Professional organizations have a role in maintaining a healthy profession. Despite the significance of American Nurses Association (ANA) Nursing Scope and Standards of Practice document as a preeminent guide for nurses, little is known about its diffusion and adoption in nursing practice. Members of ANA Committee on Nursing Practice Standards developed and administered a national survey to generate new knowledge on diffusion characteristics of the document using Rogers’ diffusion of innovation model. A total of 1679 participants were included in the descriptive and content analysis. Despite high agreement levels among respondents regarding the purpose of and need for the document, findings revealed that the document was not widely diffused or adopted. Awareness, the first criteria for diffusion, was found to be both a barrier and a needed strategy. Observability, a key component for adoption, had a low agreement level for making a difference in one’s own and a peer’s practice.
Key Words: standards of practice, scope of practice, nursing, nursing practice, diffusion of innovation, nursing profession, profession, professional association, professional organization, American Nurses Association
ANA advocacy...can be characterized in its commitment to the essential work associated with the development, maintenance, revision, and dissemination of the scope and standards of practice for the nursing profession. The American Nurses Association (ANA) Enterprise’s current mission statement reads, “Lead the profession to shape the future of nursing and health care,” describes the requisite professional organization’s actions to reach the vision of “A healthy world through the power of nursing” (ANA Enterprise, n.d., paras. 2-3). ANA advocacy for the over four million registered nurses (RNs) in the United States can be characterized in its commitment to the essential work associated with the development, maintenance, revision, and dissemination of the scope and standards of practice for the nursing profession. This fulfills the description by Matthews (2012) of the role of professional organizations to maintain a healthy profession, including proactive advocacy work characterized by the foundational documents, particularly the various scope and standards of practice publications for nurses developed over the course of many years.
The ANA initial Standards of Nursing Practice published in 1973 were crafted by the Congress for Nursing Practice as “…measures to judge the competency of its membership and evaluate the quality of its services” (ANA, 1973, p. 1). An initial nursing scope of practice statement, additional editions of standards of clinical nursing practice and advanced practice registered nursing, and combined nursing scope and standards of practice editions followed (ANA, 1987, 1991, 1996, 1998, 2004, 2010, 2015b). In 1995, the ANA Congress of Nursing Practice directed the Committee on Nursing Practice Standards and Guidelines to establish a process for periodic review and revision of nursing standards (ANA, 1998, p. viii). This committee, now known as the Committee on Nursing Practice Standards, reports to the ANA Board of Directors and has been charged with oversight accountability to maintain the ANA scope and standards program.
Specialty nursing scope and standards of practice build on the general nursing standards and competencies and help to preserve consistency and one voice for nursing.In 2015, committee member discussions focused on the magnitude of awareness and use of one of the foundational documents, Nursing: Scope and Standards of Practice (ANA, 2004, 2010, 2015b). Committee members elected to conduct a national survey to garner evidence about the impact of this professional resource. The Nursing Scope and Standards of Practice documents described the who, what, where, when, why, and how of nursing in the scope of practice statement and identify standards of practice and professional performance and accompanying competencies applicable to all RNs in the United States (U.S.), including those prepared at the graduate level to include advanced practice registered nurses (APRNs). Specialty nursing scope and standards of practice build on the general nursing standards and competencies and help to preserve consistency and one voice for nursing.
A review of literature revealed that...evaluation of successful integration or logistics of implementation are not widely discussed.Despite the significance of the ANA Nursing Scope and Standards of Practice (NSSP) document as a preeminent guide for nurses, little is known about its diffusion and implementation and/or adoption in nursing practice. A review of literature revealed that while some of the ANA foundational documents and nursing specialties have written about incorporation of specific standards of practice documents, evaluation of successful integration or logistics of implementation are not widely discussed (McCormick & Calzone, 2017; Sipes et al., 2017). Marion et al. (2017) detailed the rationale, development, and impact of a new addition to the 2015 NSSP document, Standard 8 Culturally Congruent Practice (ANA, 2015b), and provided examples of its application, implementation, and evaluation in clinical, educational, and research environments. The American Association of Colleges of Nursing (2021) Concept Across Domains: Ethics recently highlighted the ANA 2015 Code of Ethics for Nurses (ANA, 2015a) as a foundational document to develop curriculum in nursing education models supporting nurse moral agency development.
Examples included reflecting the standards in job descriptions, performance reviews, corrective action plans, and topic presentations.Regarding nursing specialties, Sipes et al. (2017) evaluated a tool that identified competencies needed for health information technology roles against other tools specific for nursing informatics, including the Nursing Informatics: Scope and Standards of Practice, Second Edition ([NISSP], ANA 2014). The many gaps discovered led the authors to recommend using the NISSP as a framework for measuring competencies. Gomez et al. (2017) described the development of the Nephrology Nursing Scope and Standards of Practice, 8th Edition (American Nephrology Nurses Association, 2017), based on the ANA (2015b) NSSP along with examples of how the document was integrated into clinical practice. Examples included reflecting the standards in job descriptions, performance reviews, corrective action plans, and topic presentations. Herena et al. (2018) provided a thorough example of utilizing the Clinical Research Nursing: Scope and Standards of Practice (ANA, 2016) as a foundation to develop and evaluate an orientation course for new oncology research nurses.
The absence of literature confirms how little is known about the diffusion and adoption of the foundational ANA NSSP documents in education, administration, practice, and research spaces. This research, which started as an idea among members in the ANA Committee on Nursing Practice Standards, is an example of nursing organization advocacy informing the profession of nursing. The purpose of developing and administering a national survey on the ANA NSSP document was to generate new knowledge gleaned from RNs in the U.S. about the dissemination and implementation and/or adoption of the document in nursing education and practice settings. The research aims were to describe survey respondent demographics and characteristics related to the diffusion of the ANA NSSP (general) documents and identify barriers, facilitators, and outcomes to the implementation/adoption of the document.
Methods
The RDI framework describes how an idea, practice, or product spreads over time within a social network...The research design was a descriptive, cross-sectional, mixed methods study using survey methodology. Committee members as investigators developed the National Survey on the ANA Nursing Scope and Standards of Practice document based on Rogers’ Diffusion of Innovations (RDI) Theoretical Framework (Rogers, 2003). The RDI framework describes how an idea, practice, or product spreads over time within a social network and is influenced by communication, perceptions, and decision-making within a five-step process: knowledge, persuasion, decision, implementation, and confirmation. Rogers’ (2003) diffusion of innovation curve categorizes the rate of adoption from early (innovators) to late (laggards).
