In March 2020, COVID-19 cases were beginning to emerge in North Florida and concern over hospital bed capacity started to rise. Baptist Health System in Jacksonville, Florida quickly formed a multidisciplinary team to explore how we could increase hospital bed capacity. Utilizing the resources within our affiliated home healthcare agency, an Enhanced Home Support Model (EHSM) with a COVID-19 protocol was developed. The protocol was implemented by home health nurses and included COVID-19 testing, blood tests, and the ability to start oxygen at home on admission. Patients were provided self-monitoring equipment and information about self-isolating and infection control within the home. After the initial visit, the home health nurse and the primary care physician shared collaborative oversight through virtual visits. This article discusses how we initially approached identification of severity and the methods we used to implement the protocol. The results section offers information about the number of patients utilizing this protocol between April and December 2020; patient and physician satisfaction; and considers strengths and weaknesses of the program. In conclusion, the EHSM protocol allowed patients to receive high quality emergent care at home and increased access to hospital emergency departments and inpatient hospital beds for more seriously ill patients.
Key Words: COVID-19, home health nurses, hospital at home, hospital capacity, nurses, virtual healthcare visits, primary care providers
In March 2020...concern over hospital bed capacity started to rise. In March 2020, COVID-19 cases were beginning to emerge in North Florida and concern over hospital bed capacity started to rise. Using a combination of demographic and clinical data gathered from seven weeks of COVID-19 patient care early in the coronavirus pandemic, Johns Hopkins (2020) researchers published a “prediction model” that was used to help hospital-based providers care for COVID-19 patients and make important decisions about planning and resource allocations. The Johns Hopkins COVID-19 prediction model showed a surge of COVID-19 cases with an extreme shortage of hospital beds within the Jacksonville and surrounding areas (Johns Hopkins, 2020).
Baptist Health System has five hospitals and over 200 primary care physicians and specialists serving the 5-county area in Northeast Florida. To prepare for the predicted COVID-19 surge, we created a multidisciplinary team led by a doctorally-prepared Advanced Practice Registered Nurse (APRN). Our goal was to reduce utilization of hospital and emergency department services by safely managing patients in their homes under an Enhanced Home Support Model (EHSM). Caring for mildly ill patients in their homes opened hospital beds for the patients with more severe illness.
Our goal was to reduce utilization of hospital and emergency department services by safely managing patients in their homes...This article discusses how we initially approached identification of severity in the population of those diagnosed with COVID-19, and the methods we used to implement the protocol. The results section offers information about the number of patients utilizing this protocol between April and December 2020; patient and physician satisfaction; and considers strengths and weaknesses of the program.
Identification of Severity
Patients were initially identified by providers in the Baptist Primary Care (BPC) offices, using Centers for Disease Control and Prevention (CDC) Interim Guidance for Implementing Home Care of People Not Requiring Hospitalization for Coronavirus Disease 2019 (CDC, 2020). We identified patients who had a confirmed diagnosis or had symptoms consistent with COVID-19 infection and patients who were experiencing mild symptoms, such as myalgias, upper respiratory infection (URI), and low-grade fever. Primary care providers assessed patients utilizing telehealth technology via virtual visits, where the provider could see the patient over the phone or computer. Standard criteria were used to then develop a plan of treatment, depending on the severity of symptoms.
Patients with mild or no symptoms continued to be monitored by the provider. Patients with mild or no symptoms continued to be monitored by the provider. Patients with mild symptoms who needed further assessment were cared for in their homes under a specially designed program initiated by a set of standing orders. To enroll in the EHSM program, patients had to meet defined criteria. For example, they needed to have the ability to self-monitor, self-isolate, and have a caregiver who could provide food, over the counter medications, and transportation to the hospital in the event of clinical decline. Patients with serious coexisting medical conditions and or severe symptoms were referred to the Emergency Department (ED).
The EHSM program was considered successful, as evidenced by the number of patients who recovered in their homes, even though many required supplemental oxygen. The program was expanded; patients were referred to the program from the ED and hospital. This further opened beds for more seriously ill patients.
Methods
Brief Overview of Procedure
The COVID-19 Enhanced Home Support Model of care was developed by physicians from BPC, with collaboration from risk management and legal experts and leadership in the home health and hospital settings. The EHSM included a physician standing order set, (see Figure 1), utilization of telehealth technology, and immediate access to in home oxygen. A key component of the EHSM was the close collaboration between the primary care provider, the patient, and the home healthcare clinician.
