Autism spectrum disorder (ASD) occurs in approximately 1 in 44 children in the United States. As the pediatric population of individuals with an ASD age, and prevalence of ASD continues to trend upward, nurses who care for adults and older adults can expect to see a steadily increasing percentage of patients affected by an ASD. Individuals and families affected by this complicated and heterogeneous neurological disorder grapple with a wide range of social and behavioral impairments as well as substantial medical and psychological comorbidities, making nursing care complex and multi-faceted. Individuals with an ASD comprise a vulnerable population with a markedly reduced life expectancy of nearly 36 years. This article reviews foundational information about the essentials of ASD, such as the definition and characteristics and discusses research about ASD and aging. We have created an embedded case study throughout the discussion that offers an exemplar based on evidence related to functionality, comorbidities, family centered care, and becoming informed through descriptions of the moment experience. Finally, we discuss implications for person-centered care for those with ASD that consider practice, education, research, and nursing administration.
Key Words: Autism Spectrum Disorders, aging, adulthood, person-centered care, nursing interventions, Autism Healthcare Accommodations Tool (AHAT), Vial of LIFE, communication, comorbidities
...healthcare providers can expect to see an increase in the population of adults and older adults with an ASD across all care settings.The diagnosis of autism is over 70 years old, and those earliest diagnosed children are now experiencing later life. However, there is limited data about the population of individuals with an autism spectrum disorder (ASD) over the age of 65 (Hand et al., 2020). Although the rate of ASD continues to climb, with 1 in 44 children receiving a diagnosis of ASD by age 8 years old in 2018 (Centers for Disease Control and Prevention [CDC], 2022), information about ASD in adults and older adults remains sparse. Current prevalence of an ASD in adults 18–84-year-old is 2.2% (Dietz et al., 2020). The number of patients seen in the Emergency Department having a coexisting diagnosis of an ASD doubled in a 5-year study period (Vohra et al., 2016). Given this upward trend in the prevalence of an ASD diagnosis, healthcare providers can expect to see an increase in the population of adults and older adults with an ASD across all care settings. Additionally, it is possible that there is a substantial pool of aging adults with undiagnosed autism who are “missing” from the prevalence statistics. There is some evidence to suggest that these missing adults may be incarcerated and/or homeless (Demer, 2018).
The frequency of the diagnosis of an ASD in children has prompted a plethora of research related to knowledge about the lived experiences of having an ASD in the pediatric realm; this has resulted in a substantial database of information for younger populations. However, ASD research focused on adults and older adults remains limited (Edelson et al, 2021; Wright et al., 2019). Literature findings do indicate that individuals with an ASD, across all levels of intellectual ability, experience substantial increased rates of medical and psychiatric comorbidities. These individuals may have a lifespan reduced by as many as 36 years when compared with individuals without an ASD (Guan & Li, 2017; Hand et al., 2020).
...ASD research focused on adults and older adults remains limitedAs the community of aging adults with an ASD continues to grow, information specific to ASD in older populations is needed in the nursing literature. A repository of information specific to individuals within this subset of the ASD community will better prepare nurses to provide adequate person-centered care for optimal aging in older adults with an ASD. The purpose of this article is to present findings from the existing literature about adult and older adults with a diagnosis of an ASD and to discuss implications for nurses in an aim to optimize care for this vulnerable population. While the focus of this article is the intersection of aging and autism, some work with young adult participants, or studies about individuals with an intellectual disability are included as this is often the only literature available.
In its updated position statement on providing care to people with intellectual and developmental disabilities (IDD), the American Nurses Association (ANA) advisory board states: “nurses must provide compassionate, comprehensive, and person-centered care to all people, inclusive of at-risk populations such as people with IDD…” (ANA, 2020, para 3). The position statement further addresses challenges including a family perspective and attention to caregivers, as well as palliative care. The new American Association of Colleges of Nursing ([AACN], 2021) Essentials, a guide which describes standards for nursing curriculum, provide clarity on person-centered care. AACN defines person centered care as focusing on “...the individual within multiple complicated contexts, including family and/or important others” (2021, p. 10). These perspectives are essential for nurses as they strive to improve disparities in health outcomes for individuals and families as they age with an ASD diagnosis.
Background
ASD: Definition and Characteristics
ASD encompasses a broad scope of behavioral, developmental, and social disorders that can present in various ways and are categorized in a progression ranging from mild to severe (American Psychiatric Association [APA], 2013). Diagnoses such as Asperger’s syndrome, pervasive developmental delays, and autistic disorder are included on the spectrum of ASD (APA, 2013). As defined in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (APA, 2013; CDC, 2022), a person who has “persistent deficits in social communication and interaction” (para 3) and a minimum of two types of repetitive behaviors, meets the criteria for an ASD. Key identifying characteristics of an ASD are related to social and behavioral patterns typically noticed in childhood but can be diagnosed for the first time in adulthood. Central to an ASD is a disruption in social abilities and repetitive behaviors.
Central to an ASD is a disruption in social abilities and repetitive behaviors.Individuals falling on the ASD spectrum often exhibit social behaviors related to ineffective communication or difficult interactions with others (APA, 2013). Although the occurrence of these traits and their severity vary from person to person, the resulting impaired functioning related to the behaviors makes these traits an identifying feature of ASD. Another common phenomenon among individuals with an ASD is difficulty with unfamiliar or overly stimulating environments, for instance, loud noises, frequent movement, and bright lights. These elements can cause uneasiness. Some individuals will cope with unfamiliar circumstances or stressful events by engaging in repeated behaviors or patterns known as “stimming” (Nicolaidis et al., 2014). While patterns of behavior are quite individual, behaviors typically associated with ASD impair functioning to a varying degree (APA, 2013).
The presence of an ID adds an additional layer of complexity to care...One more element of ASD is the presence of a comorbid intellectual disability (ID). There remains some debate about the extent to which individuals with an ASD have an ID, however, the presence or absence of intellectual impairment is a specifying feature in a diagnosis of ASD, according to the DSM-V (Thurm et al., 2019). The presence of an ID adds an additional layer of complexity to care, ranging from interventions to improve functioning to government resources to financially support the individual and ultimately the ability to live in the least supported environment possible (Thurm et al., 2019).