The 31-item survey consisted of the following:
- nine demographic questions including age, gender, race/ethnicity, highest earned nursing degree, advanced practice nurse status, state of employment, employment setting, role/position, and change disposition
- NSSP awareness methods including communication methods and document version(s) read
- 14 NSSP document diffusion characteristics with a 5-point response scale from strongly disagree to strongly agree
- four open-ended items related to NSSP document implementation/adoption barriers, strategies, outcomes, and general comments.
The survey had a content validity index of 0.90 among five committee members. Survey Monkey (2016) was the web-based platform used to administer and collect responses from study participants. Skip-logic was used within the survey, based on a question addressing participants’ awareness of the NSSP document, to progress through survey items on awareness methods, diffusion characteristics, and open-ended questions. Table 1 crosswalks the RDI framework elements to related survey items on ANA NSSP document diffusion characteristics.
Table 1. Crosswalk of Rogers’ Diffusion of Innovation (RDI) Framework Components and National Survey on ANA Nursing Scope and Standards of Practice Document Diffusion Items
|
RDI Framework Element |
National Survey on ANA’s Scope and Standards of Practice Document Diffusion Item |
|---|---|
| Personality Characteristics | What is your general disposition toward change and adoption? |
| Awareness Knowledge | I am aware of ANA’s Nursing Scope and Standards of Practice document (inclusion criteria) |
| Which ANA Nursing Scope and Standards of Practice documents have you read? | |
| Social System | By which communication method did you become aware of ANA’s Nursing Scope and Standards of Practice document? |
| Persuasion -Characteristics | |
| Relative advantage | The document fulfills a need for the nursing profession |
| The document is a respected resource for professional nursing | |
| Compatibility | The document is consistent with existing values, practices, and needs of nurses |
| Complexity | The document is easy to understand |
| Trialability | The document is easy to use/apply in any practice setting |
| Observability | Outcomes of using the document are visible to nurses |
| Knowledge | |
| Principles | I know the purpose of the document |
| How-To | I know examples of how the document can be or has been used in practice |
| Decision | I have tried using the document in practice |
| Implementation | I have integrated the document into my current practice |
| Reinvention | I feel the document is updated to reflect current healthcare needs and trends |
| I provide input into the document revision through task force participation and/or public comment | |
| Confirmation | I feel using the document has made a difference in my practice |
| I feel using the document has made a difference in the practice of my peers |
...current U.S. RNs practicing nursing in any role or setting...were invited to complete the survey.The research was approved by the principal investigator’s organizational institutional review board as an exempt study. Information about the study was provided in the introductory letter included as the first page of the web-based survey. Using multimodal snowball sampling to disseminate the web-based link and solicitation/introductory letter, current U.S. RNs practicing nursing in any role or setting (inclusion criteria) were invited to complete the survey. Committee members disseminated the survey link to their contacts using a variety of mediums, including social media. The survey link was posted on ANA social media platforms. Voluntary completion of the survey by respondents indicated their willingness to participate in the study. Anonymity of respondents was assured as no personal identifying information was requested in the survey.
The survey period was from January 11, 2016, through February 29, 2016. At the conclusion of the survey period, survey data were downloaded from the web-based survey platform as an Excel file, prepared for data analysis, and transferred into the IBM SPSS statistical program (IBM SPSS Statistics for Windows, Version 24.0.) for analysis. Survey data were accessed and maintained in the principal investigator’s password-protected computer.
Descriptive and conventional content analysis (Hsieh & Shannon, 2005) were applied to describe the data and address study aims. Descriptive analysis included frequency, percentage, and measure of central tendency. Variables from participants meeting inclusion criteria were analyzed. Investigators used consensus agreement when deciding to include/exclude participants based on survey item responses in relation to inclusion criteria. Quantitative data were reported in aggregate form, including missing data. Hsieh and Shannon (2005) described conventional content analysis as an inductive method where themes and subthemes flow from the data. Investigators independently reviewed qualitative responses to the open-ended questions and, through group consensus, developed the themes and subthemes that emerged. A coding schema based on the themes and subthemes was then assigned. Investigators independently applied the coding schema to responses, gained consensus on coding application with a partner, and achieved group consensus on final coding assignments among all investigators.
Results
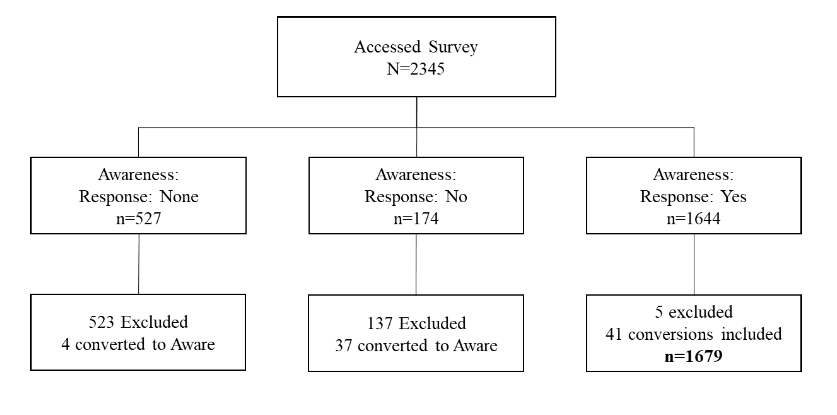
The total number of participants meeting inclusion criteria and who were aware of the ANA (2015) NSSP documents was 1,679. Figure 1 depicts how survey respondents were handled by consensus of the investigators. Despite the skip-logic applied within the survey for the question on awareness of the ANA NSSP, 41 participants who did not declare, or declared no awareness, were included in the sample for data analysis. Five respondents who indicated awareness were excluded from the sample as they did not meet inclusion criteria (i.e., retired or student nurses).
Figure 1. Flow Diagram of Participant Responses and Resultant Sample
Demographics
Participant demographics included age (M = 51.10, SD = 11.24), gender (mostly female), race/ethnicity (predominantly white), highest nursing degree (88% BSN or higher), years practicing as an RN (M = 24.58, SD = 13.13), advanced practice registered nurse status (23%), state of employment (all 50 states represented), employment setting (mainly hospital), employment role (highest percent in direct care) and change disposition (high rate of adoption). Tables 2-4 detail participant demographic variables.
