Hispanics comprise more than one third of U.S. COVID-19 cases. This higher prevalence is associated with determinants to access that existed long before the pandemic. Using the Preferred Report Items for Systematic Review and Metanalysis (PRISMA) guidelines, this review examined 20 studies that addressed barriers faced specifically by Hispanics in the United States, Sampling methods are described and the synthesized research findings are organized using the Theoretical Framework of Access, which classified barriers as either structural or personal. Results suggested that Hispanics had lower COVID-19 knowledge than other groups. The article discussion considers possible causes, such as low health literacy levels, an inability to reach or pay for services, a mistrust of healthcare providers, or a lack of access to information. To increase U.S. Hispanics’ COVID-19 knowledge and encourage safer behaviors, culturally sensitive and linguistically appropriate information is needed.
Key Words: COVID-19; health literacy; risk perception; cultural sensitivity; healthcare access; Hispanics; language barriers; PRISMA; Latinx
The COVID-19 virus, caused by a coronavirus and named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was initially reported to the World Health Organization on December 31, 2019 (Cennimo, Bergman, & Olsen, 2021). As it spread worldwide and into the United States, an ethnic disparity became visible: Latinx or Hispanics (henceforth referred to as Hispanics) were more likely to contract COVID-19 than non-Hispanic whites [NHWs] (Centers for Disease Control and Prevention [CDC], 2022). Hispanics comprise over one third of national cases (Moyce et al., 2021), with a mortality 1.9 times higher than cases in NHWs (Gross et al., 2020).
Increased cases in minority populations such as Hispanics have been associated with disparities... Increased cases in minority populations such as Hispanics have been associated with disparities such as overcrowded living spaces, an inability to shelter in place due to work, and status as essential workers (Pflugeisen & Mou, 2021). Further putting Hispanics at risk are disparities in healthcare, which are well documented (Manuel, 2018; Sharma et al., 2018; Singh & Wilk, 2019; Yue, Rasmussen, & Ponce, 2018). For one, they are less likely to have health insurance, making it difficult to receive care (Berchick, Barnett, & Upton, 2019). Due to this lack of insurance, Hispanics also tend to have more preexisting conditions, such as obesity, diabetes, and hypertension, all of which increase morbidity and mortality (Aguayo-Mazzucato et al., 2019; Garg, 2020; Hales, Carroll, Fryar, & Ogden, 2020; Williams et al., 2020).
This is due, in part, to limited or no insurance, which has caused further delays in testing for and treatment of COVID-19Hispanics also tend to have a higher prevalence of specific chronic diseases such as diabetes (Baquero et al., 2020). In a study that evaluated prevalence data (n = 56,290), 29% of Hispanics reported having diabetes, compared to 17% of NHWs. However, NHWs had a higher prevalence of multimorbidities excluding diabetes, but Hispanics still suffered greater rates of infection by COVID-19. This is due, in part, to limited or no insurance, which has caused further delays in testing for and treatment of COVID-19 (Williams et al., 2020). Access to healthcare is critical during a pandemic, but a full understanding of the barriers to access is needed to lower COVID-19 case rates and improve general health for Hispanics.
Although the expansion of healthcare coverage as a result of the Affordable Care Act (2010) has provided opportunities to access healthcare, coverage alone is not enough (Pflugeisen & Mou, 2021; Yue et al., 2018). A person must also be able to navigate the healthcare system. However, Hispanics often have lower health literacy levels than NHWs, as well as language barriers that limit their ability to navigate the system (Edward et al., 2018; Villagra, Bhuva, Coman, Smith, & Fifield, 2019). Determining barriers to access for Hispanics during the COVID-19 pandemic is complex; the objective of this review is to examine how Hispanics access care, as well as the potential barriers to accessing that care during the COVID-19 pandemic.
Theoretical Framework of Access
...the relationship between the demand and supply sides interconnect and overlap...Levesque, Harris, and Russell (2013) synthesized published literature to evaluate conceptualizations of access to healthcare and to develop a broader definition of access. Their synthesis generated a holistic concept of access, including dimensions of accessibility relating to the healthcare system. These dimensions included the organizations supplying the healthcare, or the supply side of access to healthcare, and the ability of persons to use or access healthcare, the demand side of access. The dimensions of accessibility and ability were further broken down into: approachability; acceptability; availability and accommodation; affordability; appropriateness; and the ability to perceive, seek, reach, pay, and engage, respectively (Levesque et al., 2013). As seen in Figure 1, the relationship between the demand and supply sides interconnect and overlap, and the dimensions are not mutually exclusive. The components of the framework allow the operationalism of access to healthcare along the process of obtaining care and benefiting from services.