Research about ASD and Aging
Funding for research across the lifespan of the individual with autism remains deprioritized (Interagency Autism Coordinating Committee [IACC], 2021), leaving the nursing profession with a paucity of understanding when it comes to specific needs of aging adults with autism. Since this gap was identified by the IACC in 2018, the pool of knowledge is rapidly expanding with several new studies published in 2020 and 2021. The literature on aging and ASD can be divided into four categories: comorbidities, functionality and two areas providing information for nurses working to provide person-centered care, family-centered work and the lived experience. The following case study, a composite based on the authors’ experiences, will be used as an exemplar to discuss the complex care for an aging individual with an ASD, while presenting substantiating relevant literature.
Embedded Case Study
JD is a 60-year-old male admitted to the hospital with diabetic ketoacidosis (DKA). He suffers from stage II chronic kidney disease, Type II diabetes, a seizure disorder, hypertension, and he has an ASD. Upon admission, JD tells the nurse that he takes his blood pressure medications only if he has a headache and that he lives with friends in independent housing. His mother, who is 84 years old, lives nearby and provides support such as help with grocery shopping, trips to medical providers and finances. His father is deceased.
The nursing staff has limited knowledge of ASD and avoids JD.During his hospitalization, JD responds slowly to the nurse and consistently experiences poor sleep. When procedures such as blood draws, finger sticks, and vital signs are performed, JD frequently begins to rock and sometimes taps his head. These behaviors impede the nurse from completing assessments. JD needs frequent reminders in self-care and hygiene. The nursing staff has limited knowledge of ASD and avoids JD. The next sections provide information that will help inform nurses and about JD’s behaviors and provide strategies for optimal care.
Functionality
Because ASDs are varied in terms of symptomatology and functional capability, nurses may find a range in ability to perform activities of daily living (ADLs) and participate in medical self-management. For young adults, 87% will be living with family or in supported housing (Anderson et al., 2014). Some adults will approach their senior years living with minimal support, while others may need substantial assistance, requiring a caregiver at home or living in supervised housing. Aside from basic ADLs (e.g., bathing, cooking, dressing), individuals may need help with transportation, access to healthcare, and managing financial and legal responsibilities. In a survey of 715 family members of an individual with an ASD living at home, 88% required help with some basic functions (Roux et al., 2021). Further, in a study of a small sample of Australian individuals with an ASD, only 3% met the criteria for ‘aging well’ (Hwang et al., 2017).
Access to healthcare can be a substantial challenge for individuals and families affected by ASD.Access to healthcare can be a substantial challenge for individuals and families affected by ASD. Gerber et al. (2017) found that in a small sample (n = 94) of adults with autism, 60% of participants needed assistance to obtain medical care. Several barriers to primary care were noted in a sample of 392 individuals with autism, including communication difficulty, anxiety, worry about cost, and difficulty managing sensory stimuli (Raymaker et al., 2017). Thus, the nurse should carefully assess JD’s current level of functionality, ability to interact with healthcare providers and challenges to meet medical needs consistently. The nurse should also anticipate that JD may not receive essential services such as regular screening, nutrition counseling, and monitoring of his chronic conditions.
...some data suggest that functionality, daily functioning, and ability to work, may not decrease much over timeDespite the substantial level of medical and psychiatric comorbidity in adults and seniors (see next section), some data suggest that functionality, daily functioning, and ability to work, may not decrease much over time (Wise et al., 2020). Another study with participants who were all over 60 years of age noted that objective measures of executive function (e.g., planning, impulse control, and working memory) were no different between participants with an ASD and those without. However, the participants with an ASD reported subjectively higher levels of difficulty with executive function (Geurts et al., 2020). Thus, the older adults with an ASD may lack self confidence in their ablity to complete self-care activities such as medication management or self-monitoring of blood pressure or glucose. Another element to consider is JD’s ability to swallow medication because patients with autism may have difficulty related to color and texture of pills (Quiban et al., 2020).
A plan of care tailored to JD’s existing routine and individual capability might yield greater success. Given JD’s level of functioning, the nurse might further consider technologies that would assist JD in tracking his blood sugar. For example, upon discharge, FreeStyle Libre, a continuous glucose monitoring system that has been associated with convenient, cost effective, and accurate management of blood sugar levels, may be used with the LibreLink mobile application to record trends in blood glucose levels (Jaiswal et al., 2021; Leelarathna & Wilmot, 2018). Data can be transmitted to several devices, alerting caregivers to changes in glycemic control.
Comorbidities
Medical and psychiatric conditions or comorbidities are common in individuals with an ASD (Miot et al., 2019), often requiring complicated medication regimens. In a longitudinal study of 92 individuals with an ASD, spanning 30+ years, Jones et al. (2016) found an average of 11 comorbid conditions per participant. Certainly, in the case of JD, there are numerous comorbid conditions that affect his health and complicate his care. As members of the autistic community age, some medical concerns are likely to be extensions of pediatric/adolescent problems and other conditions may relate to the aging process.
Medical and psychiatric conditions or comorbidities are common in individuals with an ASD...Comorbidities that appear to persist beyond childhood include gastrointestinal issues such as constipation, seizure disorders, and sleep disruption (Jones et al., 2016; Miot et al., 2019). Risk for infection appears higher as well (Zandam et al., 2022). Other conditions are related to aging but appear to occur at rates far higher among individuals with an ASD than in the general population. These conditions include hypertension, hip fracture (e.g., 11 times greater risk in women with an ASD) and Parkinson’s disease (Hand et al., 2020; Jones et al., 2016; Neumeyer et al., 2015). Table 1 highlights the risks and sequelae that commonly occur related to comorbidities in older adults with an ASD.