Table 2. Participant Demographics
|
Variable |
n |
% |
|---|---|---|
| Age | ||
| 18–29 | 75 | 4.5 |
| 30–34 | 100 | 6.0 |
| 35–39 | 118 | 7.0 |
| 40–44 | 149 | 8.9 |
| 45–49 | 163 | 9.7 |
| 50–54 | 264 | 15.7 |
| 55–59 | 341 | 20.3 |
| 60–64 | 282 | 16.8 |
| ≥ 65 | 126 | 7.5 |
| Missing | 61 | 3.6 |
| RN Years | ||
| 0–10 | 350 | 20.8 |
| 11–20 | 282 | 16.8 |
| 21–30 | 393 | 23.4 |
| 31–40 | 389 | 23.2 |
| > 40 | 227 | 13.5 |
| Missing | 38 | 2.3 |
| Gender | ||
| Female | 1568 | 93.4 |
| Male | 107 | 6.4 |
| Missing | 4 | 0.2 |
| Race/Ethnicity | ||
| White | 1427 | 85 |
| Black/African American | 95 | 5.7 |
| Asian | 42 | 2.5 |
| Alaskan/American Indian | 10 | 0.6 |
| Hispanic/Latino | 53 | 3.2 |
| Hawaiian/Pacific Islander | 14 | 0.8 |
| Mixed/Other | 31 | 1.8 |
| Missing | 7 | 0.4 |
| Nursing Education | ||
| MSN | 683 | 40.7 |
| BSN | 540 | 32.2 |
| ASN | 152 | 9.1 |
| PhD/Other Doctorate | 145 | 8.6 |
| DNP | 107 | 6.4 |
| Diploma | 40 | 0.7 |
| Missing | 12 | 0.7 |
| Advanced Practice RN (APRN) | ||
| Not APRN | 1154 | 68.7 |
| Nurse Practitioner | 190 | 11.3 |
| Clinical Nurse Specialist | 128 | 7.6 |
| Nurse Midwife | 10 | 0.6 |
| Nurse Anesthetist | 7 | 0.4 |
| Missing | 190 | 11.3 |
| Primary Employment Setting | ||
| Hospital | 783 | 46.6 |
| Academic Institution | 280 | 16.7 |
| Government | 105 | 6.3 |
| Ambulatory Care/Call Center/Clinic/Urgent Care | 89 | 5.3 |
| Community-based Center/Public Health | 85 | 5.1 |
| Self-employed/Consultant | 53 | 3.2 |
| Healthcare Industry/Insurance | 45 | 2.7 |
| Physician/Private Practice | 44 | 2.6 |
| School Health Service | 43 | 2.6 |
| Extended/Long-term Care | 36 | 2.1 |
| Home Health | 35 | 2.1 |
| Employee/Occupational Health | 12 | 0.7 |
| Correctional | 5 | 0.3 |
| Other | 54 | 3.2 |
| Missing | 10 | 0.6 |
| Role/Position | ||
| Direct-care Nurse | 439 | 26.1 |
| Faculty/Professor/Researcher | 225 | 13.4 |
| Nurse Educator/Staff Development | 201 | 12.0 |
| Senior Nurse Administrator/Executive | 148 | 8.8 |
| Nurse Manager | 136 | 8.1 |
| Nurse Practitioner | 108 | 6.4 |
| Case Manager/Discharge Planner/Utilization Review | 81 | 4.8 |
| Informaticist | 64 | 3.8 |
| Legal/Quality/Regulatory Nurse | 60 | 3.6 |
| Nursing Supervisor | 59 | 3.5 |
| Community Clinic/Public Health/Occupational/School Nurse | 59 | 3.5 |
| Clinical Nurse Specialist | 52 | 3.1 |
| Government Administrator | 10 | 0.6 |
| Policy Developer | 9 | 0.5 |
| Nurse Midwife | 1 | 0.1 |
| Nurse Anesthetist | 1 | 0.1 |
| Other | 18 | 1.1 |
| Missing | 8 | 0.5 |
Table 3. Participant State and/or Territory
|
State |
n |
% |
|---|---|---|
| NY | 133 | 7.9 |
| NJ | 97 | 5.8 |
| CA | 95 | 5.7 |
| MO | 94 | 5.6 |
| TN | 86 | 5.1 |
| PA | 86 | 5.1 |
| TX | 84 | 5.0 |
| NC | 71 | 4.2 |
| OK | 59 | 3.5 |
| FL | 50 | 3.0 |
| WA | 49 | 2.9 |
| IN | 47 | 2.8 |
| IL | 44 | 2.6 |
| LA | 40 | 2.4 |
| OH | 39 | 2.3 |
| GA | 39 | 2.3 |
| VA | 38 | 2.3 |
| WI | 37 | 2.2 |
| MD | 34 | 2.0 |
| MA | 31 | 1.8 |
| MI | 29 | 1.7 |
| CT | 26 | 1.5 |
| SD | 24 | 1.4 |
| MT | 23 | 1.4 |
| SC | 21 | 1.3 |
| RI | 20 | 1.2 |
| AZ | 20 | 1.2 |
| NM | 19 | 1.1 |
| OR | 16 | 1.0 |
| KS | 16 | 1.0 |
| AR | 16 | 1.0 |
| MN | 14 | 0.8 |
| KY | 14 | 0.8 |
| DE | 13 | 0.8 |
| CO | 13 | 0.8 |
| NE | 12 | 0.7 |
| ME | 12 | 0.7 |
| MS | 11 | 0.7 |
| ID | 11 | 0.7 |
| IA | 10 | 0.6 |
| AL | 10 | 0.6 |
| VT | 8 | 0.5 |
| WY | 7 | 0.4 |
| DC | 7 | 0.4 |
| WV | 6 | 0.4 |
| UT | 5 | 0.3 |
| HI | 5 | 0.3 |
| NH | 4 | 0.2 |
| ND | 3 | 0.2 |
| NV | 3 | 0.2 |
| AK | 3 | 0.2 |
| GU | 2 | 0.1 |
| PR | 1 | 0.1 |
| Missing | 22 | 1.3 |
Table 4. Participant Change Disposition
|
Rate of Adoption |
n |
% |
|---|---|---|
| Innovator: Take risks, adopt quickly | 447 | 26.6 |
| Early Adopter: High opinion, judicious choice, adopt early | 896 | 53.4 |
| Early Majority: Some opinion, adopt after time | 320 | 19.1 |
| Late Majority: Skeptic, adopt after majority | 8 | 0.5 |
| Laggard: No opinion, adverse to change, adopt last | 4 | 0.2 |
| Missing | 4 | 0.2 |
Diffusion Characteristics
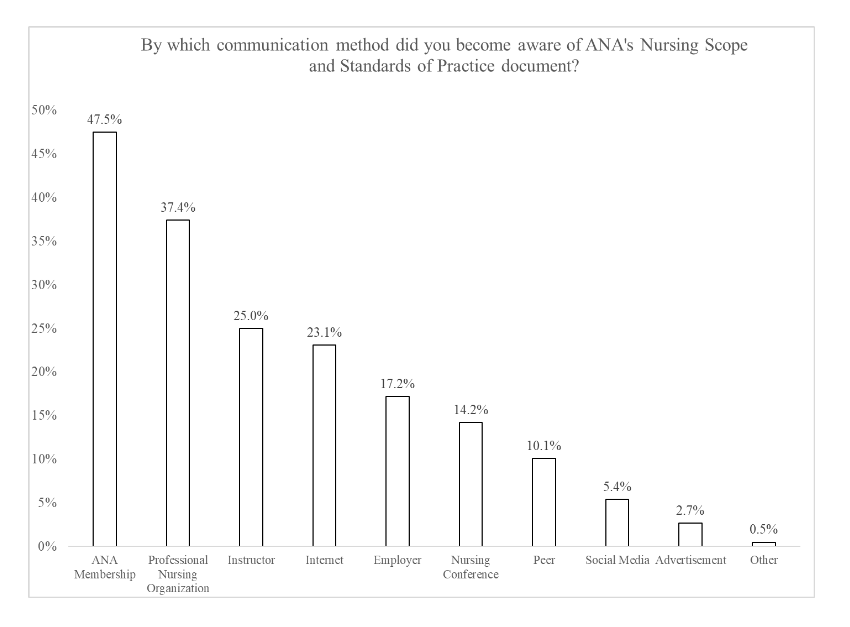
