Precision Health (PH), a novel approach to care provision, tailors medical decisions, interventions, and treatments to an individual's uniqueness by recognizing individual variations in genes, environment, and lifestyle. Although the implementation of PH is proliferating, there is currently no clear shared understanding of it among practicing Registered Nurses (RNs). This descriptive cross-sectional study assesses nursing’s capacity to integrate PH into practice through a survey examining knowledge, skills, and attitudes (KSAs) in a sample of RNs. Pilot testing of the Precision Health Nurse Capacity Scale (PHNCS) was aimed at determining its utility in assessing nurses' capacity for PH. Results indicate that nurses favor PH and that the PHNCS is a valid and reliable tool. Knowledge gains will be deployed in a nationwide survey of nurses in which the aim is to measure the capacity of the nursing workforce for both PH and genetics/genomics.
Key Words: Competencies, capacity, workforce, KSA, Genomics, Genetics, Wearables, Direct-to-consumer testing (DTCT), Social Determinants of Health (SDoH), Health Literacy, Biomarkers, omics
Precision Health (PH), an emergent phenomenon, takes a holistic approach to wellness and medical care, considering many characteristics of the individual seeking care. Precision Health (PH), an emergent phenomenon, takes a holistic approach to wellness and medical care, considering many characteristics of the individual seeking care. Cognizant of variations in genes, environment, health literacy, and lifestyle on an individual’s health outcomes, PH integrates various omics information, including genomic, proteomics, metabolomics, and microbiomics, alongside clinical data to enable personalized disease diagnosis, treatment, and prevention strategies (Ginsburg & Phillips, 2018; National Research Council, 2011).
Although the adoption, hence the visibility, of PH by institutions and individual providers is rising steeply, a shared understanding of what constitutes good practice or defined competencies is needed. The training nurses receive in PH varies widely across nursing programs and health organizations, leading to a vague understanding of what PH is, often blurring it with only the more familiar concepts and skills from genomics.
Existing literature on workforce capabilities in PH often focuses on specific subsets of care, such as genetics and genomics (Calzone et al., 2011), or specific skill sets, such as direct-to-consumer testing (DTCT) (McGrath et al., 2019). Additionally, previous literature has explored competencies in related fields, such as pharmacogenetics for pharmacists (Formea et al., 2018), radiology education with AI integration (Duong et al., 2019), and genetics and genomics for advanced practice nurses (Flowers et al., 2019). However, these studies fail to comprehensively address the baseline PH capacity of a workforce or how to integrate PH competencies into practice. This study seeks to fill that gap by surveying the capacity of a sample of Registered Nurses (RNs) to integrate PH KSAs into their practice.
This pilot study had two purposes. First, to assess the capacity of a sample of nurses to integrate precision health (PH) competencies into their practice. Second, to evaluate an investigator-developed instrument–the Precision Health Nurse Capacity Scale (PHNCS)--for its suitability in making such an assessment.
Background
The concept of PH is rooted in the Human Genome Project (2003), which provided a comprehensive map of the human genome and deepened our understanding of genetic factors contributing to diseases. Since then, research in PH has expanded with new discoveries and advancements in innovative technology and increased access to patient health data, often through giant data sets from an institution’s Electronic Medical Record, or EMR. PH has evolved from the concept of Precision Medicine (PM), formerly known as personalized medicine, by incorporating omics data and considering broader factors such as lifestyle, social determinants, economic factors, cultural influences, and environmental considerations (Fu et al., 2020). The concept of PH is rooted in the Human Genome Project (2003), which provided a comprehensive map of the human genomeData analytics derived from these enormous data sets enable optimizing disease diagnosis, treatment, and prevention strategies tailored to each patient's needs. By integrating omic information into precise care, healthcare professionals gain a holistic understanding of an individual's biological makeup and their encompassing genetic, molecular, and microbial factors. This comprehensive approach allows for personalized interventions that optimize disease diagnosis, treatment selection, and prevention strategies, ultimately aiming to provide precise, customized care that maximizes therapeutic efficacy and improves overall health outcomes.
Despite the potential of PH to improve care processes and outcomes, its practical application in nursing practice remains a challenge. Nurses' training and education in PH vary widely across nursing programs and health organizations, hindering the widespread implementation of PH principles in patient care. Standardized education and integrating PH competencies into nursing practice are essential for providing high-quality, personalized care—the type of care the profession has discussed for decades.
Nurse leaders are responsible for providing the necessary education and training for their workforce to apply this knowledge of omic data, SDoH, and other factors that contribute to the well-being and health of individuals. Incorporating PH principles into nursing education, including the social drivers of health, lifestyle factors, comorbidities, biomarkers, socioeconomic status, health literacy, and genetic and other omic factors, enables practitioners to effectively contribute to personalized, precise care and improved health outcomes. Additionally, ongoing professional development programs are crucial to keep nurses updated with the latest advancements and practices in the rapidly evolving field of PH. Our workforce must be ready to participate in population-based screening, targeted treatment interventions, DTCT, and other healthcare initiatives that may have a significant impact on the health of patients and populations.
Methods
Design
A cross-sectional descriptive design with convenience sampling was used to report levels (or relevance) of PH KSAs perceived by practicing nurses. Ethics approval from a university was obtained prior to data collection (IRB Approval-IRB-FY2023-169). The IRB approval and study materials were sent to four institutions in anticipation of the participation of their nurse employees.
