Health disparities increasingly impact African Americans (AAs). An individual’s perception is a significant predictor of health. This exploratory research study aimed to identify perceptions of health among AA males in a barbershop setting. The Duke Health Profile-8 and a demographic questionnaire were utilized. Data were analyzed using SPSS for descriptive statistics, multiple regression, and correlational analyses. The number of health conditions negatively correlated with physical, perceived, and overall health. Education level was positively correlated with mental health. Mental health scores were higher among those who were married. Identifying perceptions of health can help healthcare providers create tailored interventions to reduce risk factors and improve health outcomes.
Key Words: African Americans, males, perceptions, health, health disparities, barbershop, nursing
African American (AA) men experience some of the highest morbidity and mortality rates in the United States. Nearly 40% of AA males over the age of 20 are obese, and 40.5% have hypertension (CDC, 2020). In 2018, diabetes rates were notably higher at 13.4%, and AA males experienced more diabetes-related deaths than any other ethnicity (CDC, 2020). This group has the highest death rates from diabetes,AAs (AA) men experience some of the highest morbidity and mortality rates in the United States. heart disease, cancer, hepatitis, human immunodeficiency virus (HIV), and stroke (USDHHS, 2020). They are particularly vulnerable to untreated mental health issues, with their suicide rate being four times higher than that of AA females in 2017 (USDHHS, 2020). AA males often arrive at the emergency room in critical condition more often than other men. Moreover, they are less likely to have health insurance or attend regular healthcare provider appointments (Stewart et al., 2019).
The World Health Organization (WHO, 2020) defines health as complete physical, mental, and social well-being, not merely the absence of disease or infirmity. One’s perception of health can influence overall well-being and health outcomes. Healthy People 2030 has identified factors determining an individual's health (Determinants of Health). These determinants are organized into five key domains: (1) Economic Stability, (2) Education Access and Quality, (3) Health Care Access and Quality, (4) Neighborhood and Built Environment, and (5) Social and Community Context (Healthy People, 2030). AAss are disproportionately and negatively affected by factors described in these domains. The rates are so alarming that more research and initiatives are needed to improve health among AA males.
Purpose
While motivation is essential for behavior change, researchers have discovered that another critical factor is people’s mindsets (Martinovich, 2017). Perceptions play a significant role in predicting health outcomes. Furthermore, an individual’s definition of health is an important criterion. Since perceptions vary based on life experiences, exploring this area may provide researchers with insights to help develop intervention strategies. As noted by the American Thoracic Society (2007), health perceptions (or perceived health status) are subjective evaluations. Some individuals may view themselves as healthy despite having one or more chronic diseases, while others may see themselves as unwell without any evidence of disease.
In a concept analysis of perception, McDonald (2012) concluded that an individual's perceptions can be a powerful force for action. Perception represents an individual’s way of viewing a phenomenon and involves life experiences. Therefore, it is important for healthcare providers to explore what influences perceptions to develop strategies to impact health. An understanding of individuals’ perceptions of health may provide key information to drive strategies for intervention. Therefore, this study aimed to assess AA males’ perceptions of health in a community setting. This information will assist in identifying disease risks and potential for engaging in healthy behaviors.
Literature Review
Health Perceptions
Multiple models exist to provide insight into the construct of health perceptions. Diamond and colleagues (2007) developed and tested a scale to measure adult health perceptions that could be applied in various settings. This 15-item scale was created to offer a reliable measure of beliefs that did not concentrate on a specific diagnosis but could be relevant to several conceptual models used with adults experiencing chronic conditions. The scale was administered to four groups of adults (322 participants) in different environments to assess its psychometric characteristics. The authors state that their overall aim of creating an internally consistent instrument for evaluating perceptions of health and wellness was accomplished, and the scale can serve as a tool in research to measure personal beliefs about health (Diamond et al., 2007).
A qualitative study of AA men's perceptions of health and health influences, using focus groups led by Ravenell et al. (2006), indicated that their definition of health aligns with the World Health Organization’s definition. This study, which involved 71 AA men, identified health maintenance strategies such as lifestyle changes, stress management, healthy prayer, seeking medical care, self-empowerment, and social support. Stress within this population was attributed to a lack of income, experiences of racism, "unhealthy" neighborhoods, and conflicts in relationships. Positive health influences included social support and the participants’ perceived link between unemployment and poor health. The men also recognized self-empowerment through education and communication as a crucial health maintenance strategy (Ravenell et al. 2006).