Table 1. Comorbidities and Implications
|
Comorbidity |
Estimated Prevalence or Increased Risk ASD (%) |
Estimated Prevalence or Increased Risk Control (%) |
OR |
Potential Impact |
|
Seizure Disorders |
26.4 |
1.9 |
18.9 |
↑ risk injury |
|
Parkinson’s Disease |
6.6 |
1.2 |
6.1 |
↑ risk of falls, dementia, pneumonia |
|
Depression |
35.9 |
9.1 |
5.6 |
↓ quality of life, ↑ risk of polypharmacy and suicide |
|
Thyroid Disorders |
31.7 |
13.8 |
3.1 |
↑ risk polypharmacy and lab tests |
|
Obesity |
14.4 |
10.3 |
3.1 |
↑ risk for cardiovascular disease; osteoarthritis, cancer |
|
Osteoporosis |
16.6 |
4.9 |
4.4 |
↑ risk for fracture, reduced mobility, pain |
|
Constipation |
51.2 |
17.6 |
5.2 |
↓ quality of life, ↑ risk of polypharmacy |
|
Heart Disease |
54.2 |
51.2 |
2 |
↑ risk of high cost/intensity care and early mortality |
Early screening and intervention in the acute care setting, as well as effective transition of care to the home, are vital to prevent an exacerbation of these sequelae. For nurses working with JD, monitoring for increased risk of injury and decreased quality of life could preempt some of these sequelae. Understanding that JD may face increased cost of care should act as a trigger for early intervention by a case manager and social worker. All
With regard to psychiatric conditions (e.g., bipolar disorders, anxiety, depression, dementia) in aging individuals with an ASD, there is wide variability and often contradictory information. In a sample of adult Medicaid recipients, Vohra et al. (2016), found rates for depression to be lower in those with an ASD (Odds Ratio, 0.9, N.S.). However, in one of the largest studies to date, Hand et al. (2020) examined the Medicare billing database for information about comorbidities in individuals 65 years of age or older and their findings supported the fact that these conditions are more common in individuals with ASD, affecting nearly 75% of the sample. There is also evidence, however, that late life does not bring an ever-increasing prevalence of these disorders (Lever & Geurts, 2016).
increased cost of care should act as a trigger for early intervention...All of these comorbidities complicate residential and medical care and lower quality of life. Some conditions increase risk for secondary comorbidities. For example, osteoporosis increases the risk of fractures. Since many of these conditions are treated pharmacologically, aging individuals with an ASD increasingly face polypharmacy, which itself increases risks for side effects, organ damage, drug-drug interactions, medication non-adherence and cost burden (Jones et al., 2016; Miot et al. 2019). Side effects from medications can worsen existing comorbidities such as depression, constipation, or obesity. These issues, combined with accidents, may explain the fact that individuals with ASD have a life expectancy nearly 30 years younger than non-affected individuals (Guan & Li, 2017).
Medication reconciliation and careful monitoring for side effects and drug interactions is particularly critical...However, there is also promising news. According to Medicare data, seniors with ASD do not have an increased prevalence of substance use (Hand et al., 2020). This is particularly important considering that many health-related problems in senior years (and in fact the leading causes of death in the United States, cancer, heart disease and respiratory disease), are frequently associated with lifestyle habits such as smoking, alcohol and other substance use (Danaei et al., 2011; Kochanek et al., 2020). In fact, rates of cancer appear minimally elevated in persons with ASD when compared to a matched sample of individuals without an ASD (Hand et al., 2020). Connecting JD for primary care follow-up with providers who understand the complexities and comorbidities associated with an ASD, and an interdisciplinary team that can address barriers to care, may lead to improved outcomes and a reduced likelihood of readmission. Medication reconciliation and careful monitoring for side effects and drug interactions is particularly critical in JD’s care.
Family-Centered Work
As many individuals with an ASD require some level of support during their lives, inclusion of a family perspective in the aging process is essential for a person-centered and holistic view. The literature indicates that family members do not feel well supported as they care for young adults with an ASD (Turcotte et al., 2016). Transition into later life for individuals with an ASD is a daunting period for families and caregivers. Parents experience worry related to the unknown and the burden of planning for their child’s future needs (Chamak & Bonniau 2016).
The literature indicates that family members do not feel well supported as they care for young adults with an ASDHerrema et al. (2017), surveyed 120 parents of adults with ASD and found that more than half worried weekly about their child’s happiness, future needs and potential caregiver once they were no longer alive. A qualitative study of interviews with 51 midlife parents (predominantly mothers) of adults with ASD provides further confirmation that parents worry about who will care for their child with an ASD after they die (Marsack-Topolewski & Graves, 2020). This worry is not limited to who the caregiver will be, but also the quality of care that will be provided. Many participants in this study voiced a previously expressed idea in the literature that parental skill in care is unique, effective, and related to years of relationship building with an adult child. In sum, the parent is irreplaceable. Because of the paucity of available options, parents often failed to plan in part because the future was “difficult to imagine” (Marsack-Topolewski & Graves, 2020, p. 77).
In sum, the parent is irreplaceable.To gain a family perspective in the care of JD, the nurse includes JD’s mother in conversations about how best to support and care for him during the hospital stay. The nurse learns that JD’s mother is in reasonable health and lives independently. The nurse also learns that JD’s mother is his legal guardian and healthcare proxy, and JD’s sibling (without an ASD) is co-guardian. Although JD’s mom is not involved in his day-to-day care, she helps fill his pillbox on a weekly basis and accompanies JD to neurology visits because seizure management is a priority. JD’s mom notes that he typically taps on his head when the environment is too loud. The nurse further learns that JD often phones his mother at night before bed, but that the hospital stay has disrupted this routine. As part of JD’s sleep hygiene program, the nurse implements that cue at bedtime.
The Lived Experience
Despite difficulty in recruitment into formal research and a relative paucity of seniors formally diagnosed, there is some literature that explores the unique perspective of adults and seniors who carry an ASD diagnosis. Sample sizes in these studies are small, sometimes reflecting the experience of just one individual, yet the voice of those with an ASD is essential to understand how to provide support and care in late life and is an essential component of providing ethical care to those with any developmental disability (ANA, 2020). As nurses increasingly care for individuals with an ASD, they are likely to become more skilled. Until that happens, the following books and articles represent one way to increase personal knowledge.
As nurses increasingly care for individuals with an ASD, they are likely to become more skilled.Two qualitative studies provide insight regarding the lived experience of women with an ASD during childbirth delivery in an acute care setting. Women with ASD related difficulty communicating with nursing staff during delivery. Such difficulty led to increased anxiety and fear (Donovan, 2020; Lewis et al., 2021). Sensory overload and increased pain were noted to be related to poor communication, both in understanding the nursing staff and in feeling comfortable reporting or describing pain (Lewis et al., 2021).
Women with ASD related difficulty communicating with nursing staff during delivery. Lawson (2015), a ‘highly functioning’ individual with an ASD, has written what appears to be the only ‘guide’ for individuals with an ASD as families and caregivers assist in navigating later years. The book contains different individuals' perspectives on aging. Central worries included social isolation, the need for support, continuing need for individualized plans of care and consistency in quality of care. The overarching theme addresses the challenges of transitioning through late life and adjusting to normative losses typical in this life stage.