Diffusion characteristics included awareness of the ANA NSSP documents (inclusion criteria), awareness methods, document version read, and 14 statements addressing document diffusion elements based on Roger’s Diffusion of Innovation framework with a 5-point level of agreement response scale. ANA membership (48%) was the predominant communication method for awareness of the NSSP documents (Figure 2). At the time of the survey, the 2004, 2010, and 2015 NSSP versions were read by 35%, 68%, and 48% of respondents, respectively.
Figure 2. Awareness Methods
Based on the mean for the 14 document diffusion statements aligned with RDI model elements (Table 5), respondents had a high level of agreement for knowing the purpose of the document and the document fulfilling a need for the nursing profession. The lowest level of agreement was for providing input into the document revision.
Table 5. Level of Participant Agreement for Diffusion Characteristics
|
Item |
n |
Mean |
|---|---|---|
| The document fulfills a need for the nursing profession | 1636 | 4.35 |
| The document is a respected resource for professional nursing | 1638 | 4.31 |
| The document is consistent with existing values, practices, and needs of nurses | 1639 | 4.26 |
| The document is easy to understand | 1638 | 3.99 |
| The document is easy to use/apply in any practice setting | 1634 | 3.85 |
| Outcomes of using the document are visible to nurses | 1630 | 3.57 |
| I know the purpose of the document | 1627 | 4.38 |
| I know examples of how the document can be or has been used in practice | 1639 | 4.02 |
| I have tried using the document in practice | 1635 | 3.91 |
| I have integrated the document into my current practice | 1627 | 3.89 |
| I feel the document is updated to reflect current healthcare needs and trends | 1635 | 3.92 |
| I provided input into the document revision through task force participation and/or public comment | 1622 | 2.59 |
| I feel using the document has made a difference in my practice | 1631 | 3.61 |
| I feel using the document has made a difference in the practice of my peers | 1630 | 3.44 |
Content Analyses
Content analysis of responses to open-ended questions on the survey identified themes and subthemes for barriers, facilitators, and outcomes related to implementation and/or adoption of the NSSP document and general comments.
Barriers. Six main themes identified from the open-ended question, “What are barriers to adopting and/or implementing ANA’s Nursing Scope and Standards of Practice?” included systems, standards, setting, cognition, professionalism, and support. Within each theme, subthemes were identified. Table 6 depicts the frequency of investigators’ consensus coding. A total of 941 respondents provided comments for this item, 919 were appropriate for coding, generating 1,716 codes.
Table 6. Frequency of Themes and Subthemes for Barriers
|
Theme |
n |
% |
|---|---|---|
| Systems | 688 | 40.1 |
| Awareness | 149 | 21.7 |
| Time | 102 | 14.8 |
| Availability/ Dissemination | 91 | 13.2 |
| Change | 78 | 11.3 |
| Accessibility | 64 | 9.3 |
| External Influence | 52 | 7.6 |
| Cost | 48 | 7.0 |
| Applicability | 33 | 4.8 |
| Resources | 23 | 3.3 |
| Staffing | 20 | 2.9 |
| Priorities | 17 | 2.5 |
| Communication | 11 | 1.6 |
| Standards | 221 | 12.9 |
| Usability/Utility/Practicality | 131 | 59.3 |
| Value | 47 | 21.3 |
| Specificity | 28 | 12.7 |
| Sensitivity | 15 | 6.8 |
| Setting | 217 | 12.6 |
| Culture | 95 | 43.8 |
| Employer | 70 | 32.3 |
| Integration | 52 | 24.0 |
| Cognition | 206 | 12.0 |
| Knowledge | 73 | 35.4 |
| Understanding | 67 | 32.5 |
| Meaning | 28 | 13.6 |
| Language | 21 | 10.2 |
| Clarity | 17 | 8.3 |
| Professionalism | 204 | 11.8 |
| Responsibility/ Accountability | 86 | 41.9 |
| Role | 53 | 26.1 |
| Membership | 40 | 19.7 |
| Antecedent Personal Characteristics | 25 | 12.3 |
| Support | 181 | 10.5 |
| Leaders | 112 | 61.9 |
| Education/ Training | 52 | 28.7 |
| Professional Organization | 14 | 7.7 |
| Mentoring | 3 | 1.7 |
Strategies. Six main themes identified from the open-ended question, “What are strategies to adopting and/or implementing ANA’s Nursing Scope and Standards of Practice?” included communication/dissemination, demonstration, education, organizational frameworks, professional organizations, and regulations. Within each theme, subthemes were identified. Table 7 depicts the frequency of investigators’ consensus coding. A total of 831 respondents provided comments for this item; 758 were appropriate for coding, producing 1,407 codes.