Figure 1. Theoretical Framework of Access
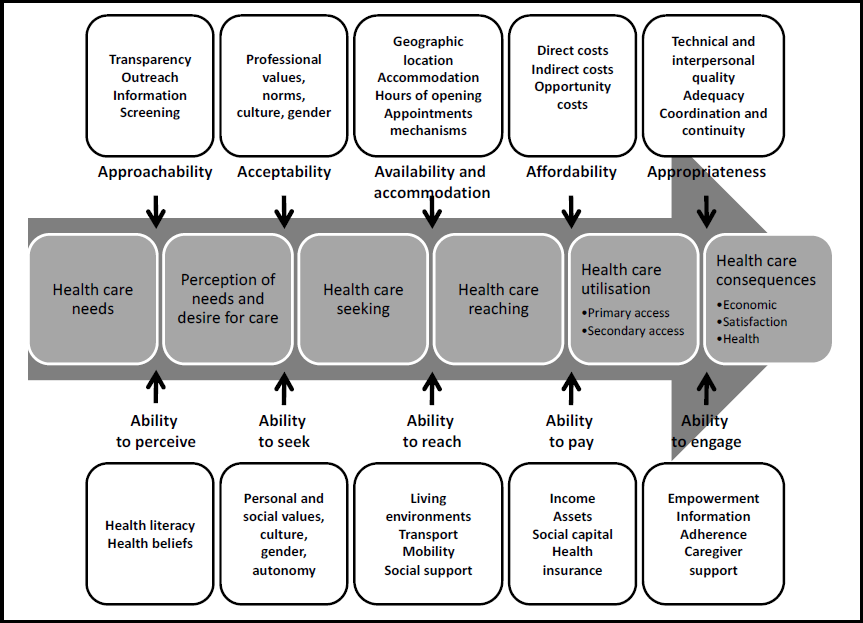
(Levesque, Harris, & Russell, 2013)
...Levesque et al.’s conceptual framework has been beneficial to identify barriers...Levesque et al.’s (2013) conceptual framework of access has been utilized in many recent studies. For example, the design, implementation, and evaluation for a five-year research program to address primary healthcare innovations was informed by this framework (Spooner et al., 2021). A qualitative study aimed at understanding expectations and needs of socially vulnerable patients also used this conceptual framework to inform the development for interview guides (Ngo Bikoko Piemea et al., 2021). Furthermore, Zhao et al. (2021) utilized this framework to identify barriers in accessing internet-based home care through semi-structured interviews with older patients. Consistently, Levesque et al.’s conceptual framework has been beneficial to identify barriers to access from the perspective of a person’s needs and expectations (i.e., demand side) to the services provided (i.e., supply side) by the healthcare system.
Domains of Access
Health information and promotion must be accessible, attainable, and understandable to consumers in order to be considered approachable on the supply side. On the demand side, consumers must be able to perceive the need for healthcare services; they must believe that healthcare is necessary and also understand their own health issues (Levesque et al., 2013).
Health services need to be equitable and free of stigmatization and discrimination to be considered acceptable.Health services need to be equitable and free of stigmatization and discrimination to be considered acceptable. If consumers feel reluctance related to stigmatization or other discriminatory beliefs, they will not seek services on the demand side.
Availability and accommodation rely on the geographical distribution of healthcare facilities within a community. Though those facilities may exist on the supply side, in order to reach them, a person must possess mobility and reliable transportation. Secure housing indirectly affects this because permanent residency makes local services easier to access.
Ability to pay for services relies on health insurance, income, and assets. Having an insurance plan, and the ability to apply that plan, is an entry point to healthcare. Income and assets (e.g., ability to obtain loans) are needed for catastrophic events that may impinge on basic living needs (Levesque et al., 2013). Services must be affordable on the supply side, and consumers must be able to pay for those services on the demand side.
Ability to engage in these services relies on a person’s communication skills...Persons accessing healthcare services should receive a benefit or benefits from doing so (Levesque et al., 2013). Appropriateness indicates effective services and treatments received in a timely manner. Ability to engage in these services relies on a person’s communication skills to voice needs and then participate in treatment decisions.
Sampling Methods
This review utilized the electronic databases PubMed and the Cumulative Index of Nursing and Allied Health (CINAHL). A main search strategy was used in PubMed, and similar combined keywords and subject headings were entered in CINAH (see Table 1). The Boolean operators “OR” and “AND” were applied to narrow the search. All searches were completed, by the author alone, between February and May of 2021.
Table 1.
Key Search Terms
|
Database |
Key Search Terms and Subject Titles Including MeSH |
|
PubMed |
(("health literacy" OR "health knowledge"[tiab] OR "perceived risk" OR "risk perception"[tiab] OR "health seeking"[tiab] OR stigma OR stigmatized OR "Health Literacy"[Mesh] OR "Patient Acceptance of Health Care"[Mesh] OR "Attitude to Health"[Mesh] OR "Social stigma"[Mesh] OR "Social Marginalization"[Mesh] OR "knowledge"[mesh] OR "health behavior"[tiab] OR "health behavior"[Mesh] OR "Health Knowledge, Attitudes, Practice"[mesh] OR "healthcare disparities"[mesh]) AND ("COVID-19"[tiab] OR "COVID-19"[MeSH Terms] OR "COVID-19 Testing"[tiab] OR "covid-19 testing"[MeSH Terms])) AND ((Hispanic[tiab] OR Hispanics[tiab] OR Latino[tiab] OR Latina[tiab] OR latinx[tiab] OR "Hispanic Americans"[Mesh])) |
|
Cumulative Index of Nursing home and Allied Health (CINAHL) |
"perceived risk" OR "risk perception" OR "health belief" OR "health Seeking" OR "Health knowledge" OR "health literacy" OR "healthcare access" OR "stigma*" OR "Stigmatization" OR "disparities" AND "hispanic americans" OR "hispanic" OR "latino" OR "ethnic" OR "ethnicity" AND "COVID-19" OR "COVID-19 Test" OR "Coronavirus" OR "COVID-19 vaccine" |
Studies were assessed according to information addressing the domain from the demand side of access during the COVID-19 pandemic: (1) the perceived risks of COVID-19, (2) seeking health information related to COVID-19, (3) the capacity to reach healthcare services (e.g., testing, treatment, vaccination) related to COVID-19, (4) the ability to pay for healthcare services related to COVID-19, (5) the engagement of healthcare services during the COVID-19 pandemic, and (6) the sample demographics, which must have included Hispanic participants. Once ineligible studies were eliminated, the bibliographies of the remaining were analyzed for additional primary sources. No restrictions were placed on publication dates due to the recent nature of events.