Another personal exploration is found in the work of Deborah Lipsky (2013), who explains how individuals with autism spectrum conditions may process loss. Ms. Lipsky, a high functioning individual with autism, has witnessed loss as a firefighter and EMT. Although the book represents one individual's viewpoint, it is well organized and inclusive, and provides insight about the topic of loss, an area that remains largely unexplored in the autism literature. Themes presented include difficulty with change after loss; increased anger related to inexpressible emotion; and difficulty in handling stimulation associated with routine grieving rituals. Common sense advice, such as having a plan in place in advance of expected losses (e.g., pets, terminally ill friends or family), may help nurses to guide care. Nurses caring for JD must be mindful of his mother’s advanced age and recall, at the very least, that JD’s sleep routine is tied to his mother’s presence in his life. In case of a loss, screening for complicated grief is an integral part of providing person centered care for the aging individual with an ASD.
Nurses caring for JD must be mindful of his mother’s advanced age and recall...Additional voices from the ASD community can be found sporadically in the literature. Barber (2017) included brief interviews with three individuals with an ASD in a study that explored how healthcare professionals can meet needs of the community. Findings from this study are consistent with the literature: adult and older adult healthcare providers and service agencies have limited knowledge about ASD and the care required by aging adults with an ASD. There is consensus that given the substantial heterogeneity of ASDs, interventions and care must be deeply personal. Thus, the nursing team caring for JD continues to ask questions about individual preferences and experiences, as well as seeking information from the literature and interdisciplinary experts.
Implications for Person-Centered Care
Implications for Nursing Practice
...while primary care of seniors with autism will need to be tailored specifically for individual needs, accommodations are possible.Individuals with an ASD across the age continuum are more likely to be hospitalized and have more complex medical regimens (Jewitt, 2017; Miot et al., 2019). High quality primary care, preferably in settings that are well versed in the care of aging adults with ASD, may provide one possible strategy for prevention of longer-term problems and reduce hospitalization. Saqr et al. (2018) found that young adults with an ASD were accommodated in a standard primary care setting by using a pre-visit telephone screening. These findings suggest that while primary care of seniors with autism will need to be tailored specifically for individual needs, accommodations are possible.
...individuals with an ASD often experience difficulty communicating their health history, especially in unfamiliar environments...When caring for someone with an ASD, as with any other patient, nurses must understand the patient's current state of health and past medical history. However, individuals with an ASD often experience difficulty communicating their health history, especially in unfamiliar environments such as a hospital setting. First, nurses must acknowledge and understand the patient's diagnosis of an ASD; in doing so, nurses allow patients to be active and capable participants in their care. Individuals with an ASD or ID often share their feeling that nurses and providers overlook them throughout care due to their diagnosis; they report feeling that they receive a low level of care (Smeltzer et al., 2012; Weir et al., 2022). Allowing patients with an ASD to participate in their care and health decisions is a critical element of patient centered care (AACN, 2021). To promote effective patient participation, nurses must inquire about patients’ abilities and preferences with the routine medical history.
Obtaining a history from an individual with an ASD may be difficult, but there is one standardized resource available. The Academic-Autistic Spectrum Partnership in Research and Education (AASPIRE, 2022) offers a toolkit that allows individuals with autism to personalize a report that can be given to clinicians prior to or during visits or hospital stays. The report is created using the Autism Healthcare Accommodations Tool (AHAT) and provides pertinent information about the individual and any care needs.
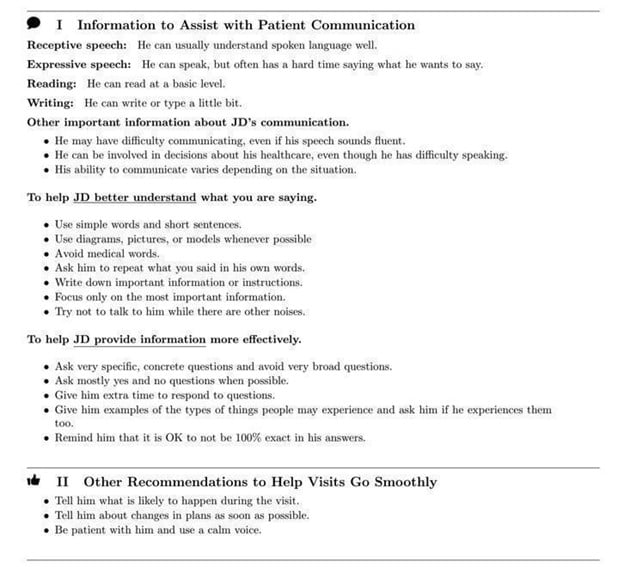
Providers using the AHAT should share the AASPIRE website with the patient and family (AASPIRE, 2022). Once logged in, patients or families answer a series of questions about how they communicate (e.g., verbal, written), what actions are stressful during a health visit (e.g., blood draws), and how they may respond (e.g., stimming behaviors). The AHAT algorithm produces an individualized report for the patient/family and healthcare provider with specific clinical suggestions (AASPIRE, 2022). Suggestions cover guidance ranging from communication (e.g., decreasing background noise) to how to help an individual with ASD tolerate an exam (e.g., let the individual practice with equipment) to strategies for adherence to healthcare interventions (e.g., use pictures). Use of the AHAT in primary care settings improves provider confidence and patient satisfaction (Nicolaidis et al., 2016).
Use of the AHAT in primary care settings improves provider confidence and patient satisfaction The Figure shows a snapshot from JD’s AHAT, which he was able to create with help from the nurse during his hospital stay. For his full AHAT report, click on the Supplemental Material link below. Upon initial assessment, JD indicated that he did not have an AHAT, but expressed interest in creating one after the nurse explained the document. The nurse assisted JD to create his personalized report, along with his “All About Me” board, allowing him to be an effective partner in his care (Fick et al., 2013).
Figure.
Excerpt from JD’s AHAT
Supplemental Material: Full AHAT Report
Another tool that can offer healthcare providers and emergency responders with critical information about a patient’s health history is the Vial of LIFE (i.e., Lifesaving Information for Emergencies). This concise document, commonly used by older adults, helps responders access necessary basic medical information in emergencies, and includes such items as current medical history, an updated medication list, emergency contacts, resuscitation status, and a recent photograph (Turner et al., 2018). Persons who participate in this program place a decal on the front door of their house that alerts medical personnel to the presence of easily accessible information to assist in their care. Nurses should encourage patients to create personalized reports such as AHAT and Vial of LIFE to assure that communication preferences and medical needs are effectively addressed. Table 2 provides a list of resources for nurses and family members.