Table 7. Frequency of Themes and Subthemes for Strategies
|
Theme |
n |
% |
|---|---|---|
| Communication/Dissemination | 425 | 30.2 |
| Make Accessible/Available | 115 | 27.1 |
| Publicize | 73 | 17.2 |
| Use Technology | 67 | 15.8 |
| Forums | 53 | 12.4 |
| Language | 52 | 12.2 |
| Advertise | 43 | 10.1 |
| Social Networks | 22 | 5.2 |
| Educate | 350 | 24.9 |
| School of Nursing Curriculum | 115 | 32.9 |
| Methods | 69 | 19.7 |
| Continuing Education | 68 | 19.4 |
| Professional Development | 49 | 14.0 |
| Education | 26 | 7.4 |
| Role Development | 23 | 6.6 |
| Demonstration | 255 | 18.1 |
| Leadership | 119 | 46.7 |
| Case Studies | 38 | 18.1 |
| Outcomes | 41 | 16.1 |
| Evidence-Based | 29 | 11.4 |
| Transformative Practice | 28 | 11.0 |
| Organizational Framework | 224 | 15.9 |
| Job Description/Performance Review | 67 | 29.9 |
| Policy/Procedures | 46 | 20.5 |
| Orientation | 31 | 13.8 |
| Strategic Planning | 28 | 12.5 |
| Magnet | 22 | 9.8 |
| Professional Practice Model | 21 | 9.4 |
| Clinical Advancement Ladder | 9 | 4.0 |
| Regulations | 84 | 6.0 |
| Licensure/Renewal | 38 | 45.2 |
| Legalities | 19 | 22.6 |
| Accreditation | 11 | 13.1 |
| Public Policy | 10 | 11.9 |
| Defining Scope | 6 | 7.1 |
| Professional Organizations | 69 | 4.9 |
| Partnership | 28 | 40.6 |
| Membership | 12 | 17.4 |
| ANA Resources | 11 | 15.9 |
| Practice Standards | 7 | 10.1 |
| Publications | 7 | 10.1 |
| Certification | 4 | 5.8 |
Outcomes. Five main themes identified from the open-ended question, “What are measurable outcomes from adopting and/or implementing ANA's Nursing Scope and Standards of Practice?” included nurse, patient, organization, community/public, and other workforce. Within each theme, subthemes were identified. Table 8 depicts the frequency of investigators’ consensus coding. A total of 590 respondents provided comments for this item; 544 were appropriate for coding, producing 1,343 codes.
Table 8. Frequency of Themes and Subthemes for Outcomes
|
Theme |
n |
% |
|---|---|---|
| Nurse | 689 | 51.3 |
| Professional Practice | 282 | 40.9 |
| Professional Development | 110 | 16.0 |
| Engagement/Satisfaction | 78 | 11.3 |
| General | 69 | 10.0 |
| Professional Practice Evaluation | 54 | 7.8 |
| Role Differentiation | 38 | 5.5 |
| Human Resources | 35 | 5.1 |
| Leadership | 23 | 3.3 |
| Patient | 311 | 23.2 |
| General | 119 | 38.3 |
| Quality/Safety Measures | 102 | 32.8 |
| Satisfaction | 80 | 25.7 |
| Access | 10 | 3.2 |
| Organization | 228 | 17.0 |
| Systems/Structures | 62 | 27.2 |
| General | 50 | 21.9 |
| Financial | 34 | 14.9 |
| Learning Organization | 32 | 14.0 |
| Reporting | 19 | 8.3 |
| Recognition | 15 | 6.6 |
| Litigation | 13 | 5.7 |
| Regulatory | 3 | 1.3 |
| Community/Public | 58 | 4.3 |
| General | 29 | 50.0 |
| State Board Adoption | 13 | 22.4 |
| Legislation | 8 | 13.8 |
| Recognition | 5 | 8.6 |
| Partnerships | 3 | 5.2 |
| Other Workforce | 57 | 4.2 |
| General | 27 | 47.4 |
| Collaboration | 18 | 31.6 |
| Ethical Care | 7 | 12.3 |
| Care Planning | 5 | 8.8 |
General Comments
Five main themes were identified from the open-ended question, “Comments about this survey and/or the ANA Nursing Scope and Standards of Practice.” Main themes were opinion, survey, scope and standards document, stimulating professional development and action, and recommendations. Within each theme, subthemes were identified. Table 9 depicts the frequency of investigators’ consensus coding. A total of 320 participants provided comments for this item; 279 were appropriate for coding, producing 474 codes.
Table 9. Frequency of Themes and Subthemes for General Comments
|
Theme |
n |
% |
|---|---|---|
| Opinion | 163 | 34.4 |
| Other | 84 | 51.5 |
| ANA Sentiment | 30 | 18.4 |
| RN Role | 22 | 13.5 |
| Vital to Recognition as Profession | 15 | 9.2 |
| Advanced Practice | 8 | 4.9 |
| Interprofessional Connectedness | 4 | 2.5 |
| Survey | 148 | 31.2 |
| Appreciation for Survey | 68 | 45.9 |
| Instrumentation | 32 | 21.6 |
| Recommendations | 21 | 14.2 |
| Findings Dissemination | 19 | 12.8 |
| Purpose | 8 | 5.4 |
| Scope & Standards Document | 112 | 23.6 |
| Appreciation for Document | 38 | 33.9 |
| Applicability/Practicality | 29 | 25.9 |
| Other | 25 | 22.3 |
| Recommendations | 20 | 17.9 |
| Stimulating Professional Development & Action | 26 | 5.5 |
| Utilization of Document | 18 | 69.2 |
| Implementation of Document in Practice | 5 | 19.2 |
| Other | 3 | 11.5 |
| Recommendations | 25 | 5.3 |
| Additional Strategies | 18 | 72.0 |
| School/Nursing Program Curriculum | 7 | 28.0 |
Discussion
The purpose of advocacy efforts by professional organizations...is to inform professional nurses about matters that can improve the profession’s voice and accountability to society.The purpose of advocacy efforts by professional organizations such as the ANA is to inform professional nurses about matters that can improve the profession’s voice and accountability to society (Matthews, 2012). This research provides insights and perspectives on the dissemination and implementation/adoption of ANA NSSP documents. Applying the RDI framework, the NSSP document is the innovation. In addition to the innovation itself, adopters, communication channels, and social system are other key components necessary for diffusion and adoption (Rogers, 2003).