A key component of the EHSM was the close collaboration...Development of standing orders streamlined care and prevented home health nurses from waiting for orders or clarification of orders. The order set was approved by the BPC Medical Director and could be initiated by any BPC provider. All BPC providers and Baptist Home Health Care (BHHC) staff were provided copies and educated about the standing orders and the processes and procedures to implement the protocol. BPC had an order selection in the electronic medical record (EMR) to “Initiate the COVID-19 Protocol/Order set.” BHHC had the order set built into the EMR for clinicians to follow. BHHC clinicians and office staff had a copy with the BPC Chief Medical Officer’s signature. This copy allowed them to enter the patient oxygen saturation, liters needed to maintain 92% oxygen saturation (SaO2) and the order was sent to durable medical equipment company to deliver an oxygen concentrator.
Figure 1.
Enhanced Home Health Standing Orders: Referral from Primary Care for Patients with Confirmed/Suspected COVID-19 Disease
|
Oxygen: If O2 sat <92%, start O2 on patient and titrate LPM to maintain O2 sat >92% not to exceed 3 LPM via nasal cannula at rest.
Start of Care Labs:
Repeat Labs:
Skilled Nurse: Daily x5 consecutive days (to be re-evaluated on a regular cadence by physician) via virtual or in home visits for assessment and vital signs, then every other day for an additional 5 days, 3 PRN visits for troubleshooting worsening symptoms and vital signs, call primary care physician for further orders.
Medications and Other Standing Orders:
Patient Education:
|
Legend: FLU/RSV-Influenza/Respiratory syncytial virus, PCP-Primary Care Provider, PRN-As needed, PO-by mouth, SOB-Short of breath. (Used with Permission of Baptist Health)
Initiation of EHSM Protocol
Once BHHC received the order, a call was made to the patient to assess his or her condition, verify the address, screen for technology capabilities, and determine personal protective equipment (PPE) needs. A nurse was deployed to the home within 4 hours, with a portable oxygen cylinder, and a COVID kit for patient self-monitoring, which contained a pulse oximeter, thermometer, blood pressure cuff, incentive spirometer, lab supplies and infection control information. Patients were tested for COVID and influenza (FLU) if this had not already been done. A complete blood count with differential (CBC with diff) and a basic metabolic panel (BMP) were obtained on the first visit and 48 hours later. If the patient had an SaO2 less than 92%, oxygen was initiated and titrated to 5 Liters Per Minute (LPM) to maintain above 92% Sa02. The order was revised to change the maximum amount of oxygen a patient could have in the home from 5 liters per minute to 3 liters per minute. If the patient needed more than 3 LPM they were required to go to the hospital. We found that patient’s clinical condition could quickly deteriorate and felt the hospital was the best place for them if they were requiring so much oxygen.
If patients were not able to maintain Sa02 above 92% the primary care provider was notified and they were referred to the ED.If patients were not able to maintain Sa02 above 92% the primary care provider was notified and they were referred to the ED. The most common symptom in patients with COVID is dyspnea, which is often accompanied by hypoxemia. Patients frequently require supplemental oxygen and close monitoring (National Institutes of Health [NIH], 2021). Patients were taught to self-monitor oxygen levels and to notify BHHC and physician if they fell below the established parameters. Patients were assessed and instructed on the process for virtual visits. If they were not capable of virtual visits the BHHC, nurse would make a home visit. Patients were educated about the importance of self-care; rest; hydration treatment for fever; and aches and pains and the use of over-the-counter medications that have shown to be effective to treat symptoms related to COVID-19 (Harvard Health Publishing, 2022).
Follow Up and Monitoring
The provider and the home health nurse collaborated and communicated very closely...The COVID-19 protocol allowed for both virtual or in-home visits, or either, providing flexibility for patient needs. Patients were followed by the BHHC virtual nurse team daily for five days and then every other day. The BPC provider did a virtual visit every other day unless the patient condition required more frequent visits. The provider and the home health nurse collaborated and communicated very closely to ensure that the plan of treatment was adjusted to address the patient’s condition. Most patients were covered under the EHSM protocol and did not require adjustments to the plan of treatment. Patients received an in-home discharge visit to ensure long-term stability.
Results
Patients were placed on a tracking spreadsheet at the time of the referral which was then frequently updated with data regarding use of oxygen, COVID test results, ED and hospitalizations. The first patient was admitted on April 4, 2020. A total of 530 patients were admitted into BHHC COVID-19 EHSM from April to December 31, 2020. There was a significant spike during the month of July 2020; this was thought to be a result of social gatherings that occurred over the Independence Day holiday on July 4.
