A tertiary, non-profit academic medical center in California encountered the demands of a rapidly evolving set of COVID-19-related guidelines in 2020. Several outdated structures and processes were identified as operational inefficiencies compounded by siloed manual work, lack of role clarity, and increased operation costs. Thus, the department of nursing education began identifying opportunities for digital transformation to improve operational efficiency, streamline the scope of work, improve team collaboration, and reduce operating costs. Using Kotter’s eight-step process for leading change, implementing digital transformation decreased excessive costs. This was achieved by reducing nursing professional development practitioners’ time spent on task-related work by 63%, allowing them to practice at the highest level of their scope and training. Additionally, leadership support, innovation, conformity to experiment, visibility and accessibility of work, interdepartmental collaboration, and communication transparency were key factors for the success of digital transformation.
Key Words: COVID-19, change theory, digitization, digitalization, digital transformation, healthcare, industry, management, nursing, professional development, revolution, technology, innovation, education, Kotter’s
The COVID-19 pandemic necessitated innumerable and unprecedented changes, particularly within health care. Amidst the constant need to address organizational and customer needs, the healthcare system is rapidly adopting digitization and digitalization to simplify and enhance work-related processes. Digitization involves technical processes, such as converting paper-based records into a digital format, and digitalization entails the inclusion of technology to facilitate or produce services such as online virtual professional development (Iyamu et al., 2021). Digital transformation is a continuous, complex, and disruptive process (Iyamu et al., 2021). It encompasses both digitization and digitalization and has been considered necessary by every industry to maintain uninterrupted functioning during COVID-19. This article’s “digital transformation” reference encompasses both digitization and digitalization.
the healthcare system is rapidly adopting digitization and digitalization to simplify and enhance work-related processes.
Educational systems have adopted online working methods and have incorporated appropriate models that facilitate them. Corporate giants have provided their employees with the tools, training, equipment, and resources that enable them to work remotely to keep themselves afloat in the market and ensure adherence to the COVID-19 safety protocols. The scope and need for digital transformation have grown exponentially and rapidly in the last two years. Ironically, the pandemic has encouraged innovation and improved provision of services, even in health care, in ways that were perhaps not even considered possible so far (McGrow, 2021).
COVID-19 has significantly altered people’s lives and has caused unprecedented disturbances in the global economy and health care with untold impacts. To avoid a complete functional breakdown, governments were forced to reopen societies, including small- and large-scale businesses and corporate and educational sectors. This called for urgent digital transformation across several industries (Whitelaw et al., 2020). It was vital for healthcare industries to proactively reduce the spread of the virus while maintaining COVID-19 safety protocols. Therefore, frontline healthcare workers and researchers pushed their boundaries to engage in innovative transformation, research, and developmental activities.
The scope and need for digital transformation have grown exponentially and rapidly in the last two years.
By the beginning of 2021, most healthcare fields focused on the viability of digital transformation. On the one hand, healthcare organizations have adopted such transformation in their clinical realm through virtual appointments via platforms like Zoom, Microsoft Teams (MT), or other video call portals. Non-clinical departments, such as the department of nursing education, encountered challenges in meeting the needs of their employees and hospital staff, such as improving work processes, clarifying roles, accommodating learner-preferred styles, attending in-person meetings, or managing course registrations and evaluations. With a surge in data, electronic systems found their place in various industries, including health care. Information technology companies like Google and Microsoft have helped immensely by developing digital tools for effective virtual meetings. These technologies have been available for years but have yet to be utilized in many medical centers.
Although digital transformation seemed like the most evident solution, the intensity and manner it was incorporated across various fields was sudden. Digital tools and training are necessary to keep the market running. The increasing global dependency on the healthcare system and the ongoing pandemic have made it almost mandatory for health informaticists and in-house departments to use such tools that make their jobs efficient (Nachit & Belhcen, 2020). Chou (2019) referred to this global transformation as the fourth industrial revolution (Industry 4.0). Its primary intention is to create a world that relies on “smart” technologies wherein the changes would be digital instead of physical (Chou 2019, p.107).
Background and Significance
A large, tertiary, non-profit academic medical center in Los Angeles, California, encountered challenges in keeping up with the rapid changes owing to COVID-19. The nursing education department, comprising nursing professional development practitioners (NPDPs) and department staff, needed help to keep up with a constantly evolving set of COVID-19 guidelines. In meeting these challenges, several outdated structures and processes were identified, thus highlighting the scope for improvement. These included traditional delivery of in-person training and education, manual record keeping of regulatory training, heavy reliance on e-mail as the only mode of communication, and manual data collection management to monitor outcomes. Such operational inefficiencies were compounded by siloed manual work, lack of role clarity, and increased operation costs.