Adopters
Respondent demographics of this 2016 study have similarities and differences with the results of a 2020 national nursing workforce survey (Smiley et al., 2021) and are being examined based on the study time frame. Similarities between study respondents and workforce survey findings respectively included: median age - 56 years (2016) and 52 years (2020); age group 55 years or older - 45% and 43%; primarily female - 93% and 91%; mainly white - 85% and 81%; and employed in a hospital setting - 47% and 55%. Differences between study respondents and workforce survey findings respectively included baccalaureate or higher degree in nursing - 88% (2016) and 65% (2020); non-APRN status - 69% and 92%; academic employment setting - 17% and 3%; and direct care position - 26% and 60%. The aims of the two surveys were different and the differences in demographics may be attributed to this. What is notable is that in this study, participant demographics had higher nursing education levels, advanced practice registered nurse roles, and practice in academic settings.
Seventy-two percent of participants indicated awareness of the NSSP document.A personality characteristic of participants in this study was their self-reported disposition to change, with a majority being early adopters (53%), followed by innovators (27%). This contrasts with Roger’s diffusion of innovation curve whereby 13.5% are early adopters and 2.5% are innovators (Rogers, 2003). Seventy-two percent of participants indicated awareness of the NSSP documents. Approximately half of the participants had read at least one version of the NSSP document. Eighty-five percent of participants responded that the communication method for awareness was through affiliation or membership with a professional organization. This highlights the role of professional organizations in advocacy efforts such as communicating information and disseminating professional knowledge (Matthew, 2012).
Communication Channels
Communication channels enable the innovation to diffuse and spread.Within RDI communication channels, the innovation-decision process of adopters/nonadopters progressed through knowledge, persuasion, decision, implementation, and confirmation (Rogers, 2003). Communication channels enable the innovation to diffuse and spread. Regarding survey items reflecting these phases, findings demonstrated responses of participants who were aware of (i.e., had knowledge of) an ANA NSSP document and whose level of agreement began high with knowledge items and then progressively decreased as the phases progressed to the confirmation items. Qualitative findings related to barriers, strategies, and outcomes of implementing and/or adopting the document provided further insight into participants’ innovation-decision process.
Barriers. The persuasion phase is influenced by characteristics of the innovation itself including relative advantage, compatibility, complexity, trialability, and observability (Rogers, 2003). Overall, the system theme received the highest percentage of coding for barriers. Within this theme, the subtheme of awareness was the most frequent. Although survey respondents had awareness of the NSSP documents, awareness was also perceived as a major barrier to be overcome for diffusion to occur. Participants had high agreement levels for items reflecting relative advantage and compatibility and lower agreement levels for complexity, trialability, and observability.
Although survey respondents had awareness of the NSSP documents, awareness was also perceived as a major barrier...The complexity of the document can be represented by the subthemes, knowledge and understanding, under the cognition theme. Trialability of the document can be represented by the subtheme usability/utility/practicality under the standards theme. Observability of the document can be represented by the subtheme responsibility/accountability under the professionalism theme. Themes related to setting and support were also present in participant comments about barriers with subthemes of culture and leaders receiving higher percentages of coding within those themes, respectively. For an individual to be persuaded to seek additional information about an NSSP document, barriers within systems, standards, setting, cognition, professionalism, and support must be overcome (Table 6).
The strategies revealed in the qualitative findings provided insight from participants on how organizations can facilitate users to implement and adopt the NSSP document.Strategies. In keeping with the RDI framework, strategies reflect a period of decision and implementation within the innovation-decision process. The strategies revealed in the qualitative findings provided insight from participants on how organizations can facilitate users to implement and adopt the NSSP document. The two most prevalent themes were communication and education, including making the NSSP document more accessible/available and including the document in schools of nursing curriculum. For example, aside from placing copies of the NSSP document in libraries and in other accessible areas on patient care units or classrooms, organizations can purchase an e-license from ANA to make the NSSP document available for all nursing staff and/or students via organizational intranet resources. As awareness was a major systems barrier, including the document in schools of nursing curriculum is an aligned strategy to bring awareness, understanding, and application practice to nursing students.
Leadership is vital for nurses to be engaged and empowered.Demonstration and organizational frameworks are other strategy themes drawn from participant comments. Leadership is vital for nurses to be engaged and empowered. Kouzes and Posner’s (2016) Learning Leadership: The Five Fundamentals of Becoming an Exemplary Leader illustrates a framework leaders can use to demonstrate the NSSP document in practice. Three examples include “modeling the way” (i.e. setting the example by aligning actions with shared values), “inspiring a shared vision” (i.e. enlisting nurses in a common vision by appealing to shared aspirations), and “enable others to act” (i.e. fostering collaboration by building trust and facilitating relationships; (Kouzes & Posner, 2016, p. 26). Demonstration through leadership establishes the culture of professional practice, sets the tone for responsibility and accountability defined in the NSSP document, and addresses the diffusion barriers of setting and professionalism. Integrating the NSSP document in organizational frameworks such as strategic planning, professional practice models, policies and procedures, job descriptions, orientation programs, professional development programs, and performance reviews are examples of how leaders can support the decision and implementation phases.
Observable outcomes are important for individuals who are deciding to continue using the NSSP document.Outcomes. Outcomes link to the confirmation phase of the individual innovation-decision process. Confirmation is an integral part of any change endeavor; this is a time when an individual determines whether to continue, discontinue, or completely reject an innovation (Rogers, 2003). The level of agreement of survey respondents with items related to the document’s visibility of outcomes, making a difference in one’s practice, and making a difference in peer’s practice were on the lower end. Observable outcomes are important for individuals who are deciding to continue using the NSSP document. The nurse theme had the highest coding for outcomes, with the subtheme of professional practice receiving the greatest percentage of codes. Visibility of outcomes within this subtheme related to the document being integrated into and guiding professional nursing practice, such as the use of nursing process and demonstration of competent professional performance. Use of the nursing process and demonstrations of professional performance are the core processes of the NSSP document (Matthews, 2012; ANA, 2015b).
Patient and organizational outcome themes emerged from participant comments.Nursing practice directly impacts quality and safety for patients and organizational metrics. Patient and organizational outcome themes emerged from participant comments. Observable patient outcomes included quality and safety measures encompassing hospital-acquired infections, nursing sensitive indicators, and morbidity and mortality. Constant presence at the bedside positions nurses to focus on monitoring and assessing patients for reaction to clinical care, detecting errors and near misses, identifying and communicating changes in patient condition, and performing countless other tasks to ensure that patients receive high-quality care (Phillips et al. 2021). Other national organizations have recognized the connection between nurses and patient safety. The National Academies of Sciences, Engineering, and Medicine (2021) identified that The Joint Commission views the profession of nursing as part of its larger mission to support high-quality and safe care for the public, and the Agency for Healthcare Research and Quality recognizes the connection of patient safety as a measure of nurses’ quality of care.