Using data from three national surveys (the National Health Interview Survey, the National Health and Nutrition Examination Survey, and the National Death Index) involving 61,141 adults, Zahrt and Crum (2017) discovered that health outcomes are influenced by perceptions of health behaviors. Participants who perceived themselves as less active than individuals of their age experienced a 71% higher mortality rate compared to those who viewed themselves as more active. Even after the researchers accounted for various factors (activity data, sociodemographic variables, health status, and other health behaviors), the results were consistent. The importance of accurate perceptions of health based on health status has also been investigated. In a study with 1289 adults, self-perceptions of health were assessed by asking, “Would you say that, in general, your health is” poor, fair, good, very good, excellent, don’t know, and no response (Dalbo et al., 2017, p. 1 ). This investigation found that people have misperceptions of their health based on the standard definitions of health. This disconnect in the understanding of health is concerning. The researchers identified a contributing factor, which may be that individuals who are at risk for disease or have been diagnosed with a disease perceive themselves to be healthy and, as a result, do not comprehend the need to modify lifestyle factors that would improve health.
Barriers
Watson (2014) conducted a qualitative study involving 37 young AA males through focus groups to identify the barriers they face in accessing health care. Three primary themes emerged from the study. These themes pertained to community and environmental factors, financial constraints, and mistrust of the medical system. Among the community and environmental issues were unhealthy living conditions, substance abuse, and negative peer influences. Many participants reported experiencing significant health issues before seeking medical care. They also conveyed how costly it was to attain and maintain good health, which was beyond their means. Furthermore, they postponed treatment due to a lack of trust in healthcare providers.
In another study, Webb et al. (2019) explored AAs perceptions of health research, their participation in research, and their willingness to participate in research compared to disadvantaged Caucasians. The study included 7,809 participants, with nearly 42% being male. Almost 60% of participants rated their health as either excellent or good. AAs were less likely to have participated in research, volunteered for research, or expressed a willingness to participate in research within the coming year. They also reported a mistrust of research and researchers and a preference for higher research compensation. AA males aged 65 and older with health insurance, rated their health as excellent or good, were married, and had less than a 12th-grade education reported a decreased interest in participating in any upcoming research. Those who had seen a doctor in the past 12 months or visited the emergency room, were unemployed, experienced food insecurity, and had participated in research before were more likely to engage in additional research. Overall, AAs were less willing to participate in research due to mistrust.
Disparities also exist for AAs regarding disabilities. According to the CDC (2020), 53 million Americans live with functional disabilities. A disability refers to any condition that makes it more challenging for someone to engage in activities and interact with others. One in four AAs has a disability. Nuru-Jeter et al. (2011) examined black-white disparities across various disability outcomes throughout the lifespan. The study aimed to investigate black-white differences in daily living activities, functional limitations, sensory impairments, and memory issues. The data for this research, sourced from the 2006 American Community Survey, included a sample of 2,288,800 individuals representing both community-dwelling and institutionalized populations. Black individuals faced higher odds of disability throughout their lifespan compared to white individuals. Furthermore, black-white differences in all disability outcomes were most pronounced in midlife (ages 50–69) and began to narrow in the mid-80s. The authors emphasize the need to address black-white disparities across a range of disability outcomes over the lifespan and suggest future research to identify the factors contributing to this pattern of disparities.
The intersection of physical wellness, emotional wellness, and overall wellness is another area of interest. In a study by McNeish et al. (2021), the emotional and physical health of AA males in relation to their overall health was investigated. The emotional and physical health of 115 AA males was assessed using a 15-item Wellness Self-Perception Questionnaire. Emotional wellness was defined as an individual's ability to cope with daily circumstances, while physical wellness was defined as an individual's capacity to function effectively. Of the 115 study participants, the majority reported a positive perception of their overall wellness. Education emerged as an important factor influencing emotional, physical, and overall wellness. Interestingly, men with higher average incomes reported lower overall wellness compared to those with lower incomes. Finally, both physical and emotional wellness were identified as predictors of overall wellness.
Methods
A descriptive research design was used to explore perceptions of health in AA males. The study utilized data collected from survey questionnaires from 100 participants. Participants were recruited using informational flyers and convenience sampling at a barbershop that predominantly serves AA males in the Southwest U.S. Participants were eligible for the study if they met the following criteria: (1) were able to speak, understand, and read English; (2) read and sign informed consent; (3) complete all research instruments; (4) self-identified as AA; and (5) at least 18 years old.