The initial search generated 413 papers. The author then screened the research, removing duplicates (n = 11) and assessing titles for preliminary eligibility criteria, resulting in 82 publications. After applying the six eligibility criteria listed above, and using primary sources extracted from bibliographies, the search yielded 20 total studies. Study designs were: cross-sectional (n = 1), poll (n = 1), qualitative (n = 1), telephone or online surveys (n = 5), reviews (n = 7), retrospective (n = 1), observational (n = 1), and non-specified (n = 2); also included were news report articles (n = 2). The approximate sample size of Hispanic participants across all 20 studies was 1060. This paper used the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Page et al., 2021) to identify and select appropriate studies (see Figure 2).
Figure 2. PRISMA 2020 flow diagram
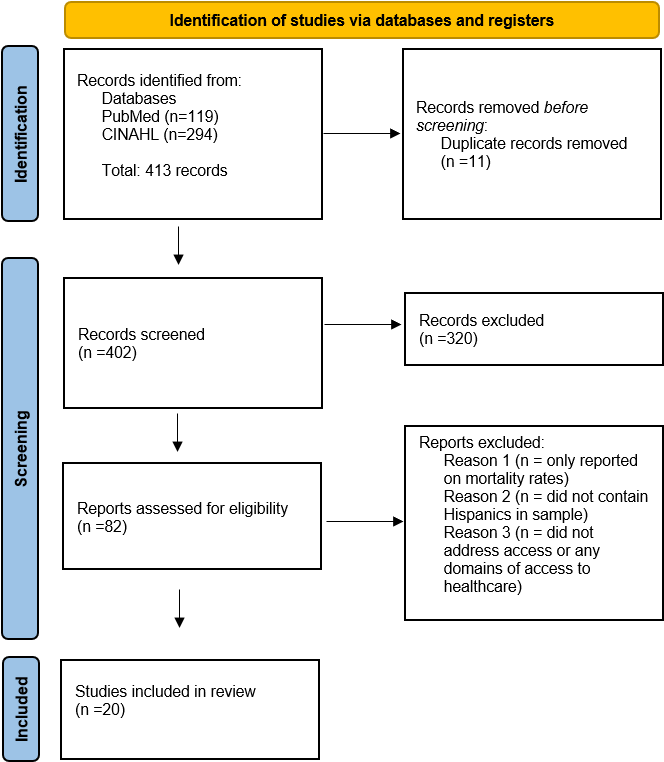
Several additional studies addressed the prevalence of COVID-19 in other minority populations, but these were not included, as this review focused specifically on U.S. Hispanics.
Results
The studies included in this review were divided into two subject areas, personal and structural barriers. Personal barriers were specific to the domains of a person’s ability to perceive the need and seek healthcare for healthcare services. Structural barriers addressed the ability to reach, pay, and engage in healthcare services (see link to full sized Table 2 that includes detailed information about the studies).
Table 2.
Barriers to the Five Domains of the Demand Side of Access
|
Author(s) & Publication Year |
Study Purpose |
Study Design/data collection |
Barrier Type |
Sample Size |
Findings |
Domains of Access |
|
Determine prevalence, risk perception attitude and preventive behavior |
Cross-sectional Questionnaire |
Personal |
n=410 |
Inadequate risk perception and engagement in preventive behavior among Hispanics making them high risk of COVID-19 |
Perceived Risk |
|
|
Measured knowledge, perception of severity, & self-efficacy in relation to preventive behaviors |
Telephone Survey |
Personal |
n=105 farmworkers 67 Non-farmworkers 35 |
Despite knowledge & perceived risk, participants did not adhere to preventive measures |
Perceived Risk |
|
|
Measured fear of COVID-19, information receptivity, knowledge, & self-efficacy in relation to preventive behaviors |
Online Survey |
Personal |
n=483 Hispanics 116 |
Socioeconomic states versus race/ethnicity contributed to less preventive behaviors, Hispanics had less fear of the COVID-19 virus |
Perceived Risk |
|
|
Investigated peoples’ acceptability to COVID-19 vaccine |
Online Survey |
Personal |
n=2006 Hispanics 241 |
Perceived risk was associated with vaccine acceptability in Hispanics |
Perceived Risk |
|
|
Reporting on Hispanics’ skepticism related to COVID-19 |
News report |
Personal |
Hispanics skeptical over disinformation |
Ability to Seek |
||
|
Investigated vaccine hesitancy |
Perspective |
Personal |
Concluded with methods to improving trust, e.g., equity lens |
Ability to Seek |
||
|
Reported on disparities related to COVID-19 |
Literature Review |
Personal |
Identified several areas of disparities related to marginalized communities, e.g., mistrust |
Ability to Seek |
||
|
Describe the experiences of Hispanics hospitalized with COVID-19 |
Qualitative Study Semi-structured phone interviews |
Personal |
n=60 |
Hispanics described initial disease misinformation, economic and immigration fears as contributors to delays in testing and seeking care |
Ability to Seek |
|
|
Assessing vaccine intentions, attitudes & trust |
Online Survey |
Personal |
n=396 Hispanic 99 |
Hispanic women reported they would not receive the vaccine 32.4% versus. 15.4% NHWs |
Ability to Seek |
|
|
Reporting on disparities related to COVID-19 |
News report |
Structural |
Identified living conditions, work obligations, and testing site availability to being barriers of treatment |
Ability to Reach |
||
|
To determine the spatial distribution of COIVD-19 testing by zip code |
Ecological Study Data from repository and 2018 Community Survey |
Structural |
COVID-19 testing has not been proportional to need in New York City |
Ability to Reach |
||
|
Explains how racial/ethnic data collected from testing can contribute to the prevention of spreading disease |
Systematic Review |
Structural |
Identified interventions to address disparities in COVID-19, e.g., collaboration with CVS to implement testing |
Ability to Reach |
||
|
Reporting of HRSA’s weekly voluntary Health Center COVID-19 Survey |
Analysis of a Survey |
Structural |
Reported on initiatives supported by HRSA, e.g., funding to support community clinics and testing |
Ability to Reach |
||
|
Investigated the association b/w racial segregation and COVID-19 rates in Massachusetts |
Utilized Moran’s I index to test the spatial autocorrelation pattern of city/town COVID-19 rates |
Structural |
Testing sites and safety nets were distributed in areas highly populated by minority communities |
Ability to Reach |
||
|
Reviewed contributors to disparities in COVID-19 |
Literature Review |
Structural |
Identified areas of barriers to minorities, e.g., access to testing, limited information |
Ability to Reach |
||
|
Reporting on the disparities among race/ethnicity in COVID-19 |
Editorial Comment |
Structural |
Identified barriers to racial/ethnic communities, e.g., telehealth |
Ability to Reach |
||
|
Describes the effects of telemedicine in vulnerable communities |
Analysis of telemedicine visits |
Structural |
n=270 Hispanic 29 |
Hispanics use of telehealth was disproportionately low |
Ability to Reach |
|
|