Sampling
The target population for this pilot study is practicing RNs from across the United States. For convenience sampling, RNs working in four institutions where investigators work in four different states, California, Alabama, Pennsylvania, and New Jersey were chosen. These four sites represent varied RN experiences in PH from small community settings to large medical centers located in urban, rural, or metropolitan areas.
Instrument
The PHNCS questionnaire comprises nine Likert-scale items formatted in a matrix-style surveyThe PHNCS questionnaire comprised of nine Likert-scale items formatted in a matrix-style survey (See Figure 1). These matrices were purposefully designed to align with the five domains of the familiar, person-centered nursing process: assessment, diagnosis, planning, implementation, and evaluation. These domains highlight the KSAs nurses must possess to execute their roles and responsibilities regarding this novel approach to highly individualized and data-based care.
Three of the nine questions, 1, 8, and 9, have a five-point Likert scale with scores ranging from 1 = very important to 5 = not at all important. These questions relate to the nurses’ knowledge of PH principles. Questions 2, 3, 4, and 5 have a three-point Likert scale with scores ranging from 1 = advantageous to 3 = not advantageous. These items seek the nurses’ beliefs on the benefits of PH in their practice, while Question 7, using the same three-point Likert scale, queries the nurses’ beliefs on PH integration to the patient’s care plan. Lastly, question 6, another three-point Likert scale (1 = confident and 3 = not confident), explores the nurses’ confidence in using non-traditional diagnostic procedures in providing more personalized care.
Figure 1. The Precision Health Nurse Capacity Scale
The PHNCS is categorized following the nursing process domains (assessment, diagnosis, planning, intervention, and evaluation).
ASSESSMENT: The following questions are related to the nurse’s role in the systematic collection of information from/about the client.
|
1. How important do you think it is for a nurse to become more educated about the following in order to provide highly individualized care? |
|
|
Social Determinants of Health |
|
|
Direct-to-Consumer Tests |
|
|
Wearables |
|
|
Health literacy |
|
|
2. Indicate whether you think each of the following would benefit by integrating assessments of Social Determinants of Health into your practice. |
|||
|
|
Advantageous |
Not sure |
Not advantageous |
|
Understanding of an individual’s wellness history |
|
|
|
|
Understanding of individual’s potential lifestyle risk factors |
|
|
|
|
Understanding of how to help the individual |
|
|
|
|
Providing better treatment |
|
|
|
|
Understanding of individual’s barriers to wellness |
|
|
|
|
3. Indicate whether you think each of the following would benefit by integrating assessments of other diagnostic procedures such as wearables into your practice. |
|||
|
|
Advantageous |
Not sure |
Not advantageous |
|
Understanding of an individual’s wellness history |
|
|
|
|
Understanding of individual’s potential lifestyle risk factors |
|
|
|
|
Understanding of how to help the individual |
|
|
|
|
Providing better treatment |
|
|
|
|
4. Please indicate whether you think each of the following would benefit by integrating assessment of other diagnostic procedures such as direct-to-consumer test kits into your practice. |
|||
|
|
Advantageous |
Not Sure |
Not advantageous |
|
Understanding of an individual’s wellness history |
|
|
|
|
Understanding of individual’s potential lifestyle risk factors |
|
|
|
|
Understanding of how to help the individual |
|
|
|
|
Providing better treatment |
|
|
|
|
5. Please indicate whether you think each of the following would benefit by integrating the assessment of an individual’s health literacy into your practice. |
|||
|
|
Advantageous |
Not Sure |
Not advantageous |
|
Evaluate health literacy and its relation to the general well-being of a person and the community |
|
|
|
|
Describe the importance of health literacy in achieving optimum wellness. |
|
|
|
DIAGNOSIS: The following questions are related to the nurse’s role in clinical judgment to the client’s potential or actual health conditions.
|
6. Each of the following statements relates to other diagnostic procedures that can be available to achieve precision health. By incorporating this diagnostic information, healthcare professionals are able to have more information that can inform their decisions in prescribing preventative measures and treatments. Please indicate how confident you are to do each of the following: |
|||
|
|
Confident |
Not sure |
Not confident |
|
Administration and interpretation of germline testing |
|
|
|
|
Administration and interpretation of genomic and biomarker testing. |
|
|
|
|
Interpretation of Direct-to-Consumer (DTC) testing e.g., 23andme |
|
|
|
|
Assessment and interpretation of other wearables such as Fitbit, iPhone watch, implantable cardioverter defibrillators, etc. |
|
|
|
|
Using Electronic Health Record (EHR) in documenting diagnostic assessments |
|
|
|
|
Use of resources to explore information or interpretation of the data. |
|
|
|
|
Advocating the use of precision health diagnostics |
|
|
|
PLANNING: The following questions are related to the client's plan of care developed by nurses.
|
7. Please indicate whether you agree or disagree with the following statements. |
|||
|
|
Agree |
Don’t know |
Disagree |
|
Formulate a plan of care respectful to patient’s rights including in the provision of informed consent. |
|
|
|
|
Formulate a plan of care inclusive of the client’s environmental, cultural, religious, gender, and ethnic perspectives. |
|
|
|
|
Formulate a plan of care addressing the Social Determinants of Health |
|
|
|
|
Develop a plan of care with consideration to potential psychological and emotional impact from health information discovered from the client and other diagnostic findings affecting the individual and/or other family members. |
|
|
|
|
Develop a plan utilizing best practices in precision medicine or precision health |
|
|
|
INTERVENTIONS: The following questions are related to the nurse’s role in the implementation of nursing care.