The NPDPs play various key roles within their scope of practice. According to the Association for Nursing Professional Development (ANPD) (2022), NPDPs assist in continual learning and role competence. They engage in activities that promote the professional development of staff, which leads to optimal patient care, population health, and public protection. For example, learning facilitators consult with departments in the educational design process to bridge knowledge, skills, and practice-related gaps identified through needs assessment. As agents of change, they proactively collaborate with interdisciplinary teams using project management and improvement processes. They also advance the nursing profession and influence interprofessional practices and learning environments, the NPD specialty, and health care through leadership and mentorship roles (ANPD, 2022).
The department of nursing education is responsible for several programs, most of which compete with other organizational priorities. In general, departmental work needed to be prioritized, and the exact roles and responsibilities assigned to NPDPs, and other team members needed to be clarified. These issues became more pronounced during the pandemic due to a lack of communication, follow-through, and proper structures and processes. The NPDPs reported spending over a third of their time on manual administrative tasks, preventing them from practicing at the top of their scope, which entails leading, facilitating, mentoring, coaching, and managing projects. Minimal interface and collaboration resulted in redundancy, duplicate work efforts, and operational inefficiencies. Moreover, faced with uncertainties of the pandemic’s onset in March 2020, traditional classroom training became nearly impossible. All classroom and conference room reservations were canceled. Any requests to hold in-person training, education, or meeting events required justification and leadership approval by the senior vice president, chief nursing officer, and chief of medical staff. Thus, the team had to create online training programs rapidly.
As the responsibilities and logistics to conduct traditional classroom training were significantly limited, time-consuming, manual, and required more staff support, the NPDPs reported working approximately 13.71 hours (34.27%) per week on administrative processes. This work included record keeping and data collection, preparation of handouts, binders and instruction manuals, course evaluations, and data analysis to track quality outcomes. For example, two or three individuals in the department of nursing education were responsible for manually storing essential training data and records. These were accessible to only a few individuals who had to undergo a formal process to access the data. This often resulted in delays and limited access for other team members who relied on data to improve programs or address customer needs. Khanmohamed (2020) found that paper-based and manual processes cost up to 20 times more than electronic or digitized processes. Due to a lack of time and knowledge, staff may not search for best practices within the literature but continue to repeat the same inefficiencies resulting in approximately a 60% reduction in work effectiveness (Khanmohamed, 2020).
Problem Statement
The identified problems highlighted the need for digital transformation within the center's nursing education department to reduce operating costs, improve operational efficiency, streamline the NPDP scope of work, and improve team collaboration. The pandemic intensified & accelerated this project, which aimed at improving operational efficiency through digital transformation. The intention was to increase the NPDPs’ self-reported time to practice within their scope and decrease administrative or task-related manual work hours by 50%.
Methodology and Implementation Plan
The team of NPDPs, led by the Director of Nursing Education, was supported by the Executive Director, Chief Nursing Officer/Vice President (VP), and Systems Chief Nurse Executive/Senior VP, with a vision for innovation and digital transformation. Using Kotter’s eight steps for leading change, the team embarked on the digital transformation from March 2020 to April 2022. Kotter’s change theory is defined as 1) a sense of urgency, 2) a team to lead and facilitate the transformation, 3) a vision and initiatives, 4) engagement of key stakeholders; 5) action to remove barriers, 6) short-term wins 7) sustained acceleration and 8) instituting changes (Kotter, 2012). This quality improvement project was deemed “Not Regulated” as it does not involve human subjects research and therefore did not require institutional review board approval per the institution’s office of research compliance and quality improvement policy.
Step 1: Establishing Urgency
The COVID-19 crisis was enough to propel the need for digital transformation. The department of nursing education needed to find innovative ways to streamline departmental processes while continuing to meet the organization’s education and training needs. The NPDPs were responsible for rapidly onboarding and orienting new hires and temporary staff, as the pandemic resulted in a fewer number of staff and increased burnout. The staff needed urgent training to adapt to COVID-19-related guidelines and use personal protective equipment in addition to other regulatory requirements, such as basic and advanced life support, keeping staff and patients safe. Lastly, monitoring departmental and organizational outcomes was needed to ensure structures and processes were in place.