Table 2. Resources for Additional Information
|
Resource |
Website |
|
Academic-Autistic Spectrum Partnership in Research and Education (AASPIRE) 5 Ways to Improve Hospitals for Autistic Adults |
|
|
AASPIRE Autism Healthcare Accommodations Tool (AHAT) |
|
|
Vial of Life |
|
|
National Institute for Mental Health (NIMH) |
https://www.nimh.nih.gov/health/publications/autism-spectrum-disorder/ |
|
Interagency Autism Coordinating Committee |
In summary, to provide optimal, patient-centered care the nurse should:
● Acknowledge the patient when collecting pertinent information, regardless of the presence of a parent, guardian, or caregiver (Smeltzer et al., 2012).
● Include the patient and family or legal guardian in decision making.
● Use the Autism Healthcare Accommodations Tool (Nicolaidis et al. 2016).
● Reduce potential sensory overstimulation ( e.g., loud noises, bright lights, and or painful stimuli) that may cause anxiety, inability to focus, and maladaptive behavior (AASPIRE, 2022).
● Consider the need for alternative methods of pain assessment based on the patient’s ability for verbal communication and altered pain threshold (Clarke, 2015; Liu et al., 2020).
● Use an “All About Me” board, based on the patient’s AHAT if available (Johnson et al., 2021).
● Assess the patient’s ability to swallow medication (Quiban et al., 2020).
Outcome of Case Study. After his metabolic state stabilized, JD was discharged to home. Nurses included JD’s mother in discharge instructions to increase the likelihood of adherence to new medications and scheduled visits to specialists. JD was provided with the phone number of a local endocrinologist with experience in caring for individuals with an ASD and a copy of his AHAT. He learned to document his blood glucose every day using the mobile app which automatically communicated that level with his mother. Ultimately, JD and his mother began to include his sibling in assisting with his care and monitoring his health status as a way to transition to a time when JD’s mother might not be able to be the primary caregiver. Table 3 summarizes key goals and interventions in JD’s care.
Table 3. Sample Nursing Goals and Interventions for JD
|
Goal |
Possible Intervention |
|
Improve self-care skills |
● Assess current level of functionality ○ discuss current capabilities with parent/guardian ● Provide verbal cues for hygiene and ADLs ● Consider Occupational Therapy referral |
|
Reduce anxiety related to procedures/care |
● Use AASPIRE tool kit (with parent/guardian if necessary) ● Encourage appropriate comfort measures (e.g. weighted blanket or rocking in bed) ● Reduce sensory overstimulation ● Use alternatives to pain assessment such as NCCPC-R or QST |
|
Improve time asleep at night |
● Promote basic sleep hygiene measures: ○ accommodate nighttime rituals ○ out of bed in chair during day ○ consistent PM care |
|
Reduce regime non-adherence |
● Provide list of ASD knowledgeable primary providers ● Evaluate ability to swallow medication ● Patient-centered education (e.g. how to assess and manage blood glucose using FreeStyle Libre and the LibreLink mobile app) |
|
Decrease risk of injury and mitigate impact of comorbidities |
● Assess risk factors ● Medication reconciliation ● Monitor side effects of medications ● Assess signs and symptoms of exacerbation of medical conditions |
|
Long term health care planning |
● Family meeting(s) that include caregiver(s) and support systems ● Case management/social work referral |
Implications for Nurse Educators
The first priority for educators in adult and gerontology courses is to ensure that their personal knowledge is up to date. The only available study of nursing faculty knowledge (n = 164) found that while pediatric faculty had sufficient knowledge and confidence in the area of autism, the majority of those who specialize in adult care had poor knowledge. These faculty felt unprepared to teach others about care for individuals and families affected by an ASD (Gardner et al., 2016). Knowledge of nurses in practice is similarly low. A small survey of ER nurses (n = 29) found that aside from knowledge about diagnostic criteria (86% answered questions correctly), only about 66% of nurses had correct answers for general ASD knowledge questions (Miller, 2015).
The first priority for educators in adult and gerontology courses is to ensure that their personal knowledge is up to date. With the recent publication of new guidelines for nursing education, many faculty are now reviewing curricula to ensure that it meets competencies for the most recent AACN Essentials (AACN, 2021). This represents an opportunity to enhance preparation of nurses to care for persons and families affected by an ASD. The Essentials call for competency in entry level nurses in four ‘spheres’ of care: wellness, restorative, chronic disease management and palliative. Caring for adults and seniors with ASD can provide opportunities to develop competency in each of these spheres.
Caring for adults and seniors with ASD can provide opportunities to develop competency in each of these spheres.Clinical opportunities to care for adults and seniors with an ASD provide several areas for students to demonstrate required competency in the nine Essentials domains. For example, the knowledge for nursing practice domain may be met by demonstrating knowledge of co-morbidities; person-centered care is demonstrated by provision of extra supports and interventions; population health competencies are addressed by articulating need for sub-population level standards of care; and the need to treat this vulnerable population ethically demonstrates professionalism. The domain of person-centered care is particularly relevant in the care of those with an ASD as most such adults will be living with family or support. The International Family Nurses Association (IFNA) further directs educators that pre-licensure students should be able to integrate family needs in care, empower families, and be able to advocate for policies that address family needs (IFNA, 2013).
The domain of person-centered care is particularly relevant in the care of those with an ASD... From didactic knowledge to clinical and simulation experience, nurse educators have substantial opportunities to enhance the knowledge and skills of students (and themselves) to provide care for this vulnerable group. While information for evidence-based pedagogy in adults and seniors is limited, educators could use a pediatric simulation as a foundation to create scenarios that are developmentally appropriate for adult or older adult patients (McIntosh et al., 2018; Mitchell et al., 2020).
Implications for Nurse Researchers
There are several areas and approaches that remain poorly explored by nurse researchers. One area deserving of further research is pain assessment and pain management in adults with ASD. Pain may be experienced and expressed differently in these adults and existing measures may not adequately assess pain in this unique population (Clarke, 2015; Liu et al., 2020). Further, nurse researchers should examine the impact of using AHAT in an acute care setting to support nurse-patient communication and adherence to the plan of care for hospitalized patients with an ASD.