|
8. Thinking about how nurses support clinical decisions by way of those interventions, how important do you think each of the following should be performed by nurses? |
|
|
Familiarize oneself by learning and applying basic concepts and skills related to precision health/precision medicine and genomics. |
|
|
Provide education for clients relative to precise care that promotes better lifestyle and health choices based on remotely acquired data (i.e., wearables) |
|
|
Discern risks versus benefits when implementing precision health activities, e.g., accessing and using the patient portal as it relates to client privacy and confidentiality |
|
|
Use patient information to develop highly personalized health care plans that aim to improve health care outcomes |
|
|
Refer clients to appropriate resources for precision health such as interpreting genetic results, advising for treatment options, and consulting with social support organizations that can assist with social determinants of health. |
|
|
Collaborate with other health professionals (such as physicians, pharmacists, genetic counselors, and social workers) to provide a comprehensive plan of care based on the individual’s data |
|
EVALUATION: The following questions are related to the nurse’s role in the continuous assessment and modifications of the plan of care.
|
9. In providing continuous quality care to patients how important are the following for nurses to perform? |
|
|
Reflect and evaluate one’s own beliefs and biases to achieve highly individualized care for health, wellness, and improved outcomes for clients and their families. |
|
|
Evaluate and improve the plan of care by giving full consideration to the client’s Social Determinants of Health. |
|
|
Evaluate and modify the plan of care by utilizing Precision Medicine/Precision Health advances (such as wearables). |
|
|
Evaluate and improve the plan of care by utilizing genomic information. |
|
|
Evaluate the plan of care to optimize the client's and their families’ health literacy. |
|
Data Collection and Analysis
The consent and the survey were sent to practicing registered nurses via email after permission of the facilities’ IRB and nursing leaders were obtained electronically. The respondents completed the survey online and submitted it anonymously to a password-protected cloud folder. The data and the reliability of the scale were analyzed using SPSS version 27.
Results
The demographics of the study participants were not collected. Instead, the descriptors of the nursing workforce for both of the participating institutions are reported in the aggregate. One group of participants worked at a large academic medical center in the eastern part of the United States that employs 3,555 RNs. This group consisted of primarily female (86%) nurses who are predominantly prepared at the baccalaureate and master levels (94.46%). Most nurses (70%) reported their ethnicity as White/not Hispanic or Latino, with the second most frequent category (12%) being Asian, not Hispanic/Latino. The RNs ranged in age from 22-77 years old, with an average age of 38.2 years.
In contrast, most practicing nurse respondents are employed at a local community hospital or regional medical center while also teaching at a public university Department of Nursing (DON). Their demographics represent a more diverse group of nurses, with (36.3%) Caucasians, (20.5%) Asians, (20.5%) Hispanics, (13.6%) African-Americans, and (9%) categorized as “other”. They are primarily females (79.54%) with age distribution ranges from 30 to over 70 years old and an average age of 51. Most nurses (79.5%) were prepared at the graduate and doctoral levels.
Frequencies
Findings show that most nurse respondents, 84.6%-96.15%, felt it is essential for nurses to be educated about social determinants of health (SDOH), DTCT, wearables, and health literacy to provide highly individualized care – Precision Health (Table 1). Most respondents (92.31% to 96.15%) feel it is advantageous for nurses to assess a person’s SDOH to understand their wellness history, potential lifestyle risk factors, means of helping the individual, and provide better treatment (Table 2). Many of the respondents consider the integration of assessments from wearables as a positive contributor to a nurse’s understanding of a patient’s wellness history (73.08%), potential lifestyle risk factors (80.77%), and in the provision of appropriate nursing interventions (80.77%) and better treatment (88.46%) (Table 3).
Table 1. Importance of Establishing Nurses’ Knowledge and Competencies with Precision Health

Note. Social Determinants of Health (SDoH), Direct-to-Consumer Tests (DTC), Wearables (W), Health literacy (HL).
Table 2. Importance of Understanding SDoH in PH
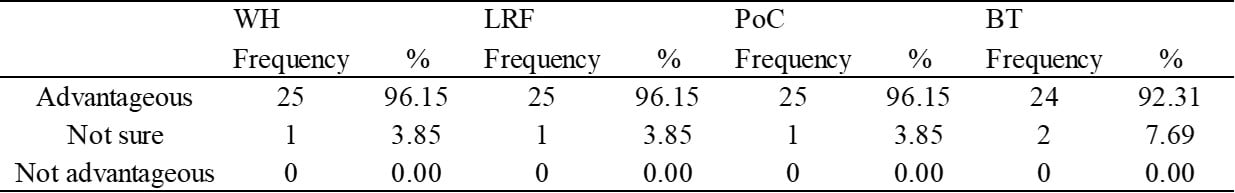
Note. Wellness history (WH), Lifestyle Risk Factors (LRF), Plan of Care (PoC), and Better Treatment (BT)
Table 3. Importance and Utility of Wearables in Precision Health
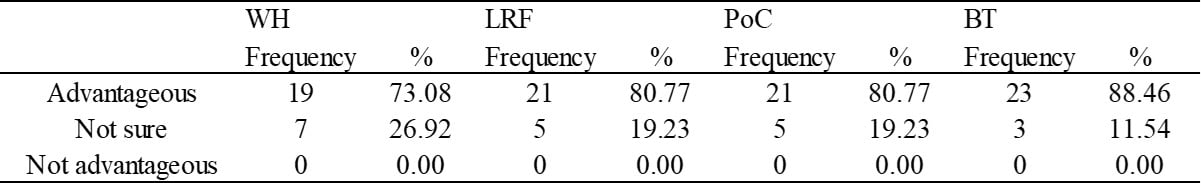
Note. Wellness history (WH), Lifestyle Risk Factors (LRF), Plan of Care (PoC), and Better Treatment (BT).