Step 2: Creating a Team to Lead and Facilitate
The NPDPs’ then-current workload was reviewed and redistributed to initiate a rapid organizational transformation. A few programs were put on hold to prioritize support for the rapid onboarding and orientation, redeployment training, and constant education awareness amid rapidly changing COVID-19 guidelines. New leadership roles were identified and hired. An NPDP was assigned to lead the onboarding and orientation of newly hired employees and staff for redeployment. Another NPDP was reassigned to lead the COVID-19 education task force. Relevant talents and skills among team members were assessed and evaluated. Consequently, the NPDPs with expertise in data collection and digital technology were identified and encouraged to present the idea of digital transformation in a more easy-to-absorb manner. Leadership supported additional job roles, such as hiring the Director of Nursing Education, Project Manager, and Project Coordinators to support the work on digital transformation. Team members were encouraged to participate in interdepartmental activities to promote team building. In a survey conducted by McKinsey (2018) on digital transformation, new leaders familiar with digital technologies emerged as key to successful digital transformation. Additionally, it was revealed that it is vital to build the digital capabilities of the team for the success of such transformation by redefining the roles and responsibilities of key team members, identifying digitally savvy team members who will bridge the gap between traditional and digital transformation, and developing talents and skills to align with such transformation (McKinsey, 2018)
an achievable vision was planned and developed to set up methods to lead to digital transformation.
Step 3: Developing Vision and Strategy
With the emergence of rapid digital transformation, an achievable vision was planned and developed to set up methods to lead to digital transformation. Leaders had to find innovative ways to propel the team toward digital transformation. This called for calculated risk-taking, increased collaboration, and a focus on staff and patient-centered compassionate care. Critical factors in attaining strategic initiatives were identified after establishing a sense of urgency and empowering teams with an inspired vision. The department established key initiatives and determined the best methods of instruction, which included face-to-face (traditional), online with web-based resources (remote), and a combination of both (hybrid) to address the pandemic-related priorities.
- Successful onboarding, orientation, and training of newly hired experienced nurses and new graduate nurse residents (hybrid)
- Successful redeployment training of staff to priority areas where staffing was needed (hybrid)
- Implementation of digital tools to make information more accessible across the organization (hybrid)
- Implementation of digital self-serve technology for internal and external partners (remote)
- Formation of pertinent advisory committees to ensure support, engagement, and collaboration with key stakeholders (remote)
Amidst the pandemic, the department supported the organization’s key initiative to support the sixth magnet redesignation.
- Successful submission of the Practice Transition Accreditation Program (PTAP) for the New Graduate Nurse Residency Program with Distinction
- Revision of the professional practice model to integrate the Theory of Caring Science
- Restructuring of shared governance to shared leadership councils
- Implementation of the online mentoring program
- Adopted the NPD Practice Model (ANPD, 2022)
Table 1. Digital Technology used and its functions for the Department of Nursing Education Programs and Operational Workflow
|
Programs and Workflow |
Box Cloud |
MS Teams |
Online Surveys |
New Software |
Smartsheet |
|---|---|---|---|---|---|
|
Department of Nursing Education Programs and Workflow |
|
|
|
|
|
|
New Functions or Digital Technology Identified |
|
|
|
|
|
Table 1 illustrates the digital technologies incorporated into nursing education programs and operational workflow. The pre-existing resources within the organization were the Box cloud, MS teams, and online surveys like Research Electronic Data Capture (Redcap ®). The team transitioned from using shared drive and frequent e-mail exchanges to using Box ® cloud and Microsoft Teams technology for file sharing, data storage, team communication, and collaboration. With leadership support, the department invested in new software, such as the online student clinical placement system, online mentoring platform, and Smartsheets ® to support programs.
Step 4: Engaging Key Stakeholders – Communication and Collaboration
Buy-in and support of key stakeholders for new innovative digital transformation ideas compelled the NPDPs to identify gaps in visibility, accessibility, communication, and collaboration. Virtual weekly huddle meetings ensured that every team member worked collectively toward a common goal and understood their roles. Huddle meetings also reinforced departmental priorities and projects and addressed any barriers or concerns surrounding digital transformation. The visibility of nursing education and professional development programs increased in weekly leadership meetings. With the introduction of digital technology to support programs, the NPDPs began to develop and lead vital advisory committees to engage key stakeholders from interprofessional teams such as human resources (HR) training and organizational development, HR talent acquisition, unit-based NPDPs, Clinical Nurse Specialists (CNS), associate directors (ADs), assistant nurse managers (ANMs), and clinical support teams. Several advisory committees were formed to support engagement and collaboration among key stakeholders, such as the Transition to Practice Advisory Committee, Preceptor Advisory Committee, Professional Development Committee, Competency management workgroups, and new graduate nurse residency program workgroup. The NPDPs who led committees and programs engaged various stakeholders through visibility and facilitated communication through virtual platforms like Microsoft Teams, SharePoint, Box, and Zoom.