Human Subjects Protection
Approval was obtained from the University’s Institutional Review Board (IRB) for the Protection of Human Subjects. Permission to utilize the Duke Health Profile-8 (Duke-8) research instrument was granted. Finally, the researchers received approval from the data collection site. Written informed consent was secured from all participants. The risks associated with participating in this study were minimal and included feelings of apprehension regarding the content of the questionnaires and concerns that responses would be shared with others. The principal investigator (PI) was the only individual with access to the data stored in a locked file cabinet in the PI’s office. After completing the study questionnaires, participants were given a $10.00 gift card as compensation for their time.
Measurements
Two instruments were utilized in the data collection process: a demographic questionnaire and the Duke Health Profile-8 (Duke-8). Completing both questionnaires took approximately 10 to 15 minutes.
Demographic Questionnaire. The demographic questionnaire included 11 questions aimed at gathering standard characteristics of the participants. The questions focused on age, gender, ethnicity, marital status, education level, number of individuals in the household, annual household income, date of the last medical check-up, diagnosed medical conditions, and occupation. One additional item asked participants to rate their overall health as excellent, good, or poor.
Duke Health Profile-8. The Duke Health Profile-8 (Duke-8) consists of eight self-report items. This instrument is a shortened version of earlier iterations that initially included 63 items (Duke Health Profile) and then 17 items (Duke 17), developed by Duke University in North Carolina and the University of North Carolina School of Public Health to measure patient-reported quality of life or functional health status. The instrument can be utilized with any population. The reliability and validity of the original scale were assessed by facilities affiliated with Duke University Medical Center and have been demonstrated in subsequent studies. Internal consistency for each item scale was measured using Cronbach’s alpha, with reliability coefficients around 0.70 (Parkerson, 2002). Research studies approved by the IRB are currently underway to validate the Duke Health Profile-8 items. The Duke-8 can be self-administered or completed in an interview style. Each of the eight questions offers three possible responses, which are rated 0, 1, or 2. The subscale measures include a Physical Health Score, Mental Health Score, Social Health Score, Perceived Health Score, and Disability Score. An overall health score can also be calculated. Responses to the items in each measure are summed, and the means of the raw scores are normalized to a scale from 0 (worst health status) to 100 (best health status) for each subscale.
Data Analysis
Data analysis was conducted using SPSS version 25.0 for Windows. Descriptive statistics summarized the demographic characteristics. Additionally, multiple regression and correlation analyses were used to examine the relationships between selected characteristics, self-reported health ratings, and the Duke-8.
Results
Demographic Questionnaire
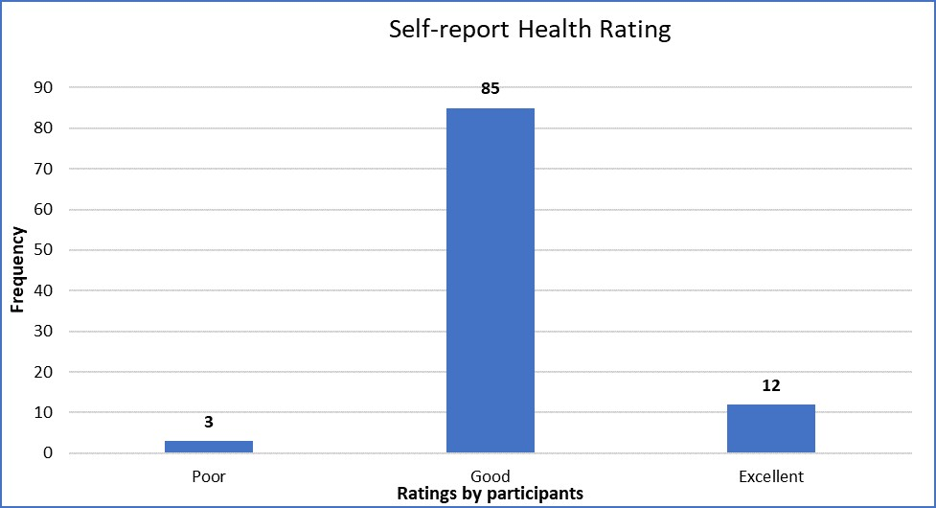
The ages of the 100 AA male participants ranged from 19 to 69 years (Mean = 35.53). Less than half (41%) were married, and 98% had completed high school or obtained additional higher education (see Table 1). Most participants were employed in various occupations, and the mean annual income exceeded $50,000. As shown in Figure 1, the most commonly reported medical conditions were high blood pressure, asthma, and diabetes. Participants reported varying lengths of time for visits to healthcare providers, with the longest reported timeframe being 37 years. A large majority (73%) of participants lived with other household members, while only 27% reported living alone. The overwhelming majority of participants rated their self-health as good (85%). Only three percent of participants gave a poor self-health rating (Figure 2).