Further, most respondents consider the integration of assessments from DTCT as a positive contributor to a nurse’s understanding of a patient’s wellness history (69.23%), potential lifestyle risk factors (73.08%), and in the provision of appropriate nursing interventions (73.08%) and better treatment (80.77%) (Table 4). Many respondents reported that they favored an evaluation of the patient’s health literacy as a contributor to the person’s general well-being and optimal wellness (92.31%) (Table 5).
Table 4. Importance and Utility of Non-Traditional Diagnostic Tests in Precision Health
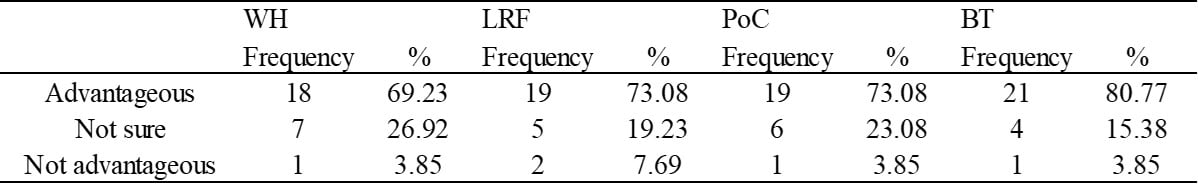
Note. Wellness history (WH), Lifestyle Risk Factors (LRF), Plan of Care (PoC), Better Treatment (BT).
Table 5. Importance of Patient’s Health Literacy Relative To Individual Well-Being
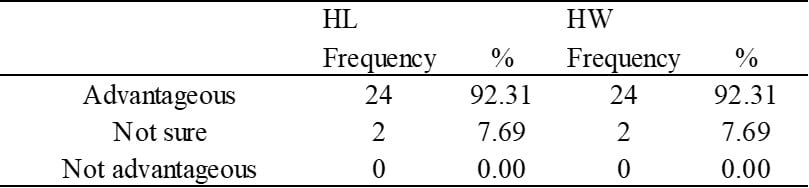
Note. Health Literacy (HL), Health and Wellness (HW).
In reporting about self-confidence in the use of non-traditional diagnostic tests, many of the respondents did not express confidence in administering and interpreting germline testing (15.38%), genomic and biomarker testing (23.07%), DTCT results (34.62%), and other wearables (50%) (Table 6). However, the vast majority of respondents expressed confidence in documenting diagnostic assessments within the EHR (92.31%), a smaller majority (76.92%) expressed confidence with the use of resources to explore information or interpret data, and a minority of respondents (46.15%) were confident in advocating for the use of PH diagnostics. Table 7 shows the percentage of respondents affirming statements related to the formulation of a precise plan of care that is: respectful of the patient’s rights (88.46%), inclusive of a client’s perspectives (84.62%), and of the patient’s SDOH (84.62%), considerate to potential psychological and emotional impact from health information discovery (88.46%), and intentional to development of a plan reflecting best practices in Precision Medicine or PH (88.46%).
Table 6. Confidence in Non-Traditional Diagnostic Procedures
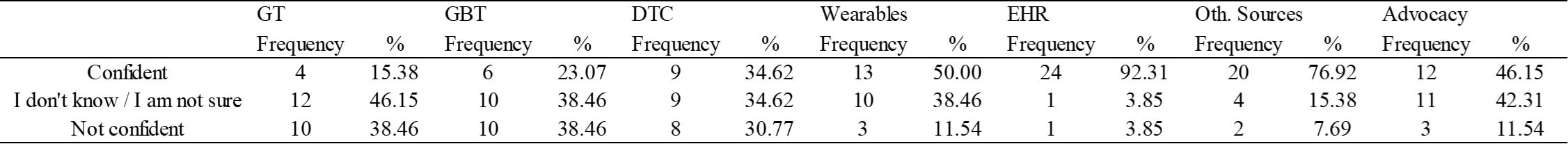
Note. Germline Testing (GT), Genomic and biomarker testing (GBT), Direct-to-Consumer (DTC), Electronic Health Record (EHR), and other sources of data (Oth. Sources).