One area deserving of further research is pain assessment and pain management in adults with ASD. Rigorous quantitative evidence is needed to support practice and policy interventions. Suggestions for nurses in acute care settings include exploring patient satisfaction scores, frequency of refused care, falls and other incidents, and the impact of education on knowledge and confidence of nursing staff. Researchers in primary and community care may wish to explore novel interventions related to prevention of long-term sequelae from medications and comorbidities, as well as primary prevention strategies such as nutrition and exercise. Nurse researchers in long-term care can begin by building qualitative and quantitative databases regarding experiences of individuals with an ASD in long-term care settings. The need for research on the impact of other disparities (e.g., income, gender, race) remains paramount.
Implications for Nurse Administrators
Lastly, nurse administrators can assist in the effort to reduce the health disparities in the ASD community by supporting staff in these efforts and working toward implementing institutional policies that support evidence-based care. Understanding the budgetary impact of caring for older adults with an ASD will become increasingly important as the number of such persons in this age group increases. Encouraging staff members to increase their knowledge base in this area can create a cadre of nurses who can lead teams to care for this vulnerable population. Nurse administrators can collaborate with staff to analyze potential policies in such areas as staffing levels, standard use of the AHAT, and care policies that guide nurses to reduce stimulation levels.
Conclusion
It is likely that nurses across all care settings will see a steady increase in the percentage of patients and families affected by ASDs. The extant literature indicates that current nursing knowledge is not yet adequate to allow nurses to provide evidence-based care. Even more concerning is that the current lack of knowledge may be causing harm to patients (Donovan, 2020). This article has provided a glimpse into the evidence available and gaps in knowledge related to providing high quality person-centered care for those in the autism community. Thus, the article provides a sound starting point for those nurses unfamiliar with the ASD diagnosis.
It is likely that nurses across all care settings will see a steady increase in the percentage of patients and families affected by ASDs. All nurses must advocate for adequate funding for nursing research, education, and practice opportunities. Further advocacy is crucial for ample reimbursement to provide the level of complex, person and family-centered care that this vulnerable population deserves. The gaps in the literature and the documented poor outcomes for individuals with an ASD, such as a dramatically reduced life span, and preventable causes of death, are clear. The opportunity for nursing professionals to create, study, and implement evidence-based care models for these patients is promising and vast.
Authors
Connie Kartoz, PhD, RN
Email: kartoz@tcnj.edu
ORCID ID: 0000-0003-2650-1906
Connie Kartoz is an Associate Professor of Nursing at The College of New Jersey and a family nurse practitioner. She holds a BSN from the University of Pennsylvania, an MSN from Old Dominion University and a PhD from Seton Hall University, where she was a Robert Wood Johnson/New Jersey Nurse Initiative Scholar. Her research focus is intergenerational relationships in aging families and she is the co-author of the Parent Anticipatory Loss Scale. In addition to providing care for families with an ASD in her clinical practice, she works with a local Autism service organization to help identify optimal strategies for high quality of life as participants age.
Munira Wells, PhD, RN
Email: munira.wells@shu.edu
ORCID ID: 0000-0001-7360-388X
Munira Wells is an Associate Professor of Nursing at Seton Hall University. She holds a BSN and MSN from Kean University and a PhD from Seton Hall University, where she was a Robert Wood Johnson/New Jersey Nurse Initiative Scholar. Dr. Wells teaches adult health nursing courses, where she addresses care of individuals with developmental disability. Her research focus is qualitative methodology and intergenerational relationships in aging families and she is the co-author of the Parent Anticipatory Loss Scale.
Sara Muñoz
Email: muñozs5@tcnj.edu
ORCID ID: 0000-0003-2262-2751
Sara Muñoz is a senior nursing student at The College of New Jersey, where she was awarded a summer research fellowship to conduct qualitative research with parents of adult children with an autism spectrum disorder. She is also a Patient Care Technician at the Robert Wood Johnson Children's Specialized Hospital in New Brunswick, NJ.
References
AASPIRE.org. (2022). AASPIRE healthcare toolkit. Home. https://autismandhealth.org/?p=home&theme=ltlc&size=small
American Association of Colleges of Nursing (AACN). (2021). The essentials: Core competencies for professional nursing education. https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf
American Psychiatric Association (APA). (2013). Autism spectrum disorder. In: Diagnostic and statistical manual of mental disorders (DSM-5®), p. 50-59. ProQuest Ebook Central https://psychiatry.org/psychiatrists/practice/dsm
American Nurses Association (ANA) Ethics Board. (October 20, 2020). ANA position statement: Nurse’s role in providing ethically and developmentally appropriate care to people with intellectual and developmental disabilities" OJIN: The Online Journal of Issues in Nursing, 26(1). https://doi.org/10.3912/OJIN.Vol26No01PoSCol01
Anderson, K. A., Shattuck, P. T., Cooper, B. P., Roux, A. M., & Wagner, M. (2014). Prevalence and correlates of postsecondary residential status among young adults with an autism spectrum disorder. Autism: The International Journal of Research and Practice, 18(5), 562–570. https://doi.org/10.1177%2F1362361313481860
Barber C. (2017). Meeting the healthcare needs of adults on the autism spectrum. British Journal of Nursing, 26(7), 420–425. https://doi.org/10.12968/bjon.2017.26.7.420
Centers for Disease Control and Prevention (CDC). (2022). Data & statistics on autism spectrum disorder. ASD Homepage. https://www.cdc.gov/ncbddd/autism/data.html