These program frameworks promote a culture of nursing excellence and support a quality professional practice environment in healthcare organizations.Social System
Examples of social systems which promote diffusion and impact implementation and adoption of the NSSP document are professional and employment organizations, such as the ANA and healthcare and academic institutions respectively. Within the ANA professional organization enterprise, the American Nurses Credentialing Center (ANCC) facilitates the adoption of the NSSP and other foundational documents through credentialling and recognition programs. The NSSP serves as a resource for every content expert panel creating specialty nursing certification examinations and associated content outlines and learning materials. These program frameworks promote a culture of nursing excellence and support a quality professional practice environment in healthcare organizations (Cosme et al., 2021).
The ANCC Magnet Recognition Program (n.d.) which promotes excellence in nursing practice, including the practice environment, requires evidence of outcome in alignment with a nursing professional practice model (PPM). A PPM is a schematic that guides nursing practice and is based on the fundamental values of nursing (Hoffart & Woods, 1996). The NSSP document reflects the values of nursing and is covertly or overtly a structural, process, and/or outcome component of nursing PPMs. The ANA NSSP and other foundational documents are either named directly in the PPM schematic diagram or indirectly through professional role elements (Silverstein & Kowalski, 2017). ANA, as the professional nursing organization for nurses across the U.S., bridges the NSSP document to expectations for nursing practice, promoting a culture of nursing excellence and supporting a professional practice environment in healthcare organizations (Cosme et al., 2021).
...participants indicated that 25% of awareness methods for the document was through a nursing instructor.Academic institutions offering undergraduate and graduate nursing degrees vary in the caliber of their incorporation of content from ANA foundational documents within their academic and practice venues, and may elect to use ANA NSSP document and/or related professional development educational resources. In this study, participants indicated that 25% of awareness methods for the document was through a nursing instructor. Integration of the standards document(s) in schools of nursing curricula received the highest percentage of coding in the educate strategy theme. Nurse educators may request complimentary copies of the foundational documents for professional review and incorporation into curriculum.
Partnerships between professional organizations and regulatory agencies, such as state boards of nursing, may also influence adoption of the NSSP document. The Tri-Council for Nursing (National Council of State Boards of Nursing, 2016) comprised of the American Association of Colleges of Nursing, ANA, the American Organization of Nurse Executives, the National League for Nursing, and the National Council of State Boards of Nursing, developed a uniform nursing practice decision-making framework for RNs based on professional nursing scope and standards to promote patient safety. In addition to the Nurse Practice Act, the framework references two ANA foundational documents, the NSSP and the Code of Ethics for Nurses.
Organizational, cultural, social, political, and economic factors can also positively or negatively influence implementation and adoption...For organizations that employ nurses such as hospital, academic, government, ambulatory, and public health settings, formal and informal leaders within the organization influence the adoption of the NSSP document. Within the organizational social systems, evidence that the innovation fulfills a need is assessed by stakeholders who will decide on whether to adopt the innovation (Warty, et al., 2021). These influential individuals play a role in diffusion and implementation when they decide to adopt, communicate it to others, and change systems (Dearing & Cox, 2018). Organizational, cultural, social, political, and economic factors can also positively or negatively influence implementation and adoption (Chaves, et al., 2021). Observability of leaders communicating, educating, and demonstrating use of the document and embedding elements into organizational frameworks strengthens the confirmation phase of the RDI innovation-decision process.
Several limitations in this study include the lack of previous research and evidence on the diffusion and adoption of the NSSP documents, the sampling strategy, which may have contributed to the underrepresentation of respondents from some states and overrepresentation from academia and APRNs. A survey method that included self-reporting and use of skip logic may have inherent issues such as bias and malfunction respectively, and investigator biases were possible, given all were members of a specialized committee on the NSSP document. Generalizability is affected due to these limitations and study design. Recommendations for future research include correlating dissemination and awareness methods for the NSSP document with implementation and adoption, describing if and how organizations are integrating the NSSP document in practice, and examining the impact of adoption of the NSSP document on nurse, patient, and organizational outcomes.
Conclusion
For nursing to be a healthy profession, a scope and standards of practice must be defined.For nursing to be a healthy profession, a scope and standards of practice must be defined. This study was undertaken to determine the diffusion and adoption of the ANA NSSP documents in the United States. Despite high agreement levels among respondents on purpose of and need for the document, findings revealed the NSSP document was not widely diffused or adopted. Awareness, the first criteria for diffusion, was found to be both a barrier and a needed strategy. Key strategies for dissemination and implementation of the NSSP document include communicating, educating, demonstrating, and integrating. Observability, a key component for adoption, had a low agreement level for making a difference in one’s own and a peer’s practice. Positive nurse, patient, and organizational outcomes from document use will support confirmation and adoption.
This research provides initial knowledge and new insights on the diffusion and implementation/adoption of the ANA NSSP document. Findings can assist nurses in all roles and settings, including professional organizations, to understand barriers, strategies, and outcomes to implementation or adoption of the document. This stimulates professional advocacy, generates creative approaches, and helps further advance the nursing profession.
Acknowledgements
The research team was comprised of members of the ANA Committee on Nursing Practice Standards and included:
Verna Sitzer, PhD, RN, CNS
Danette Culver, MSN, APRN, ACNS-BC, CCRN-K, RN-BC
Renee Gecsedi, MS, RN
Deedra Harrington, DNP, RN, APRN, ACNP-BC
Richard Henker, PhD, RN, CRNA, FAAN
Carla Lee, PhD, ARNP-BC, CNAA, FAAN
Carol J. Bickford, PhD, RN-BC, CPHIMS, FAMIA, FHIMSS, FAAN
Authors
Verna Sitzer, PHD, RN, CNS
Email: Verna.sitzer@sharp.com
Verna Sitzer is Director of Professional Practice, Research, and Innovation at Sharp Memorial Hospital in San Diego, CA. She served on the American Nurses Association Committee on Nursing Practice from 2014-2020. Her many years of experience as a clinical nurse specialist, Magnet program director, and formal leader has provided ongoing opportunities to advocate for embedding professional practice standards into nursing practice structures, and processes.
Danette Culver, MSN, APRN, ACNS-BC, CCRN-K, RN-BC
Email: Danette.culver@nortonhealthcare.org
Danette Culver is Director of Clinical Effectiveness at Norton Healthcare in Louisville, KY. She has served on the American Nurses Association Committee on Nursing Practice Standards since 2015. In addition to her work on this committee, Danette’s professional role allows her to advance nursing practice within Norton Healthcare’s system through evidence-based practice and process improvement strategies.