Table 7. Affirmation Statements When Designing a Plan of Care
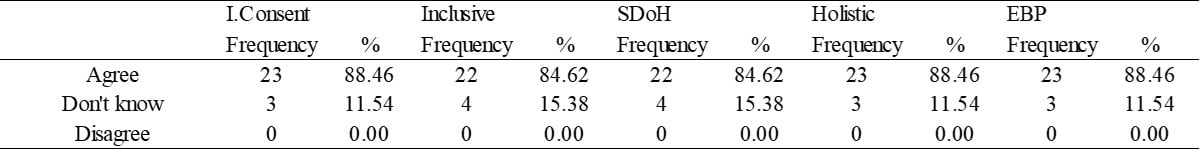
Note. Informed Consent (I.Consent), Inclusive plan of care (Inclusive), Social Determinants of Health (SDoH), and Evidence-Based Practices (EBP)
Regarding the knowledge and skills necessary to implement precise nursing care, respondents affirmed the importance of the need for possession of basic PH principles (96.15%), the provision of precise patient education based on individual lifestyle and remotely-acquired data (96.15%), discernment of risks versus benefits in implementation of precise health activities, (96.15%), use of patient information to develop highly-personalized health plans (96.15%), patient referral to resources such as genetic counseling (96.15%), and collaboration with all health professionals to develop a precise plan of care (96.15%) (Table 8). In the evaluation of patient care, Table 9, notes that many respondents considered these factors to be very or somewhat important to the continuous quality of care: reflection on one’s own beliefs (92.3%), plan improvement based on significant consideration of the patient’s SDOH (96.15%), plan modification based on advances in Precision Medicine (92.3%), modification of a plan based on genomics (78.46%), and evaluation of the plan of care aimed at building health literacy (96.15%).
Table 8. Importance of PH in Nursing Interventions
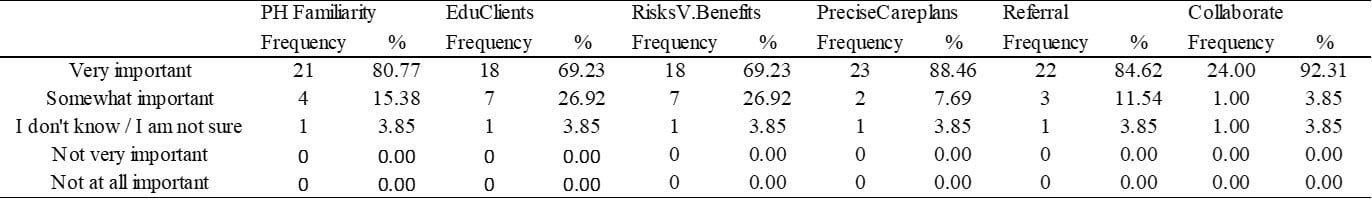
Note. Precision Health (PH), education for clients (EduClients), risks versus benefits (RisksV.Benefits)
Table 9. Importance of Precision Health in the Evaluation of Care
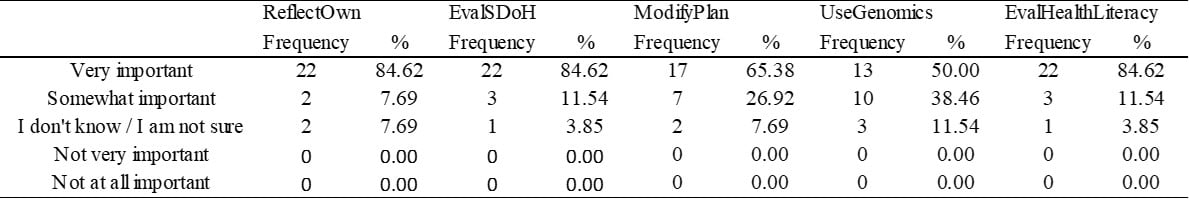
Note. Reflect own beliefs (ReflectOwn), evaluate Social Determinants of Health (EvalSDoH),
Validity & Reliability of the Scale
A team of experts drafted the survey questions based on a preliminary set of competencies developed by a Work Group convened by the American Nurses Association (ANA). These competencies were written in concert with practicing nurse experts in various areas of expertise within PH.
To establish face validity, the lead investigators presented the items and their scales to three practicing PH nurse experts. The items were read to them on a virtual call at which time, feedback on the relevance, wording, and timeliness of each item was received.
These three experts are employed in institutions known for innovations in personalized care. One is a Clinical Nurse Specialist in Gastrointestinal Oncology in one of our nation’s premier medical centers. Another is an Associate Professor in Nursing Informatics at a school affiliated with a well-known academic medical center. The remaining expert is a staff nurse and manager in inpatient oncology at a large medical center.
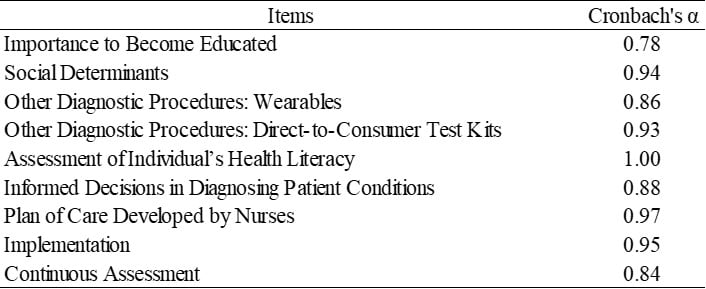
The reliability of the scale was established, using Cronbach’s alpha. Scores ranged from 0.78 to 0.97 which demonstrated strong measures of reliability (see Table 10).
Table 10. Reliability of Precision Health Nurse Capacity Scale (PHNCS)
Correlations
Correlations demonstrate relationships amongst variables. In this study, findings showed moderate to strong correlations between the importance for nurses to become educated with SDOH (0.73**) and the implementation (0.70**) and evaluation of patient care (0.68**). Assessment of SDOH suggested a strong relationship between nursing interventions (0.75**) and evaluation of the patient’s plan of care (0.69**). The plan of care developed by nurses revealed a strong relationship with the implementation of nursing interventions (0.70**) and evaluation of patient care (0.83**). These relationships are depicted in Table 11.