Table 1. Participant Characteristics
|
Criterion |
Frequency |
Percentage |
|---|---|---|
|
Age (Mean = 35.53%) |
|
|
|
Marital Status |
|
|
|
Income |
|
|
|
Education Level |
|
|
Duke-8
The mean scores for the subscales of the Duke-8 ranged from 72.5 to 94 and are detailed in Table 2. The mean Physical Health Score was 82.75, indicating difficulty walking and general pain. The mean Mental Health Score was 84.0, reflecting the individual’s concentration and emotional state. The mean Social Health Score was 85.50, which indicates socialization. The mean Disability Score was 94.0, indicative of reasons why participants stayed home. The lowest mean score among participants was the Perceived Health Score, which reflected how participants perceived their general health at 72.50. The mean Overall Health Score obtained from the Duke-8 was 83.88.
Table 2. Duke Health Profile-8 Mean Scores
|
Scale |
Mean Score |
SD (+/-) |
|---|---|---|
|
Physical Health Score |
82.75 |
20.0 |
|
Mental Health Score |
84.00 |
20.57 |
|
Social Health Score |
85.50 |
18.86 |
|
Perceived Health Score |
72.50 |
26.94 |
|
Disability Score |
94.00 |
19.17 |
|
Overall Health Score |
83.88 |
10.56 |
Figure 1. Reported Health Conditions
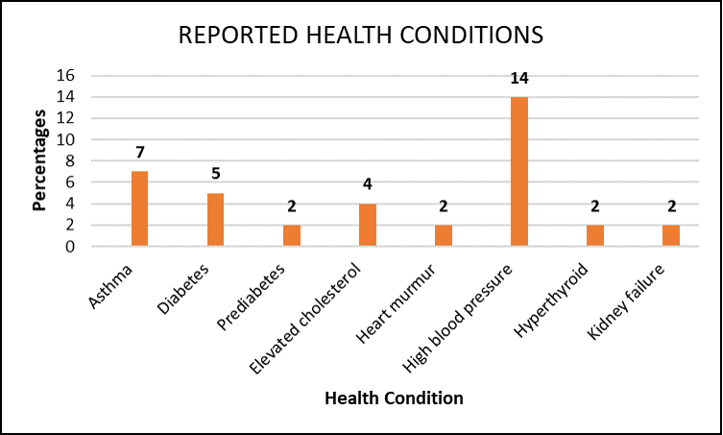
Perceived health was positively correlated with physical health. The number of health conditions was negatively associated with physical health, perceived health, and overall health. Education level was positively correlated with mental health. Married individuals had higher mental health scores than those who were unmarried. Overall health was positively correlated with physical health, mental health, and social health.
Figure 2. Self-report Health Rating
Discussion
This study explored health perceptions in AA males. Since the Duke-8 is very brief, it can be used to assess areas that may need to be addressed quickly by healthcare providers. By using the overall score and then reviewing each subscale, healthcare providers can identify areas that may require interventions. Scores reflect not only perceived health but also the best health status and functioning.
The mean scores for Physical Health (82.75) and Mental Health (84.0) were more closely aligned. Only four participants reported being unemployed, so it is understandable that the physical score would be relatively good. Many participants were employed, which can support general mental wellness. While four participants listed unemployment, another eleven did not specify an occupation. Most participants had completed high school and/or some additional advanced education, which aligns with findings reported by McNeish et al. (2021) that education impacts physical and mental health.
The mean Social Health Score of 85.5 also indicates good social support. Forty-one percent of participants in this study were married, which may provide social support. In addition, the participants were in a barbershop, which often provided a sense of community, social interaction, and support.
The highest mean score for disability was 94. This relatively high score may be due to participant characteristics reported. None of the participants reported any disability related to mobility, so this score reflects that response. This finding is not reflective of the CDC statistics, which report that 1 in 4 AAs have a functional disability. The location of the study may have also played a factor, as the participants were actively mobile and out in a community setting and possibly did not perceive any disability.