As the volume of COVID positive patients increased, we utilized other local home healthcare agencies...As the volume of COVID positive patients increased, we utilized other local home healthcare agencies to provide care using the same protocol. Data from BHHC patients only are included in Figure 2 below which shows the number of admissions by month from April through December. Relevant patient data that depict COVID-19 status, oxygen use, and hospitalizations are shown in Figure 3. The hospitalization rate for patients under the program was 9%, and re-hospitalization rate was 3%, significantly lower than the national average of 20% re-hospitalization for patients in home healthcare.
Figure 2.
Number of Symptomatic Patients Admitted to Home Health under EHSM COVID Protocol
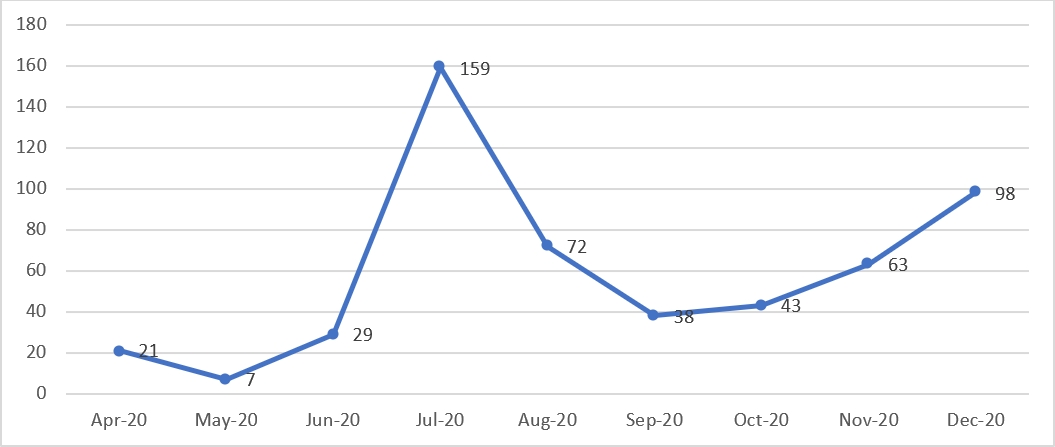
Figure 3.
Relevant Patient Data
|
COVID-19 Status |
# % |
|
Positive |
460 (87%) |
|
Negative |
36 (7%) |
|
Unconfirmed |
34 (6%) |
|
Oxygen Use |
|
|
Started on oxygen in the home |
116 (22%) |
|
Came from the hospital on oxygen |
48 (9%) |
|
Already on oxygen in the home (CHF/COPD) |
15 (3%) |
|
Higher Level of Care |
|
|
Used Emergency Department* |
28 (5%) |
|
Hospitalized* |
47 (9%) |
|
Rehospitalized* |
17 (3%) |
| *While under care of the BHHC not claims data |
|
Patient and Physician Satisfaction
...the program was very well received by patients and providers.We conducted a patient and physician satisfaction survey early in the program, in August 2020. Forty patients participated in the survey and 100% agreed or strongly agreed that having a home healthcare nurse improved their COVID-19 condition; 97.5% agreed or strongly agreed that the BHHC nurse worked well with BPC providers. The average score for other questions asked (e.g., patients agreed the Home Health Nurse understood their needs and problems, were timely in addressing their problems, and the nurse helped them understand their plan of care) was a positive 95%. Collaborating physicians were asked if the EHSM was a valuable program for the care of patients with COVID-19 and 100% agreed or strongly agreed. In sum, the program was very well received by patients and providers.
EHSM Program Strengths and Weaknesses
Multidisciplinary collaboration was a strength of this program.Multidisciplinary collaboration was a strength of this program. Development and implementation of the EHSM included collaboration from leadership in settings of primary care; hospital and EDs; home health agencies; durable medical equipment companies, with input from legal and risk management experts and representatives from pharmacies, discharge planning, information systems, and education departments. Meetings were held weekly with subgroups convening even more frequently. Processes and protocol went through many revisions. The protocol was considered a living document, with the goal and ability to revise as new knowledge and experience were gained. The time frame for protocol development was short; however, the urgency to help the health system gain capacity was felt by all members. Thus, the program was given a priority focus.