Table 11. Correlations
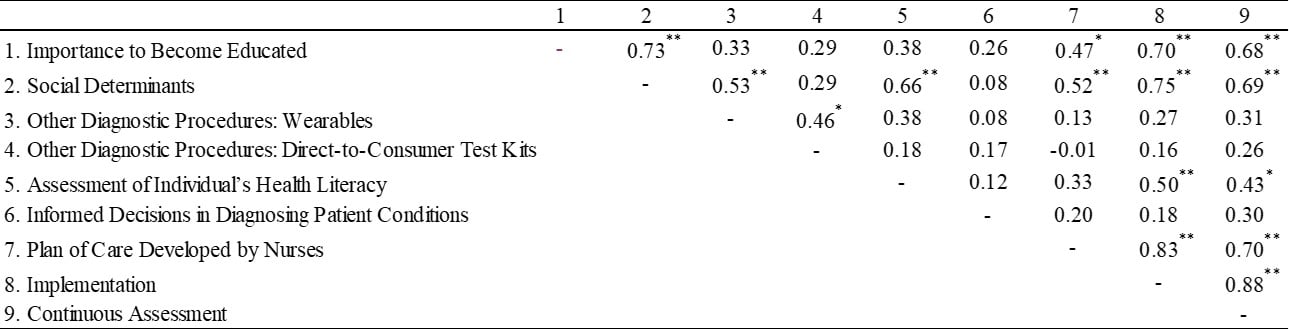
Note. ** p < 0.01, * p < 0.05.
Discussion
Nurses responding to the pilot study overwhelmingly agreed that the workforce must be prepared to assess individual-level patient data derived from histories, laboratory results, genetic/genomic testing, and environments. They also supported the incorporation of genetic/genomic data, health histories, and data sourced from wearable devices into patient diagnoses, care planning, and interventions. Many of the nurses believed that social determinants of health (including issues of gender, culture & ethnicity, environment, & religious beliefs), along with the assessment of lifestyle risk factors, play key roles in the individualized planning of nursing interventions that meet patients’ individual needs and improve patient outcomes. They also agreed that assessing patient health literacy levels impacts patient outcomes and patient/family teaching, and should play a role in the nurse’s planning, interventions, and evaluation of outcomes.
A number of nurses had less confidence in their ability to administer and interpret results from diagnostic procedures such as germline and biomarker testing, although they felt competent to incorporate the results into patients’ electronic medical records. Their lower confidence in interpreting the results of PH diagnostics impacts their ability to advocate for the use of these non-traditional diagnostic tools that can better contribute to a holistic plan of care.
Despite the nurses’ beliefs that the KSAs identified are critical in providing precise care, their confidence in integrating diagnostics and interventions to adopt these practices is lacking. Therefore, nursing needs to teach these essential skills as the fundamental step in the full adoption of PH. A set of competencies, also lacking, is needed to guide nurse educators and other leaders in teaching and implementing PH. The seminal work presented here is merely the beginning of a multistep effort to advance PH in nursing. An important next step is the concurrent nationwide project under the auspices of the American Nurses Association (ANA) – a larger survey, “Precision Health and Genomics” (closed, July 2023) (Gelinas, 2021). PH competencies, informed by this larger survey, should appear in ANA’s Nursing: Scope and Standards of Practice as early as 2025.
Additionally, the PHNCS, proven to have face validity and reliability, was noted to be an appropriate scale to assess the KSA of nurses relevant to PH. This scale can be used in addition to the Genetic and Genomics in Nursing Practice Scale (GGNPS) to assess the nurses' KSAs on a larger scale.
Implications for Practice
Professional nursing practice, rooted in quality and safety for cohorts of consumers or disease-based populations, has not been able to give truly-individualized care due to a lack of data and information about people, their genes, and their environment that now exist. Entraining an individual’s factors into a plan of care will be every nurse’s responsibility, irrespective of the practice arena. Full adoption of PH will depend upon the profession’s ability to embrace this healthcare evolution, seizing the chance to transform nursing practice and inspire patient engagement in all clinical encounters to improve outcomes. Nursing education must respond to the inevitable massive cultural change necessitated by this conversion to PH or the profession will be outperformed by other providers who are both willing and ready to lead.
Future research should target the underpinnings of this lack of knowledge and/or confidence. That is, while this survey provides some answers to how nurses feel about the integration of PH and its benefits, further exploration of underlying hesitancies e.g., higher workload, inability, or unwillingness to “learn new things”, feasibility issues in training, or a belief in the predominance of medical (as opposed to interprofessional) approaches to care provision is needed.
Limitations
The study limitations include common ones such as a small sample size, the cross-sectional design, convenience sampling strategy, and poor response rate. Out of the four sites targeted, only nurses from two sites participated. Application of the findings to nursing education and practice more globally necessitates a larger, nationwide sampling.
Conclusion
The adoption of Precision Medicine and Precision Health has been a remarkable step forward in providing targeted therapies to individual patientsThe adoption of Precision Medicine and Precision Health has been a remarkable step forward in providing targeted therapies to individual patients based on the patient’s own genetic and genomic markers. Incorporating this genetic data with information on the individual patient’s SoDH and environmental factors, as well as digital data from wearables, has given healthcare providers the means to deploy digital therapeutics on an individual level. This ability has already shown great promise in treating patients as individuals rather than as a group of persons with the same medical diagnosis (Gelinas, 2021).