The lowest mean score was 72.5, which was represented by the Perceived Health Score. This may be explained by half of the participants (50%) reporting a medical condition, which could have factored into their overall perceived assessment. Dalbo et al. (2017) found that people misperceive their health based on the standard definitions of health. In contrast, the participants in this study reflect an awareness of the relationship between disease conditions and health status.
The mean Overall Health Score on the Duke-8 more accurately reflected the percentage of participants who self-reported their health rating. Among the self-reported health ratings, 85% of participants described their health as good. Sixty-six percent of participants in this study had attended college or completed a graduate degree, and their mean income exceeded $50,000 per year, which may have influenced the health ratings. The findings related to education level were consistent with those reported by McNeish et al. (2021); however, the findings regarding income differed.
Findings regarding education level were similar to those reported by McNeish et al. (2021). Like this study, McNeish found that having a high school diploma, some college education, or a four-year college degree predicted better overall health reports. McNeish et al. (2021) reported that an income of $20,000 to $ 29,999 predicted worse overall health. This finding was similiar to this study where the mean income greater than $50,000 participants reflected a good overall health rating.
Limitations
The study had several limitations, including being conducted in one location and represented one ethnic group; subsequently, the findings cannot be generalized to other ethnic groups. Participants had the option to leave items blank if they felt uncomfortable disclosing certain information. The instruments did not gather additional details that could influence individual perceptions of health, such as experiences of discrimination, the use of prescription or non-prescription medications, family history, and personal definitions of health. Furthermore, no objective measures of health status were collected, including height, weight, body mass index, blood pressure, heart rate, and oxygen saturation.The data relied on self-reports, and participants may not have provided accurate responses due to discomfort in sharing their answers with researchers.
Implications for Future Practice
A better understanding of AA males’ perceptions of health can help healthcare providers identify areas for intervention and patient education. First, hospital nurses can develop care plans tailored to the AA male perspective to promote positive health outcomes. Employers should commit to nursing continuing professional development (NCPD) activities, such as in-services, workshops, and regular updates, focused on AA health. Second, community nurses can use this information to quickly assess educational needs. Lastly, nursing curricula should include AA health issues. This knowledge will enable culturally competent nurses to empower AA males to engage in a healthier lifestyle. A better understanding of AA males’ perceptions of health can help healthcare providers identify areas for intervention and patient education.
AAs have higher rates of hypertension, diabetes, and end-stage renal disease. These rates may be attributed to perceptions of health. Ongoing research in this area may identify perceptions about health and barriers that prevent AA males from leading a healthy lifestyle. Given the rising rates of chronic disease among AAs, identifying opportunities to promote education and reach individuals is essential. The barbershop serves as a vital community space for health promotion and prevention. Introducing health education to community venues such as barbershops provides an innovative approach to positively impacting underserved communities.
Conclusion
Due to the lack of participation among AAs in research, it is crucial for healthcare providers to actively recruit AA males for studies. Their perspectives are essential for developing culturally specific interventions and enhancing positive experiences. The The barbershop serves as an ideal setting for conducting research and promoting health to address health disparities. significant evidence of health disparities in the U.S., particularly among AAs, compels healthcare workers to investigate various factors that can influence health. It's important to understand how socioeconomic status intersects with health impacts. Nurses have a duty, as healthcare providers, to create educational materials, culturally relevant interventions, and community engagement activities. Barbershops play a vital role in the AA community, serving as one of the few safe spaces where AA males can gather without feeling threatened. They provide an environment for discussing relevant issues and exchanging information in a real-world context. The barbershop serves as an ideal setting for conducting research and promoting health to address health disparities. Engaging with this population should not be confined to acute care settings but should also extend into the community. Further research is recommended to continuously assess the health perceptions of AA males, with the goal of building trust, reducing health disparities, and improving overall health outcomes.
Acknowledgments
The researchers would like to thank the university for supporting and encouraging the advancing of scientific knowledge and to the barbershop patrons, barbers, and proprietor of the barbershop, for their time in participating in research to advance knowledge.
Authors
Glenda Daniels, PhD, RN, CNS, CGRN, CWOCN
Email: glenda.daniels@tcu.edu
ORCID ID: 0000-0003-4420-8287
Glenda Daniels, PhD, RN, CNS, CGRN, CWOCN, is a Professor of Nursing at Texas Christian University, Harris College of Nursing & Health Sciences, Fort Worth, Texas. She received her BSN from The University of Texas, Austin, MSN from Texas Woman’s University, and PhD from the University of Texas at Arlington. Her research focus includes improving outcomes in the gastrointestinal setting, increasing knowledge about kidney disease and colorectal cancer screening, and health promotion.