To evaluate inequities in telemedicine |
Retrospective |
Structural |
n=148,402 |
Non-English-speaking patients had lower rates of telemedicine and Hispanics had less video access |
Ability to Pay |
|
|
Vaccine monitoring: access, information |
Polling |
Structural |
Hispanics find it difficult to navigate online appointments and receive timely access |
Ability to Engage |
||
|
To provide an overview COVID-19 is detrimental for older Black and Hispanic adults |
Theoretical Overview |
Structural |
Identified structural racism in healthcare access and quality, e.g., Distribution of hospitals that are crowded |
Ability to Engage |
Personal Barriers
Both groups perceived a high risk of contracting the virus...A cross-sectional study consisting of Hispanic persons (n = 410) measured both perceived risk and precautionary behaviors (Karout et al., 2020). Hispanics (97.3%) felt they were at low risk for contracting the virus and therefore many did not wear masks (71.2%) or social distance (85.4%). In another study, however, Hispanic farm workers (n = 67) and nonfarm workers (n = 38) participated in a telephone survey that asked questions regarding their perceptions of severity, knowledge, self-efficacy, and preventive behaviors related to COVID-19 (Quandt et al., 2020). Both groups perceived a high risk of contracting the virus and practiced preventive behaviors, such as wearing masks. That said, neither group practiced social distancing according to public health recommendations; they continued to engage in large family gatherings. Researchers determined that this was most likely related to living accommodations, having extended family in close proximity, and cultural practices.
An online survey (n = 483) measured fear of contracting the virus, susceptibility, information seeking behaviors, knowledge, and self-efficacy (Roberts & David, 2021). The researchers found that the Hispanic group (n = 116) was less likely to fear the virus than NHWs and African Americans, resulting in less information seeking (Roberts & David, 2021). Another online survey investigating the probability of vaccination found that minority populations, including Hispanics (n = 241), who perceived a high risk of COVID-19 transmission were more likely to be vaccinated [95%, C.I., 1.07-1.22] (Reiter et al., 2020).
A qualitative study of Hispanics (total n = 60; women = 24) revealed a reluctance toward receiving care for fear of losing employment or even eviction (Cervantes et al., 2021). Undocumented Hispanics were specifically concerned with deportation. As a result, Hispanics who were unaware that they had virus were then unable to carry out recommended protocols such as self-quarantining or sheltering in place.
One physician reported to NBC that Hispanics’ skepticism was related to disinformationStigmatization or discriminatory experiences also prevent consumers from seeking care (Levesque et al., 2013). Mistrust is not a new phenomenon in minority populations, due to historical discriminatory experiences in healthcare (Reverby, 2009). One physician reported to NBC that Hispanics’ skepticism was related to disinformation (Sesin, 2020). Another study suggested that Hispanics must feel a sense of respect in order to share their needs with providers as they seek healthcare services during the pandemic (Reverby, 2021), a process that cannot happen without trust. Similarly, other researchers (Tai et al., 2021) found that disinformation exacerbates mistrust and increases the risks of contraction and transmission due to reluctance to seek care (e.g., COVID-19 testing).
...mistrust in healthcare leads to a reluctance to participate in interventions and treatments, such as the COVID-19 vaccinationLastly, mistrust in healthcare leads to a reluctance to participate in interventions and treatments, such as the COVID-19 vaccination (Allen et al., 2021). Researchers performed a data analysis from a larger study to investigate vaccine intentions. The sample (total n = 396, Hispanic n = 99) consisted of women aged 27-45. Of the respondents, 32.4% of Hispanic women reported that they would not be receiving the vaccine versus 15.4% of NHWs and 27.5% of non-Hispanic blacks. Researchers confirmed this reluctance was related to a mistrust of healthcare systems, political polarization around the pandemic, and disinformation.
Structural Barriers
Limited testing sites were a barrier to reaching, or accessing, COVID-19 testing. Initially, these tests were reserved for persons with symptoms only or who had traveled (Subbaraman, 2020). This directly affected minority populations, many of whom were essential workers and still working in-person, and delayed quarantining. In New York, testing accessibility was not proportional to need, and testing in white communities was greater than in minoritized communities (Lieberman-Cribbin et al., 2020). However, as awareness increased, organizations such as CVS, in collaboration with healthcare organizations and local groups, increased testing site accessibility (Graham, 2021).
Limited testing sites were a barrier to reaching, or accessing, COVID-19 testing.Because minority populations often obtain care from community clinics, the U.S. Department of Health Resources and Services Administration provided funding to sustain community clinics and implement COVID-19 testing and contact tracing (Romero et al., 2020). Another study on clinics, this one conducted in the state of Massachusetts, noted that testing sites and safety nets (e.g., hospitals and community clinics) were distributed in areas highly populated by minority communities, including Hispanics (Hu et al., 2020), which increased their ability to access testing services.