Carol J. Bickford, PhD, RN-BC, CPHIMS, FAMIA, FHIMSS, FAAN
Email: carol.bickford@ana.org
Carol Bickford is the American Nurses Association senior policy advisor, has facilitated the Committee on Nursing Practice Standards activities and operations for over 20 years. These efforts included extensive development and writing of scope and standards documents, oversight of the review and revision of four editions of Nursing: Scope and Standards of Practice, and extensive consultation and review of over 60 specialty nursing scope and standards development efforts.
References
American Association of Colleges of Nursing. (2021). Concept across domains: Ethics. https://www.aacnnursing.org/essentials/database/kit/i/c_eth_wg_xls
American Nephrology Nurses Association. (2017). Nephrology nursing scope and standarsda of practice, 8th edition. American Nephrology Nurses Association.
American Nurses Association. (1973). Standards of nursing practice. American Nurses Association.
American Nurses Association. (1987). The scope of nursing practice. American Nurses Association.
American Nurses Association. (1991). Standards of clinical nursing practice. American Nurses Association.
American Nurses Association. (1996). Scope and standards of advanced practice registered nursing. American Nurses Publishing.
American Nurses Association. (1998). Standards of clinical nursing practice, second edition. American Nurses Publishing.
American Nurses Association. (2004). Nursing: Scope and standards of practice. Nursesbooks.org.
American Nurses Association. (2010). Nursing: Scope and standards of practice, 2nd edition. Nursesbooks.org.
American Nurses Association. (2014). Nursing informatics: Scope and standards of practice, 2nd edition. Nursesbooks.org.
American Nurses Association. (2015a). Code of ethics for nurses with interpretive statements. Nursesbooks.org.
American Nurses Association. (2015b). Nursing: Scope and standards of practice, 3rd ed. Nursesbooks.org.
American Nurses Association. (2016). Clinical research nursing: Scope and standards of practice. Nursesbooks.org.
American Nurses Association Enterprise. (n.d.). 2020-2023 Strategic Plan. One vision, one mission. https://www.nursingworld.org/ana-enterprise/about-us/anae-strategic-plan-2020---2023/
American Nurses Credentialing Center. (n.d.). ANCC Magnet Recognition Program®. https://www.nursingworld.org/organizational-programs/magnet/
Chaves, B. G., Briand, C., & Bouabida, K. (2021). International Journal of Health Research and Innovation, 9(1), 1-14. https://doi.org/10.47260/ijhri/911
Cosme, S., DeGarmo, S., Graebe, J., Horahan, M., Lal, M. M., & Pabico, C. G. (2021). A framework for nursing excellence. The Journal of Nursing Administration, 51(2), 55-57. http://doi.org/10.1097/NNA.0000000000000968
Dearing, J. W., & Cox, J. G. (2018). Diffusion of innovations theory, principles, and practice. Health Affairs, 37(2), 183-190. http://doi.org/10.1377/hlthaff.2017.1104
Gomez, N. J., Castner, D., & Hain, D. (2017). Nephrology nursing scope and standards of practice: Integration into clinical practice. Nephrology Nursing Journal, 44(1), 19-26.
Herena, P., Paguio, G., & Pulone, B. (2018). Clinical research nurse education: Using scope and standards of practice to improve care. Clinical Journal of Oncology Nursing, 22(4). http://doi.org/10.1188/18.CJON.450-452
Hsieh, H. F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687
Hoffart, N., & Woods, C. Q. (1996). Elements of a nursing professional practice model. Journal of Professional Nursing, 12(6), 354-364. https://doi.org/10.1016/S8755-7223(96)80083-4
IBM Corp. (2016). IBM SPSS Statistics for Windows, Version 24.0. IBM Corp.
Kouzes, J. M., & Posner, B. Z. (2016). Learning leadership: The five fundamentals of becoming an exemplary leader. Wiley.
Marion, L., Douglas, M., Lavin, M., Barr, N., Gazaway, S., Thomas, L., & Bickford, C. (2017). Implementing the new ANA standard 8: Culturally congruent practice. The Online Journal of Issues in Nursing, 22(1). https://doi.org/10.3912/OJIN.Vol22No01PPT20
Matthews, J. H., (2012). Role of professional organizations in advocating for the nursing profession. The Online Journal of Issues in Nursing, 17(1), 3. https://doi.org/10.3912/OJIN.Vol17No01Man03
McCormick, K. A., & Calzone, K. A. (2017). Genetic and genomic competencies for nursing informatics internationally. In J. Murphy et al. (Eds.), Forecasting informatics competencies for nurses in the future of connected health (pp. 152-164). IMIA and IOS Press. http://doi.org/10.3233/978-1-61499-738-2-152
National Academies of Sciences, Engineering, and Medicine. (2021). The future of nursing 2020-2030: Charting a patient to achieve health equity. The National Academies Press. https://doi.org/10.17226/25982
National Council of State Boards of Nursing. (2016). Scope of practice decision-making framework. https://www.ncsbn.org/decision-making-framework.htm
Phillips, J., Malliaris, A. P., & Bakerjian, D. (2021). Nursing and patient safety. https://psnet.ahrq.gov/primer/nursing-and-patient-safety
Rogers, E. M. (2003). Diffusion of Innovations, 5th Ed. Free Press.
Silverstein, W., & Kowalski, M. O. (2017, September). Adapting a professional practice model. American Nurse. https://www.myamericannurse.com/adapting-professional-practice-model/
Sipes, C., Hunter, K., McGonigle, D., West, K., Hill, T., & Hebda, T. (2017). The health information technology competencies tool. Does it translate for nursing informatics in the United States? Computers, Informatics, Nursing, 35(12), 609-614. http://doi.org/10.1097/CIN.0000000000000408
Smiley, R. A, Ruttinger, C., Oliveira, C. M., Reneau, K. A., Silvestre, J. H., Alexander, M. (2021). The 2020 National Nursing Workforce Survey. Journal of Nursing Regulation, 12(1) supp, S1-S96. https://doi.org/10.1016/S2155-8256(21)00027-2
Survey Monkey. (2016). Home page. http://www.surveymonkey.com
Warty, R. R., Smith, V., Salih, M., Fox, D., McArthur, S. L., & Mol, B. W. (2021). Barriers to the diffusion of medical technologies within healthcare: A systematic review. IEEE Access, 9, 139043-139058. https://doi.org/10.1109/ACCESS.2021.3118554