Chamak, B., & Bonniau, B. (2016). Trajectories, long-term outcomes and family experiences of 76 adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(3), 1084–1095. https://doi.org/10.1007/s10803-015-2656-6
Clarke, C. (2015). Autism spectrum disorder and amplified pain. Case Reports in Psychiatry, 2015, 930874. https://doi.org/10.1155%2F2015%2F930874
Danaei, G., Ding, E. L., Mozaffarian, D., Taylor, B., Rehm, J., Murray, C. J. L., & Ezzati (2011). Correction: The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLOS Medicine, 6(4), e1000058. https://doi.org/10.1371/annotation/0ef47acd-9dcc-4296-a897-872d182cde57
Demer, L. L. (2018). The autism spectrum: Human rights perspectives. Pediatrics, 141(Suppl 4), S369–S372. https://doi.org/10.1542/peds.2016-4300O
Dietz, P. M., Rose, C. E., McArthur, D. & Maenner, M. (2020). National and state estimates of adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 50, 4258–4266. https://doi.org/10.1007/s10803-020-04494-4
Donovan, J. (2020). Childbirth experiences of women with autism spectrum disorder in an acute care setting. Nursing for Women's Health, 24(3), 165-17. https://doi.org/10.1016/j.nwh.2020.04.001
Edelson, S. M., Nicholas, D. B., Stoddart, K. P., Bauman, M. B., Mawlam, L., Lawson, W. B., Jose, C., Morris, R., & Wright, S. D. (2021). Strategies for research, practice, and policy for autism in later life: A report from a think tank on aging and autism. Journal of Autism and Developmental Disorders, 51(1), 382–390. https://psycnet.apa.org/doi/10.1007/s10803-020-04514-3
Fick, D. M., DiMeglio, B., McDowell, J. A., & Mathis-Halpin, J. (2013). Do you know your patient? Knowing individuals with dementia combined with evidence-based care promotes function and satisfaction in hospitalized older adults. Journal of Gerontological Nursing, 39(9), 2–4. https://doi.org/10.3928/00989134-20130809-89
Gardner, M. R., Suplee, P. D., & Jerome-D'Emilia, B. (2016). Survey of nursing faculty preparation for teaching about autism spectrum disorders. Nurse educator, 41(4), 212–216. https://doi.org/10.1097/NNE.0000000000000237
Gerber, A. H., McCormick, C. E. B., Levine, T. P., Morrow, E. M., Anders, T. F., & Sheinkopf, S. J. (2017). Brief report: Factors influencing healthcare satisfaction in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(6), 1896–1903. https://doi.org/10.1007/s10803-017-3087-3
Geurts, H. M., Pol, S. E., Lobbestael, J., & Simons, C. J. P. (2020). Executive functioning in 60+ autistic males: The discrepancy between experienced challenges and cognitive performance. Journal of Autism and Developmental Disorders, 50(4), 1380–1390. https://doi.org/10.1007/s10803-020-04368-9
Guan, J., & Li, G. (2017). Injury mortality in individuals with autism. American Journal of Public Health, 107(5), 791–793. https://doi.org/10.2105/AJPH.2017.303696
Hand, B. N., Angell, A. M., Harris, L., & Carpenter, L. A. (2020). Prevalence of physical and mental health conditions in Medicare-enrolled, autistic older adults. Autism: The International Journal of Research and Practice, 24(3), 755–764. https://doi.org/10.1177/1362361319890793
Herrema, R., Garland, D., Osborne, M., Freeston, M., Honey, E., & Rodgers, J. (2017). Brief report: What happens when I can no longer support my autistic relative? Worries about the future for family members of autistic adults. Journal of Autism and Developmental Disorders, 47(11), 3659–3668. https://doi.org/10.1007/s10803-017-3254-6
Hwang, Y., Foley, K. R., & Trollor, J. N. (2017). Aging well on the autism spectrum: The perspectives of autistic adults and carers. International Psychogeriatrics, 29(12), 2033–2046. https://doi.org/10.1017/s1041610217001521
International Family Nursing Association (IFNA). (2013). IFNA position statement on pre-licensure family nursing education. Retrieved from https://internationalfamilynursing.org/2015/07/25/ifna-position-statement-on-pre-licensure-family-nursing-education
Interagency Autism Coordinating Committee (IACC). (2021). 2017-2018 IACC autism spectrum disorder research portfolio analysis report. Publications. https://iacc.hhs.gov/publications/portfolio-analysis/2018/
Jaiswal, R., Zhang, M., Zuniga, S., & Myers, A. K. (2021). Integration of flash glucose monitoring during the transition of care from inpatient to outpatient settings in patients with type 2 diabetes. Journal of the Endocrine Society, 5(Suppl 1), A427–A428. https://doi.org/10.1210/jendso/bvab048.872
Jewitt, C. (2017, September 23). Nowhere to go: Young people with severe autism languish weeks or longer in hospitals. The Washington Post. https://www.washingtonpost.com/national/health-science/nowhere-to-go-young-people-with-severe-autism-languish-weeks-or-longer-in-hospitals/2017/09/23/25333dfc-997c-11e7-b569-3360011663b4_story.html
Johnson, K., Razo, S., Smith, J., Cain, A., & Detaranto, B. (2021). A person-centered nursing care intervention on a medical surgical unit. Geriatric Nursing, 42(5), 1125–1128. https://doi.org/10.1016/j.gerinurse.2021.06.029
Jones, K. B., Cottle, K., Bakian, A., Farley, M., Bilder, D., Coon, H., & McMahon, W. M. (2016). A description of medical conditions in adults with autism spectrum disorder: A follow-up of the 1980s Utah/UCLA Autism Epidemiologic Study. Autism: The International Journal of Research and Practice, 20(5), 551–561. https://doi.org/10.1177/1362361315594798
Kochanek, K. D., Xu, J., & Arias, E. (2020). Mortality in the United States, 2019 (NCHS Data Brief No. 395). National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db395.htm
Lawson, W. (2015). Older adults and autism spectrum conditions: An introduction and guide. Jessica Kingsley Publishers.
Leelarathna, L., & Wilmot, E. G. (2018). Flash forward: A review of flash glucose monitoring. Diabetic Medicine: A Journal of the British Diabetic Association, 35(4), 472–482. https://doi.org/10.1111/dme.13584
Lever, A. G., & Geurts, H. M. (2016). Psychiatric co-occurring symptoms and disorders in young, middle-aged, and older adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(6), 1916–1930. https://doi.org/10.1007/s10803-016-2722-8
Lewis, L.F., Schirling, H., Beaudoin, E., Scheibner, H., & Cestrone, A. (2021). Exploring the birth stories of women on the autism spectrum. Journal of Obstetric, Gynecologic, & Neonatal Nursing (JOGNN), 50(6), 679-690. https://doi.org/10.1016/j.jogn.2021.08.099
Lipsky, D. (2013). How people with autism grieve, and how to help: An insider handbook. Jessica Kingsley Publishers.