Despite these initiatives, not all minority populations were able to reach available care. Many of the community clinics and Federally Qualified Health Centers utilized by vulnerable populations closed during the start of the pandemic, delaying testing and primary healthcare (Thankur et al., 2020). Primary care began to transition to telehealth to provide services; digital literacy became an apparent barrier impacting vulnerable populations (Webb Hooper et al., 2020). One such example was shown in Ramirez et al. (2020), in a predominantly Hispanic town in Texas, where an otolaryngologist implemented telehealth in response to COVID-19 precautions. Of 270 total consults, 42 patients elected to use telehealth (of which 29 were Hispanics, or 69%). Compared to usage by the general population (92.4%), Hispanics’ use of telehealth was disproportionately low. The practice observed, in particular, lower rates of Hispanic men who accessed telehealth.
...Hispanics’ use of telehealth was disproportionately low. Limited technology accessibility also affected Hispanics living in rural areas. Eberly et al. (2020) noted that Hispanics with income less than $50,000 had lower rates of telemedicine use, presumably due to incurred costs from broadband, technology devices, and video access, resulting in an inability to pay for services.
Overcrowding was an additional barrier to healthcare engagement.Communication skills are necessary to engage in healthcare and participate in treatment decisions (Levesque et al., 2013). Expressing healthcare needs and receiving care without delay are important to receive effective services. However, initiatives to improve communication, such as telehealth and online portals, may hinder engagement. Four out of 10 persons found it difficult to navigate online appointments for vaccines, delaying access (Hamel et al., 2021). As far as quality, residential segregation determined the distribution of patients to hospitals that are overcrowded (Garcia et al., 2021). Overcrowding was an additional barrier to healthcare engagement.
Discussion
Intersection of Domains
Although the conceptual framework has been presented in a linear manner in the results described above, the domains are intersectional. For example, Levesque et al. (2013) stated that in order to perceive risk, one must also have knowledge and understanding of individual health status. The literature provides data linking knowledge to preventive behaviors that lower risk (Alsan, Stantcheva, Yang, & Cutler, 2020; Jones et al., 2020). For example, in a nationwide U.S. survey (n = 1435), Hispanics (n = 158, or 11%) were less likely to be aware of current COVID-19 cases and deaths (Jones et al., 2020). This might suggest a lack of knowledge and, therefore, lower risk perception. Similarly, in another web-based survey (n = 5198), Hispanics (n = 623, or 12%) demonstrated less knowledge about behaviors preventing transmission (Alsan et al., 2020); McCormack et al. (2021) also found that Hispanics (n = 123, or 12%) had significantly lower knowledge related to COVID-19, compared to NHWs. It is premature to conclude that risk perceptions in Hispanics are low without further investigating if the perceived risks of COVID-19 are directly associated with knowledge.
A shift in how healthcare information and services are delivered has resulted from the implementation of social distancing protocols.A shift in how healthcare information and services are delivered has resulted from the implementation of social distancing protocols. This may impact Hispanics’ ability to access COVID-19 health information and treatment. Digital health information, online scheduling for testing and appointments, and telehealth have become the new norm and Healthy People 2030 objectives include increasing the use of health information technology to allow consumers to track their health information and communicate with providers (Office of Disease Prevention and Health Promotion [ODPHP], n.d.). As this occurs, though, Hispanics are at a greater risk of not receiving healthcare services.
Hispanics’ low health literacy (LHL) levels have been well documented in the literature (Edward et al., 2018; Villagra et al., 2019). Persons with LHL needed greater assistance with online navigation and used the internet less often to seek health information related to COVID-19 (Vollbrecht et al., 2021). Since most COVID-19 information is found online, readability needs to be considered, particularly for populations with LHL and low English language proficiency. To assess this, researchers used four Readability Scales to evaluate 47 websites containing information related to COVID-19 (Valizadeh-Haghi, Khazaal, & Rahmatizadeh, 2021). They found that readability levels of content were close to high school and college levels, versus the recommended sixth-grade level. Understanding Hispanics’ barriers to care provides critical information needed to close knowledge and accessibility gaps.
Since most COVID-19 information is found online, readability needs to be considered...Another barrier faced by Hispanics was the wait time for in-person services. Overcrowding, as noted by Garcia et al. (2021), is an impediment to access. This overcrowding led to longer wait times, particularly for Hispanics using community clinics (Jha, Rav, & Epstein, 2011; Hoffman, Trawalter, Axt, & Oliver, 2016), which further limited their ability to engage.
Limitations
One limitation of this review was the low number of synthesized studies (n = 20). This small sample size could lead to biases, heterogeneity, and less robust results. Future research should include additional studies about Hispanics and COVID-19, as they are published during this unfolding situation.
Conclusion
During the pandemic, Hispanics faced increased risk because they often held essential jobs...Levesque et al.’s (2013) conceptual framework provided an opportunity to analyze access in a comprehensive manner, addressing multiple variables. The theoretical framework conceptualizes access to identify barriers to perceiving need, seeking, reaching, paying, and engaging in healthcare services. The framework’s multilevel approach considers factors on an individual level similar to health behavior models. The framework also addresses external factors, such as healthcare structures and social determinants that impede access to healthcare services that are similar to public health models. The framework in this context examined the barriers that U.S. Hispanics encounter in accessing healthcare during the COVID-19 pandemic, but can also be applied to the larger purpose of evaluating and eliminating disparities in access. Further research is needed on the associations between knowledge and perceived risks to better understand how to implement interventions for Hispanics related to both COVID-19 and general health.
Hispanics have a greater risk of contracting COVID-19 due to several determinants related to racial disparities. Hispanics have a higher prevalence of comorbidities, a result of disparities that existed long before the pandemic. The comorbidities are also associated with increased morbidity and mortality in COVID-19 (Baquero et al., 2020). During the pandemic, Hispanics faced increased risk because they often held essential jobs, limiting their ability to shelter in place, and they often live in multigenerational homes, making social distancing difficult (Kaur, 2020).