Janie R. Robinson, PhD, RN, CNE
Email: janie.r.robinson@tcu.edu
ORCID ID: 0000-0001-6093-3118
Janie R. Robinson, PhD, RN, CNE, is a registered nurse, certified nurse educator, and CPR instructor. She is a Professor of Nursing at Texas Christian University, Harris College of Nursing & Health Sciences. She obtained her Bachelor of Science in Nursing (BSN), MSN, and PhD from Southern University and A & M College in Baton Rouge, Louisiana. Her research focus is health disparities in African Americans.
References
American Thoracic Society. (2007). Health status, health perceptions. https://qol.thoracic.org/sections/key-concepts/health-status-health-perceptions.html
Centers for Disease Control and Prevention. (2020). National Center for Health Statistics: Health of Black or African American non-Hispanic Population. https://www.cdc.gov/nchs/fastats/black-health.htm
Dalbo, V. J., Teramoto, M., Roberts, M. D., & Scanlan, A. (2017). Lack of reality: Positive self-perceptions of health in the presence of disease. Sports, 5(2), 1-9. https://doi.org/10.3390/sports5020023
Diamond, J. J., Becker, J. A., Arenson, C. A., Chambers, C. V., & Rosenthal, M. P. (2007). Development of a scale to measure adults’ perceptions of health: Preliminary findings. Journal of Community Psychology, 35(5), 557-561. https://doi.org/10.1002/jcop.20211
Healthy People 2030. (n.d.). Determinants of health. Retrieved from https://health.gov/healthypeople/objectives-and-data/social-determinants-health
Martinovich, M. (2017, May 18). How your perception of health may extend your life. Stanford Graduate School of Business. https://www.gsb.stanford.edu/insights/how-your-perception-health-may-extend-your-life
McDonald, S. M. (2012). Perception: A concept analysis. International Journal of Nursing Knowledge, 23(1), 2-9. https://doi.org/10.1111/j.2047-3095.2012.01127.x
McNeish, R., Simmons, C., Watson, J., & Tran, Q. (2021). Perceptions of emotional and physical wellness among African American men as predictors of perceived overall health. Ethnicity & Health, 26(4), 600-613. https://doi.org/10.1080/13557858.2018.1530738
Nuru-Jeter, A. M., Thorpe, R. J., & Fuller-Thomson, E. (2011). Black-White differences in self-reported disability outcomes in the U.S.: Early childhood to older adulthood. Public Health Reports, 126, 834-843. https://doi.org/10.1177/003335491112600604
Parkerson, G. R. (2002). User’s guide for Duke health measures. Department of Community and Family Medicine, Duke University Medical Center.
Ravenell, J. E., Johnson, W. E., & Whitaker, E. E. (2006). African-American men’s perceptions of health: A focus group study. Journal of the National Medical Association, 98(4), 544-550. https://doi.org/10.1016/S0027-9684(15)31461-X
Stewart, K., Ristvedt, S., Brown, K. M., Waters, E. A., Trinkaus, K., McCray, N., & James, A. S. (2019). Giving voice to Black men: Guidance for increasing the likelihood of having a usual source of care. American Journal of Men’s Health, 13(5), 1-11. https://doi.org/10.1177/1557988319856738
U.S. Department of Health and Human Services, Office of Minority Health. (2020). Diabetes and African Americans. https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=61
Watson, J. (2014). Young African American males: Barriers to access to health care. Journal of Human Behavior in the Social Environment, 24(8), 1004-1009. https://doi.org/10.1080/10911359.2014.953416
Webb, F. J., Khubchandani, J., Striley, C. W., & Cottler, L. B. (2019). Black-White differences in willingness to participate and perceptions about health research: Results from the population-based HealthStreet study. Journal of Immigrant and Minority Health, 21(2), 299-305. https://doi.org/10.1007/s10903-018-0729-2
World Health Organization. (2020). Frequently asked questions. https://www.who.int/about/who-we-are/frequently-asked-questions
Zahrt, O. H., & Crum, A. J. (2017). Perceived physical activity and mortality: Evidence from three nationally representative U.S. samples. Health Psychology, 36(11), 1017-1025. https://doi.org/10.1037/hea0000531