National and global initiatives have undertaken the necessary research to implement precision health which will improve health (Ginsberg, et al., 2018). To put this valuable research into practice, nurses must have the requisite knowledge and understanding of PH that will enable them to provide quality patient care that leads to positive outcomes and enhanced patient safety. The emerging art and science of PH call for nursing educational programs that will set standards for minimum nursing competencies and provide the necessary knowledge for both the beginning and the advanced practice nurses (Gelinas, 2021).
A healthy start is found in the establishment of baseline KSAs of nurses about PH, genetic/genomic data, and other non-traditional sources of data which are critical to the design of comprehensive curricula in all levels of nursing education. the information derived from the use of the PHNCS will form the basis for the necessary PH curriculum development, and thus allow nurses to assess, diagnose, plan, intervene, and evaluate the outcomes for their patients more accurately.
Acknowledgement: Drs. Gagalang and Schultz wish to acknowledge the passing of a valued contributor to this work, Dr. Marisa Wilson (1957-2024). Her contributions to precision health and informatics nursing will never be forgotten.
Authors
Evangeline Fangonil-Gagalang, PhD, MSN, RN
Email: egagalang@csusb.edu
ORCID ID: https://orcid.org/0000-0002-6016-087X
Evangeline Fangonil-Gagalang is an assistant professor and the undergraduate nursing program director at the California State University, San Bernardino (CSUSB) in San Bernardino, California. Dr. Gagalang Co-Chairs the Precision Health and Genomics workgroup convened by the American Nurses Association in their efforts to develop basic competencies for Precision Health and update the advanced competencies for Genomics Nursing. Dr. Gagalang was the co-primary investigator and awardee of the All of Us research grant from the American Association of Colleges of Nursing, a collaborative effort with the National Institute of Health in their goal to achieve one million human samples to represent “all of us” in health research.
Recently, Dr. Gagalang authored the “Integration of Precision Health in a Baccalaureate Curriculum” where she described the processes of incorporating concepts of Precision Health in six identified courses. This year, Dr. Gagalang became a fellow in the American Association of Colleges in Nursing’s Elevating Leadership in Academic Nursing (ELAN) program, a year-long training to prepare for successful executive leadership.
Mary Anne Schultz, PhD, MBA, MSN, RN, FAAN
Email: mschultz@csusb.edu
ORCID ID: https://orcid.org/0000-0002-8874-6610
Mary Anne Schultz is Professor Emerita and an Informaticist in the Department of Nursing at the California State University, San Bernardino. She is a former Department Chair and Associate Dean, now a Consultant specializing in Precision Health. She holds a gubernatorial appointment (California, Newsom) to the state’s Advisory to Advance Precision Medicine, and she chairs a workgroup of a CMS-sponsored committee on Post-Acute Care Interoperability (PACIO) under the CARIN Initiative. She holds numerous awards for scholarship and writing in data science and informatics.
Laurie A. Huryk MSN, RN-BC
Email: lhuryk@centrastate.com
Laurie A. Huryk is a board-certified Informatics Nurse Specialist at CentraState Healthcare System in Freehold, NJ. As the lone nurse informaticist at CentraState, Ms. Huryk supports the use of electronic health records by all nursing management and staff within the hospital and ambulatory settings. Ms. Huryk is also an adjunct professor at Rutgers, the State University of New Jersey, where she provides expert instruction in Information Technology for Evidence Based Practice in the DNP program. Ms. Huryk sits on the boards of the Greater Delaware Valley American Nursing Informatics Association, New Jersey State Nurses Association Region 6, and New Jersey State Nurses Association Congress on Policy and Practice. Her passion for precision health and its potential stems from her many years of work in oncology, information technology, and recognition of the influence of social determinants of health while serving the underserved at a Federally Qualified Health Center.
Pamela A. Payne, DBe., MSN, WHNP-BC (NCC-E)
Email: pamelapayne818@gmail.com
Pamela Payne earned a BSN and MSN from California State University Los Angeles. She holds a doctorate in Bioethics from Loyola University Chicago, with specialization in research ethics, ELSI genomics/genetic therapies, reproductive ethics (with an emphasis in prenatal genetic screening), and nursing ethics. Dr. Payne previously had a clinical practice as a board-certified Women’s Health Nurse Practitioner for 21 years, and also taught Maternal/Infant Nursing and Health Assessment at CSULA for 10 years. She currently serves on the Ethics Committee of Huntington Memorial Hospital, Pasadena, CA, and the IRB for Adventist Health Systems, Glendale, CA.
Anna E. Schoenbaum, DNP, MS, RN-BC, FHIMSS
Email: anna.schoenbaum@pennmedicine.upenn.edu
ORCID ID: https://orcid.org/0000-0003-1468-6528
Anna E. Schoenbaum is the Vice President of Applications and Digital Health in the Department of Information Services at Penn Medicine (University of Pennsylvania Health System), Philadelphia. She oversees a wide range of applications and digital solutions to transform the health ecosystem to improve health and achieve health equity. She serves on the HIMSS Nursing Informatics Committee and is the co-chair of the Nursing Innovation Advisory Workgroup. She also serves on the Maryland HIMSS Board of Directors and teaches informatics at the University of Maryland School of Nursing. She is also the 2023 HIMSS and ANI Changemaker Nursing Informatics Leadership recipient.