Efforts to increase access by providing more testing sites, telehealth services, and no-cost testing and vaccination have not resulted in improved health outcomes. Disinformation has prevented many Hispanics from accessing vaccinations. The disparities of COVID-19 have highlighted the importance of health information and how it is delivered: information needs to be accurate as well as culturally sensitive and linguistically appropriate to better reach Hispanic populations. Enhancing knowledge sharing in this way may improve perceived risks, resulting in behaviors that eliminate the contraction and transmission of COVID-19.
The disparities of COVID-19 have highlighted the importance of health information and how it is delivered...Developing a culturally sensitive and diverse nurse workforce may repair mistrust and lower reluctance to seek care, both during the pandemic and after it. Public health recommendations must be developed to be inclusive of underrepresented populations. For example, Hispanics are essential workers and often utilize public transportation. Therefore, sheltering in place and social distancing are not options. Culturally sensitive public recommendations may help increase U.S. Hispanics’ COVID-19 knowledge and encourage safe behaviors.
Funding
The author has not received any financial support for the research, authorship, and/or publication of this study.
Conflicts of Interest
The author declares that there is no conflict of interest related to the research, authorship, and/or publication of this study.
Author
MaryAnn Perez-Brescia, PhD, RN
Email: Maryann.brescia@uconn.edu
ORCID ID: 0000-0003-0606-1966
Dr. Perez-Brescia is a 2021 PhD graduate whose research focus is on health equity. She has been a nurse for over 30 years In a variety of roles, but most recent, she was appointed as the diversity, equity, and inclusion coordinator for the University of Connecticut School of Nursing. Dr. Perez-Brescia completed a diversity and inclusion certification from Cornell University to prepare her for this work. She hopes to continue to learn and develop her leadership skills to dismantle structural racism in academic settings and foster an inclusive and equitable environment that values diversity.
References
Aguayo-Mazzucato, C., Diaque, P., Hernandez, S., Rosas, S., Kostic, A., & Caballero, A. E. (2019). Understanding the growing epidemic of Type 2 Diabetes in the Hispanic population living in the United States. Diabetes/Metabolism Research and Reviews, 35(2), e3097. https://doi.org/10.1002/dmrr.3097
Allen, J. D., Abuelezam, N. N., Rose, R., & Fontenot, H. B. (2021). Factors associated with the intention to obtain a COVID-19 vaccine among a racially/ethnically diverse sample of women in the USA. Translational Behavioral Medicine, 11(3), 785–792. https://doi.org/10.1093/tbm/ibab014
Alsan, M., Stantcheva, S., Yang, D., & Cutler, D. (2020). Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. Journal of the American Medical Association Network Open, 3(6), e2012403. https://doi.org/10.1001/jamanetworkopen.2020.12403
Baquero, B., Gonzalez, C., Ramirez, M., Santos, E. C., & Ornelas, I. J. (2020). Understanding and addressing Latinx COVID-19 disparities in Washington state. Health Education & Behavior, 47(6), 845-849. https://doi.org/10.1177/1090198120963099
Berchick, E. R., Barnett, J. C., & Upton, R. D. (2019). Health insurance coverage in the United States: 2018 current population reports. United States Census Bureau. https://www.census.gov/content/dam/Census/library/publications/2019/demo/p60-267.pdf
Cennimo, D. J., Bergman, S. J., Olsen, K. M. (2021, June 25). How did the coronavirus outbreak start? News & perspective. https://medscape.com/answers/250014-197402/how-did-the-coronavirus-outbreak-start/
Centers for Disease Control and Prevention (CDC). (2022). COVID data tracker weekly review. Science. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
Cervantes, L., Martin, M., & Frank, M. G., Farfan, J. F., Kearns, M., Rubio, L. A., Tong, A., Gonzalez, A. M., Camacho, C., Collings, A., Mundo, W., Powe, N. R., & Fernandez, A. (2021). Experiences of Latinx individuals hospitalized for COVID-19: A qualitative study. Journal of the American Medical Association Open Network, 4(3), e210684. https://doi.org/10.1001/jamanetworkopen.2021.0684
Eberly, L. A., Kallan, M. J., Julien, H. M., Haynes, N., Khatana, S. A. M., Nathan, A. S., Snider, C., Chokshi, N. P., Eneanya, N. D., Takvorin, S. U., Anastos-Wallen, R., Chaiyachati, K., Ambrose, M., O’Quinn, R., Seigerman, M., Goldberg, L. R., Leri, D., Choi, K., Gitelman, Y… Adusumalli, S. (2020). Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. Journal of the American Medical Association Open Network, 3(12), e2031640. https://doi.org/10.1001/jamanetworkopen.2020.31640
Edward, J., Morris, S., Mataoui, F., Granberry, P., Williams, M. V., & Torres, I. (2018). The impact of health and health insurance literacy on access to care for Hispanic/Latino communities. Public Health Nursing, 35(3), 176–183. https://doi.org/10.1111/phn.12385
Garcia, M. A., Homan, P. A., García, C., & Brown, T. H. (2021). The color of COVID-19: Structural racism and the disproportionate impact of the pandemic on older Black and Latinx adults. The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences, 76(3), e75–e80. https://dx.doi.org/10.1093%2Fgeronb%2Fgbaa114