Federal legislation that addressed the pandemic was also an advantage.Federal legislation that addressed the pandemic was also an advantage. The Coronavirus Aid, Relief and Economic Security (CARES) Act (2020) relaxed regulations that allowed this program to be successful. Several examples of this flexibility include establishing a lower Sa02 requirement to qualify for oxygen; allowing transport of oxygen cylinders by nurses; permitting nurse practitioners to write home care orders; allowing reimbursement for telehealth visits; and providing funds for personal protective equipment (AANP, 2020).
Protocols which required manual labor...impacted the efficiency of this new program...Protocols which required manual labor, such as data collection and oxygen delivery, impacted the efficiency of this new program, as well as increasing demand and existing insurance policies. For example, manual data collection relied on communication from home health clinicians, patients, and inpatient case managers to track ED visits, re-hospitalizations, and discharge information. We also tracked oxygen use manually. Oxygen transportation was limited to office to patient home and back; therefore, if patients did not need oxygen it had to be brought back to the office. When capacity was met at BHHC other agencies required education about the protocol, which used the resource of time. Insurance authorization was a barrier to 4-hour admission for some agencies and insurances.
Conclusion
The EHSM was effective in reducing patient flow and admissions in EDs and hospitals, opening beds for more seriously ill patients. Primary care providers were able to care for patients with the ability for patients to self-monitor using equipment delivered to their home. Between April and December 2020, 530 mildly ill patients were cared for in their homes without requiring them to leave and potentially expose others in the community.
Telehealth visits increased the capacity of the home health agency, and thus the capacity of hospital beds.Telehealth visits increased the capacity of the home health agency, and thus the capacity of hospital beds. Virtual visits also decreased the use of scarce PPE and decreased healthcare provider exposure. Established standing order protocols that reflected multidisciplinary collaboration and increased authority for nurses offered safety and efficiency. This program provided a foundation for effective use that extends beyond the COVID-19 pandemic. For example, the ability to care for patients in their homes and prevent ED or hospital visits might be expanded for patients with congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) in their homes using a similar model to hopefully achieve similar positive outcomes.
Author
Lisa Kidd MSN, RN, NEA-BC
Email: n00117505@unf.edu
Lisa is currently enrolled in the Doctor of Nursing Practice/Family Nurse Practitioner Program at the University of North Florida in Jacksonville Florida. She obtained a Master of Science in Nursing from Jacksonville University in 2013 and a Bachelor of Science in Nursing from University of North Florida in 1989. Lisa is Nurse Executive Advanced Board Certified by the American Nurses Credentialing Center. She is a member of Sigma Theta Tau National Honor Society, American Nurses Association, and a recipient of Northeast Florida Great 100 Nurses Award. Lisa is currently the Area Director for Baptist Home Health Care by Bayada, a recently formed joint venture between Baptist Health System and Bayada Home Health Care. Prior to the joint venture she served as the Administrator for Baptist Home Health Care and has worked in the home health department at Baptist for 28 years. Lisa works very closely with the Transition Care department within the Baptist 5 Hospital Health System and the Baptist Primary Care Providers, to provide patients with the highest quality care in the most appropriate level of care. A major focus is the implementation of programs that prevent or shorten hospitalizations.
References
American Association of Nurse Practitioners (AANP). (2020, March 27). NP applauds President Trump on signing of CARES Act. AANP News. https://www.aanp.org/news-feed/aanp-applauds-president-trump-on-signing-of-cares-act
Centers of Disease Control and Prevention (CDC). (2020, October 16). Interim guidance for implementing home care of people not requiring hospitalization for coronavirus disease 2019 (COVID-19). Healthcare Workers. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-home-care.html
Harvard Health Publishing. (2022, January 31) Treatments for COVID-19: What helps, what doesn’t, and what’s in the pipeline. COVID-19 Updates. https://www.health.harvard.edu/diseases-and-conditions/treatments-for-covid-19
Johns Hopkins Medicine Newsroom. (2020, September 23). Johns Hopkins researchers publish COVID-19 ‘prediction model’. News Releases. https://www.hopkinsmedicine.org/news/newsroom/news-releases/johns-hopkins-researchers-publish-covid-19-prediction-model
National Institute of Health (NIH). (2021, December 16). Oxygenation and ventilation. COVID-19 Treatment Guidelines, Management. https://www.covid19treatmentguidelines.nih.gov/management/critical-care/oxygenation-and-ventilation
U. S. Congress, 116th. (2020). Coronavirus Aid, Relief, and Economic Security (CARES) Act, Public Law 116-136, 134 STAT 281. https://www.congress.gov/116/plaws/publ136/PLAW-116publ136.pdf