Liu, J., Chen, L. L., Shen, S., Mao, J., Lopes, M., Liu, S., & Kong, X. (2020). Challenges in the diagnosis and management of pain in individuals with autism spectrum disorder. Review Journal of Autism and Developmental Disorders, 7(4), 352–363. https://doi.org/10.1007/s40489-020-00199-7
Marsack-Topolewski, C. N., & Graves, J. M. (2020). “I worry about his future!” Challenges to future planning for adult children with ASD. Journal of Family Social Work, 23(1), 71–85. https://doi.org/10.1080/10522158.2019.1578714
McIntosh, C. E., Thomas, C. M., Wilczynski, S., & McIntosh, D. E. (2018). Increasing nursing students' knowledge of autism spectrum disorder by using a standardized patient. Nursing Education Perspectives, 39(1), 32–34. https://doi.org/10.1097/01.NEP.0000000000000179
Miller, S. M. (2015). Nurses caring for adults with autism in an emergency department: A survey of knowledge. Doctoral Projects, 7. https://doi.org/10.31979/etd.tenz-w3vk
Miot, S., Akbaraly, T., Michelon, C., Couderc, S., Crepiat, S., Loubersac, J., Picot, M. C., Pernon, É., Gonnier, V., Jeandel, C., Blain, H., & Baghdadli, A. (2019). Comorbidity burden in adults with autism spectrum disorders and intellectual disabilities - A report from the EFAAR (Frailty Assessment in Ageing Adults with Autism Spectrum and Intellectual Disabilities) Study. Frontiers in Psychiatry, 10, 617. https://doi.org/10.3389/fpsyt.2019.00617
Mitchell, M. J., Newall, F. H., Sokol, J., & Williams, K. J. (2020). Simulation-based education for staff managing aggression and externalizing behaviors in children with autism spectrum disorder in the hospital setting: Pilot and feasibility study protocol for a cluster randomized controlled trial. JMIR Research Protocols, 9(6), e18105. https://doi.org/10.2196/18105
Neumeyer, A. M., O'Rourke, J. A., Massa, A., Lee, H., Lawson, E. A., McDougle, C. J., & Misra, M. (2015). Brief report: Bone fractures in children and adults with autism spectrum disorders. Journal of Autism and Developmental Disorders, 45(3), 881-887. https://doi.org/10.1007%2Fs10803-014-2228-1
Nicolaidis, C., Kripke, C. C., & Raymaker, D. (2014). Primary care for adults on the autism spectrum. The Medical Clinics of North America, 98 (5), 1169–1191. https://doi.org/10.1016/j.mcna.2014.06.011
Nicolaidis, C., Raymaker, D., McDonald, K., Kapp, S., Weiner, M., Ashkenazy, E., Gerrity, M., Kripke, C., Platt, L., & Baggs, A. (2016). The Development and evaluation of an online healthcare toolkit for autistic adults and their primary care providers. Journal of General Internal Medicine, 31(10), 1180–1189. https://doi.org/10.1007/s11606-016-3763-6
Quiban, C., Brooks, R., & Armstrong, D. (2020). Caring for adult patients with autism in the critical care setting. Critical Care Nursing Quarterly, 43(1), 58–67. https://doi.org/10.1097/cnq.0000000000000291
Raymaker, D. M., McDonald, K. E., Ashkenazy, E., Gerrity, M., Baggs, A. M., Kripke, C., Hourston, S., & Nicolaidis, C. (2017). Barriers to healthcare: Instrument development and comparison between autistic adults and adults with and without other disabilities. Autism: The International Journal of Research and Practice, 21(8), 972–984. https://doi.org/10.1177/1362361316661261
Roux, A. M., Rast, J. E., Garfield, T., Shattuck, P., & Shea, L. L. (2021). National autism indicators report: Family perspectives on services and supports. https://drexel.edu/~/media/Files/autismoutcomes/publications/NAIR%20Family%202021%20Final.ashx
Saqr, Y., Braun, E., Porter, K., Barnette, D., & Hanks, C. (2018). Addressing medical needs of adolescents and adults with autism spectrum disorders in a primary care setting. Autism: The International Journal of Research and Practice, 22(1), 51–61. https://doi.org/10.1177/1362361317709970
Smeltzer, S. C., Avery, C., & Haynor, P. (2012). Interactions of people with disabilities and nursing staff during hospitalization. The American Journal of Nursing, 112(4), 30–52. https://doi.org/10.1097/01.NAJ.0000413454.07369.e3
Thurm, A., Farmer, C., Salzman, E., Lord, C., & Bishop, S. (2019). State of the field: Differentiating intellectual disability from autism spectrum disorder. Frontiers in Psychiatry, 10, 526. https://doi.org/10.3389/fpsyt.2019.00526
Turcotte, P., Mathew, M., Shea, L. L., Brusilovskiy, E., & Nonnemacher, S. L. (2016). Service needs across the lifespan for individuals with autism. Journal of Autism and Developmental Disorders, 46(7), 2480–2489. https://doi.org/10.1007/s10803-016-2787-4
Turner, A. M., Osterhage, K., Loughran, J., Painter, I., Demiris, G., Hartzler, A. L., & Phelan, E. A. (2018). Emergency information management needs and practices of older adults: A descriptive study. International journal of medical informatics, 111, 149–158. https://doi.org/10.1016/j.ijmedinf.2017.12.001
Vohra, R., Madhavan, S., & Sambamoorthi, U. (2016). Emergency department use among adults with autism spectrum disorders (ASD). Journal of Autism and Developmental Disorders, 46(4), 1441–1454. https://doi.org/10.1007/s10803-015-2692-2
Weir, E., Allison, C., & Baron-Cohen, S. (2022). Autistic adults have poorer quality healthcare and worse health based on self-report data. Molecular Autism,13(23). https://doi.org/10.1186/s13229-022-00501-w
Wise, E. A., Smith, M. D., & Rabins, P. V. (2020). Correlates of daily functioning in older adults with autism spectrum disorder. Aging & mental health, 24(10), 1754–1762. https://doi.org/10.1080/13607863.2019.1647138
Wright, S. D., Guan Wright, C. A., D’Astous, V., & Wadsworth, A. M. (2019). Autism aging. Gerontology & Geriatrics Education, 40(3), 322–338. https://doi.org/10.1080/02701960.2016.1247073
Zandam, H., Mitra, M., Akobirshoev, I., Li, F. S., & Ne'eman, A. (2022). Infectious diseases-related emergency department visits among non-elderly adults with intellectual and developmental disabilities in the United States: Results from the national emergency department sample, 2016. Population Health Management, 25(3), 335-342. https://doi.org/10.1089/pop.2021.0218