Garg, S., Kim, L., Whitaker, M., O’Halloran, A., Cummings, C., Holtein, R., Prill, M., Chai, S. J., Kirley, P. D., Alden, N. B., Kawasaki, B., Yousey-Hindes, K., Niccolai, L., Anderson, E. J., Openo, K. P., Weigel, A., Monroe, M. L., Ryan, P., Henderson, J….Fry, A. (2020). Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed Coronavirus Disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR: Morbidity and Mortality Weekly Report, 69(15), 458-464. https://doi.org/10.15585/mmwr.mm6915e3
Graham, G. (2021). Addressing the disproportionate impact of COVID-19 on communities of color. Journal of Racial and Ethnic Health Disparities, 8(2), 280–282. https://dx.doi.org/10.1007%2Fs40615-021-00989-7
Gross, C. P., Essien, U. R., Pasha, S., Gross, J. R., Wang, S., & Nunez-Smith, M. (2020). Racial and ethnic disparities in population level COVID-19 mortality. Journal of General Internal Medicine, 35(10), 3097-3099. https://dx.doi.org/10.1007%2Fs11606-020-06081-w
Hales, C. M., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2020). Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS: National Center for Health Statistics, 360. https://www.cdc.gov/nchs/products/databriefs/db360.htm
Hamel, L., Sparks, G., & Brodie, M. (2021). KFF COVID-19 vaccine monitor: Experiences with vaccine access and information needs. Polling. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-experiences-vaccine-access-information-needs/
Hoffman, K. M., Trawalter, S., Axt, J. R., & Oliver, M. N. (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences USA, 113(16), 4296-4301. https://doi.org/10.1073/pnas.1516047113
Hu, T., Yue, H., Wang, C., She, B., Ye, X., Liu, R., Zhu, X., Guan, W. W., & Bao, S. (2020). Racial segregation, testing site access, and COVID-19 incidence rate in Massachusetts, USA. International Journal of Environmental Research and Public Health, 17(24), 9528. https://doi.org/10.3390/ijerph17249528
Jha, A. K., Rav, E. J., & Epstein, A. M. (2011). Low-quality, high-cost hospitals, mainly in south, care for sharply higher shares of elderly black, Hispanic, and medicaid patients. Health Affairs, 30(10), 1904-1911. https://doi.org/10.1377/hlthaff.2011.0027
Jones, J., Sullivan, P. S., Sanchez, T. H., Guest, J. L., Hall, E. W., Luisi, N., Zlotorzynska, M., Wilde, G., Bradley, H., & Siegler, A. J. (2020). Similarities and differences in COVID-19 awareness, concern, and symptoms by race and ethnicity in the United States: Cross-sectional survey. Journal of Medical Internet Research, 22(7), e20001. https://doi.org/10.2196/20001
Karout, L., Serwat, A., El Mais, H., Kassab, M., Khalid, F., & Mercedes, B. R. (2020). COVID-19 prevalence, risk perceptions, and preventive behavior in asymptomatic Latino population: A cross-sectional study. Cureus, 12(9), e10707. https://doi.org/10.7759/cureus.10707
Kaur, H. (2020, August 20). These variables affect whether you live, die or get help during the pandemic. CNN. https://www.cnn.com/2020/08/20/us/systemic-racism-coronavirus-pandemic-trnd/index.html
Levesque, J. F., Harris, M. F., & Russell, G. (2013). Patient-centered access to health care: Conceptualising access at the interface of health systems and populations. International Journal for Equity in Health, 12, 18. https://doi.org/10.1186/1475-9276-12-18
Lieberman-Cribbin, W., Tuminello, S., Flores, R. M., & Taioli, E. (2020). Disparities in COVID-19 testing and positivity in New York City. American Journal of Preventative Medicine, 59(3), 326-332. https://doi.org/10.1016/j.amepre.2020.06.005
Manuel J. I. (2018). Racial/ethnic and gender disparities in health care use and access. Health Services Research, 53(3), 1407–1429. https://doi.org/10.1111/1475-6773.12705
McCormack, L. A., Squiers, L., Frasier, A. M., Lynch, M., Bann, C. M., & MacDonald, P. D. M. (2021 Feb. 18). Gaps in knowledge about COVID-19 among US residents early in the outbreak. Public Health Reports, 136(1), 107-116. https://doi.org/10.1177/0033354920970182
Moyce, S., Velazquez, M., Claudio, D., Thompson, S., Metcalf, M., Aghbashian, E., Vanderwood, K., & Sisson, N. (2021). Exploring a rural Latino community's perception of the COVID-19 pandemic. Ethnicity & Health, 26(1), 126–138. https://doi.org/10.1080/13557858.2020.1838456
Ngo Bikoko Piemeu, C. S., Loignon, C., Dionne, É., Paré-Plante, A. A., Haggerty, J., & Breton, M. (2021). Expectations and needs of socially vulnerable patients for navigational support of primary health care services. BMC Health Services Research, 21(1), 999. https://doi.org/10.1186/s12913-021-06811-8
Office of Disease Prevention and Heath Promotion (ODPHP). (n.d.). Health Communication. Healthy People 2030 Objectives and Data. Retrieved from https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-communication.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffman, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hrobjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S….Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. The BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
Pflugeisen, B. M., & Mou, J. (2021). Empiric evidence of ethnic disparities in coronavirus positivity in Washington State. Ethnicity & Health, 26(1), 36–48. https://doi.org/10.1080/13557858.2020.1863922