Kimberly Velez, MSN, RN, NYAM Fellow
Email: kvelez1@northwell.edu
Kimberly Velez is an Expert Learning and Organizational Development Educator in the Digital IT & Services Office of the OCIO at Northwell Health, Lake Success, New York, where she educates on the Electronic Health Record (EHR) and clinician workflow. Kimberly serves on the boards of ANIA NY Tri-State, ANA-NY, and the planning committee of HIMSS NY Nursing Chapter Informatics Committee. She also serves on the boards of six nursing organizations on National, State, and Local levels, 14 years on the NYS Board for Nursing, and published on EHR inclusion in nursing school curriculum. Kimberly was appointed as a New York Academy Fellow ‘23 and recipient of the NCNW Award for Leadership and Community ‘22.
Marisa L. Wilson DNSc, MHSc, RN-BC, CPHIMS, FAMIA, FIAHSI, FAAN
Email: mwilsoa@uab.edu
ORCID ID: https://orcid.org/0000-0003-3320-5275
Marisa L. Wilson received her Master's degree from the Johns Hopkins University Bloomberg School of Public Health and her doctorate from the Johns Hopkins University School of Nursing. Dr. Wilson spent over two decades in epidemiological, clinical, and operational informatics work in public health, acute care, and post-acute care settings. Dr. Wilson also has 15 years of clinical direct care and healthcare leadership experience. She is currently an Associate Professor and Director of the Nursing Health Services Leadership Graduate Pathways at the University of Alabama at Birmingham School of Nursing (UABSON). She also coordinates the MSN Nursing Informatics program. Dr. Wilson is a core faculty member in the Doctor of Nursing Practice (DNP) and Executive DNP programs at UABSON. She is also an Associate faculty member for the Informatics Institute of the University of Alabama at Birmingham School of Medicine. She was a 2012 American Association of Colleges of Nursing Leadership for Academic Nursing fellow. Dr. Wilson is actively involved in the Nursing Knowledge Big Data Science Initiative, IMIA, AMIA, and HIMSS through her work with informatics continuing education programs and mentorship of new informaticians. She was a HIMSS 2022 ANI Innovator awardee.
References
Calzone, K., Jenkins, J., Prows, C., & Masny, A. (2011). Establishing the outcome indicators for the essential nursing competencies and curricula guidelines for genetics and genomics. Journal of Professional Nursing, 27(3), 179–191. https://doi.org/10.1016/j.profnurs.2011.01.001.
Duong, M. T., Rauschecker, A. M., Rudie, J. D., Chen, P.-H., Cook, T. S., Bryan, R. N., & Mohan, S. (2019). Artificial intelligence for precision education in radiology. The British Journal of Radiology, 92(1103), 20190389. https://doi.org/10.1259/bjr.20190389.
Flowers, E., Martin, M., Abid, H., Binford, S., & Mackin, L. (2019). Pairing pedagogical and genomic advances to prepare advanced practice nurses for the era of precision health. BMC Medical Education, 19(1), 112. https://doi.org/10.1186/s12909-019-1542-x.
Formea, C. M., Nicholson, W. T., Rohrer-Vitek, C., Wix, K. K., McCullough, K. B., Cunningham, J. L., Zeuli, J. D., Matey, E. T., Merten, J. A., Richardson, D. M., Billings, A. L., & Schramm, G. E. (2018). Implementation of a pharmacogenetics education program for pharmacists. American Journal of Health System Pharmacy, 75(23), 1939-1946, 10.2146/ajhp170771 https://doi.org/10.2146/ajhp170771.
Fu, M. R., Kurnat-Thoma, E., Starkweather, Al, Henderson, W. A., Cashion, A. K., Williams, J. K., Katapodi, M. C., Reuter-Rice, K., Hickey, K. T., Barcelona de Mendoza, V., Calzone, K., Conley, Y. P., Anderson, C. M., Lyon, D. E., Weaver, M. T., Shiao, P. K., Constantino, R. E., Wung, S. F., Hammer, M. J.,… Coleman B. (2019). Precision health: A nursing perspective. International Journal of Nursing Science, 7(1),5-12. https://doi.org/10.1016/j.ijnss.2019.12.008.
Gelinas, L. (2021). Genomics and precision health and genomics: Looking into the future [editorial]. American Nurse Journal, 16(8), 4. https://www.myamericannurse.com/wp-content/uploads/2021/08/an8-Gelinas-727.pdf
Ginsburg, G. S., & Phillips, K. A. (2018). Precision medicine: From science to value. Health Affairs, 37(5), 694-701. https://doi.org/10.1377/hlthaff.2017.1624.
Human Genome Project. (2003). https://www.genome.gov/human-genome-project
McGrath, S. P., Walton, N., Williams, M. S., Kim, K. K., & Bastola, K. (2019). Are providers prepared for genomic medicine: Interpretation of direct-to-consumer genetic testing (DTC-GT) results and genetic self-efficacy by medical professionals. BMC Health Services Research, 19(1), 844. https://doi.org/10.1186/s12913-019-4679-8.
National Research Council. (2011). Toward precision medicine: Building a network for biomedical research and new taxonomy of disease. The National Academies Press; Washington, D.C. https://doi.org/10.17226/13284


