owens, C., Martin, T., & Strona, F. V. (2022). Emergency department and intensive care unit overcrowding and ventilator shortages in US hospitals during the COVID-19 pandemic, 2020-2021. Public Health Reports, 137(4), 796–802. https://doi.org/10.1177/00333549221091781
Scales, D. (2020). An understaffed hospital battles COVID-19. Health Affairs, 39(8), 1450–1452. https://doi.org/10.1377/hlthaff.2020.00810
Staffing Industry Analysts. (2023). US health staffing market assessment: 2023 update. https://www2.staffingindustry.com/Research/Research-Reports/Americas/US-Healthcare-Staffing-Market-Assessment-2023-Update
Stamps, A., Cockerell, K., & Opton, L. (2021). A modern take on facilitating transition into the academic nurse educator role. Teaching and Learning in Nursing, 16(1), 92–94. https://doi.org/10.1016/j.teln.2020.04.002
U.S. Department of Health and Human Services Health Resources and Services Administration. (2017, July 21). Supply and demand projections of the nursing workforce: 2014-2030. HRSA. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/nchwa-hrsa-nursing-report.pdf
U.S. Department of Health and Human Services Health Resources and Services Administration. (2013, October). The U.S. nursing workforce: Trends in supply and education. HRSA. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/nursing-workforce-trendsoct2013.pdf
U.S. Department of Health and Human Services. (2023).The Biden-Harris administration announces $100 million to grow the nursing workforce. News. https://www.hhs.gov/about/news/2023/08/10/biden-harris-administration-announces-100-million-grow-nursing-workforce.html
U.S. Department of Labor Bureau of Labor Statistics. (2022, January 22). The employment situation-December 2021. BLS News release. https://www.bls.gov/news.release/archives/empsit_01072022.pdf#:~:text=THE%20EMPLOYMENT%20SITUATION%20%E2%80%94%20DECEMBER%202021%20Totalnonfarm%20payroll,the%20U.S.%20Bureau%20of%20Labor%20Statistics%20reported%20today.
Wanderly Data. (n.d.) Home. https://www.wanderly.us/
Yakusheva, O.,& Rambur, B. (2023). How the hospital reimbursement model harms nursing quality and what to do about it. Health Affairs Forefront. https://doi.org/10.1377/forefront.20230526.873299
Yang, Y. T., & Mason, D. J. (2022, January 28). COVID-19’s impact on nursing shortages, the rise of travel nurses, and price gouging. Health Affairs Forefront. https://doi.org/10.1377/forefront.20220125.695159
Yoo, B.-K., Kim, M., Sasaki, T., Ward, D., & Spetz, J. (2017). Program evaluation of a nursing workforce intervention: The Maryland Nurse Support Program II. Nursing Economic$, 35(1), 14–20, 38. https://pubmed.ncbi.nlm.nih.gov/29984943/