Quandt, S. A., LaMonto, N. J., Mora, D. C., Talton, J. W., Laurienti, P. J., & Arcury, T. A. (2020). COVID-19 Pandemic among Latinx farmworker and nonfarmworker families in North Carolina: Knowledge, risk perceptions, and preventive behaviors. International Journal of Environmental Research and Public Health, 17(16), 5786. https://doi.org/10.3390/ijerph17165786
Ramirez, A.V., Ojeaga, M., Espinoza, V., Hensler, B., & Honrubia, V. (2020). Telemedicine in minority and socioeconomically disadvantaged communities amidst COVID-19 pandemic. Otolaryngology Head and Neck Surgery, 164(1), 91-92. https://doi.org/10.1177/0194599820947667
Reiter, P. L., Pennell, M. L., & Katz, M. L. (2020). Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine, 38(42), 6500–6507. https://doi.org/10.1016/j.vaccine.2020.08.043
Reverby, S. M. (2009). Examining Tuskegee: The infamous syphilis study and its legacy. University of North Carolina Press. https://uncpress.org/book/9781469609720/examining-tuskegee/
Reverby, S. M. (2021). Racism, disease, and vaccine refusal: People of color are dying for access to COVID-19 vaccines. PLOS Biology, 19(3), e30001167. https://doi.org/10.1371/journal.pbio.3001167
Roberts, J. A., & David, M. E. (2021). The pandemic within a pandemic: Testing a sequential mediation model to better understand racial/ethnic disparities in COVID-19 preventive behavior. Healthcare, 9(2), 230. https://doi.org/10.3390/healthcare9020230
Romero, L., Pao, L. Z., Clark, H., Riley, C., Merali, S., Park, M., Egger, C., Campbell, S., Bui, C., Bolton, J., Le, X., Fanfair, R. N., Rose, M., Hinckley, A., & Siza, C. (2020, December 18). Health center testing for SARS-CoV-2 during the COVID-19 pandemic—United States, June 5-October 2, 2020. MMWR Morbidity and Mortality Weekly Report, 69(50), 1895–1901. http://dx.doi.org/10.15585/mmwr.mm6950a3
Sesin, C. (2020, December 20). Mistrust, disinformation among Latinos on Covid vaccine worries Hispanic doctors. NBC News, https://www.nbcnews.com/news/latino/mistrust-disinformation-among-latinos-covid-vaccine-worries-hispanic-doctors-n1251636
Sharma, R., Tinkler, S., Mitra, A., Pal, S., Susu-Mago, R., & Stano, M. (2018). State Medicaid fees and access to primary care physicians. Health Economics, 27(3), 629–636. https://doi.org/10.1002/hec.3591
Singh, K. A., & Wilk, A. S. (2019). Affordable Care Act Medicaid expansion and racial and ethnic disparities in access to primary care. Journal of Health Care for the Poor and Underserved, 30(4), 1543–1559. https://doi.org/10.1353/hpu.2019.0088
Spooner, C., Lewis, V., Scott, C., Dahrouge, S., Haggerty, J., Russell, G., Levesque, J. F., Dionne, E., Stocks, N., Harris, M. F., & IMPACT team. (2021). Improving access to primary health care: A cross-case comparison based on an a priori program theory. International Journal for Equity in Health, 20(1), 223. https://doi.org/10.1186/s12939-021-01508-0
Subbaraman, N. (2020). How to address the coronavirus's outsized toll on people of colour. Nature, 581(7809), 366–367. https://doi.org/10.1038/d41586-020-01470-x
Tai, D. B. G., Shah, A., Doubeni, C. A., Sia, I. G., & Wieland, M. L. (2021). The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clinical Infectious Diseases, 72(4), 703–706. https://doi.org/10.1093/cid/ciaa815
Thankur, N., Lovinsky-Desir, S., Bime, C., Wisnivesky, J. P., Celedon, J. C. (2020). The structural and social determinants of the racial/ethnic disparities in the U.S. COVID-19 pandemic. American Journal of Respiratory and Critical Care Medicine, 202(7), 943-949. https://doi.org/10.1164/rccm.202005-1523pp
U. S. Congress, 111th Congress. (2010). Patient Protection and Affordable Care Act, H. R. 3590, P/ L. 111-148. https://www.congress.gov/bill/111th-congress/house-bill/3590
Valizadeh-Haghi, S., Khazaal, Y., & Rahmatizadeh, S. (2021). Health websites on COVID-19: Are they readable and credible enough to help public self-care? Journal of the Medical Library Association, 109(1), 75-83. https://doi.org/10.5195/jmla.2021.1020
Villagra, V. G., Bhuva, B., Coman, E., Smith, D. O., & Fifield, J. (2019). Health insurance literacy: Disparities by race, ethnicity, and language preference. The American Journal of Managed Care, 25(3), e71–e75. https://pubmed.ncbi.nlm.nih.gov/30875174/
Vollbrecht, H., Arora, V. M., Otero, S., Carey, K.A., Meltzer, D.O., & Press, V. G. (2021). Measuring eHealth literacy in urban hospitalized patients: Implications for the post-COVID world. Journal of General Internal Medicine, 36(1), 251–253. https://doi.org/10.1007/s11606-020-06309-9
Webb Hooper, M., Napoles, A. M., & Perez-Stable, E. J. (2020). COVID-19 and racial/ethnic disparities. Journal of the American Medical Association, 32(24), 2466-2467. https://doi.org/10.1001/jama.2020.8598
Williams, R., Karuranga, S., Malanda, B., Saeedi, P., Basit, A., Besancon, S. Bommer, C., Esteghmati, A., Ogurtsova, K., Zhang, P., & Colagiuri, S. (2020). Global and regional estimates and projections of diabetes-related health expenditure: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Research and Clinical Practice, 162, e.108072. https://doi.org/10.1016/j.diabres.2020.108072
Yue, D., Rasmussen, P. W., & Ponce, N. A. (2018). Racial/ethnic differential effects of medicaid expansion on health care access. Health Services Research, 53(5), 3640–3656. https://doi.org/10.1111/1475-6773.12834
Zhao, B., Zhang, X., Huang, R., Yi, M., Dong, X., & Li, Z. (2021). Barriers to accessing internet-based home care for older patients: A qualitative study. BMC Geriatrics, 21(1), 565. https://doi.org/10.1186/s12877-021-02474-6