Step 5: Empowering to Experiment with New Digital Ideas
The NPDPs reviewed old practices and explored ways to improve their workflow. Leadership empowered them to experiment with new innovative ideas and explore existing resources and tools to improve communication and collaboration, monitor and track training, and data collection and analysis of outcomes. Table 2 describes the transition in innovative ideas experimentation. The teams were encouraged and supported but not mandated to transition to these new digital technologies. To improve file sharing, communication, and collaboration, the transition from a shared drive to Box ® file sharing was one of the first digital technologies explored early on during the shift toward accreditation from the PTAP. Using a project tracker was also encouraged for weekly one-to-one meetings with direct reports. MS Team channels were also utilized early for communication, collaboration, and project management. These virtual platforms and software programs were choices for early tool integration into digital technology because they were readily available through the organization, and the NPDPs were familiar with them as the main modes of virtual meetings after the onset of COVID-19. The transition from paper-based data collection was facilitated and supported with the availability of the RedCap ® software for all employees, a secure web application for building and managing online surveys and databases. Smartsheet ® was also introduced, allowing teams to move faster, drive innovation, improve accountability, increase connectivity, and keep remote teams focused. Leaders ensured each newly implemented standard operating procedure was accessible to the team, and each team member was provided the support and resources to operate the platforms. The NPDPs and other staff members were prioritized to learn and understand the working methods of various electronic and digital platforms.
Table 2. Transition of Key Strategic Initiatives to Digital Solutions
|
Key Strategic Initiative |
Traditional Method |
Digital Solution |
|---|---|---|
|
Weekly reporting |
|
|
|
Monitoring and tracking |
|
|
|
Communication and collaboration |
|
|
|
Data collection and analysis |
|
|
Step 6: Generating Short-term Wins
As the team started to integrate digital platforms into their daily work, the focus of weekly huddles shifted to include the four Rs of success – recognition, reflection, readiness, and reminders. This process was vital to the success of the overall digital transformation process to encourage staff during a time of change, share best practices, and ensure timelines were being met. The leaders modified the weekly huddle reporting structure to be team-led. Each team member rotated to lead the weekly meeting and was encouraged to share their appreciation (recognition) of what they have accomplished, and gratitude of self and for the support from others. They were encouraged to share their current priorities (reflections) and future work (readiness), including any requests for support from the leaders and the team. Lastly, each team member provided information on upcoming events and where electronic information, such as surveys or team files, could be found or accessed (reminders). The team was supported and encouraged to gradually use digital technology in their daily work. For example, Box file sharing was initially introduced to the PTAP writing team to transfer files from shared drive to Box for team collaboration. Smartsheet ® experimentation gradually started with one subscription, allowing team members to create drafts and explore its functionality. MS Team channels were initiated for the department and then gradually explored to address programmatic needs. Each step of the way was celebrated, encouraged, and supported.
Step 7: Sustaining Success and Acceleration
With the introduction of several digital technologies to the daily workflow and celebration of short-term win successes, the team was inspired and encouraged to sustain successes through communication, collaboration, constant clarification, and celebration. A two–way feedback system using the MT channel was created to improve communication among team members and inter-professional groups and to maintain progress toward digital transformation. Team members were encouraged to communicate concerns, feedback, or recommendations regarding digitalization and daily work. Several drop-in sessions were conducted to allow more training and acclimatization to the new digital technologies and to provide ongoing support for those challenged with technology or resistant to change. Progress reports were communicated regularly for transparency and visibility of the work and to encourage engagement and support from key stakeholders.
Step 8: Anchoring New Approaches in the Culture
As this change process progressed in the department, new approaches and innovations were introduced. It was essential to ensure that each team member remained committed and supported throughout the digital transformation process, as it demonstrated significant economic and professional benefits and outcomes. The team participated in staff satisfaction pulse surveys as projects were piloted and successes were measured. Implementing digital transformation elevated organizational standards, improved operational efficiency, and provided team members with the technology skills to streamline their work, regardless of their roles.
Results of Digital Transformation and Essential Keys to Success
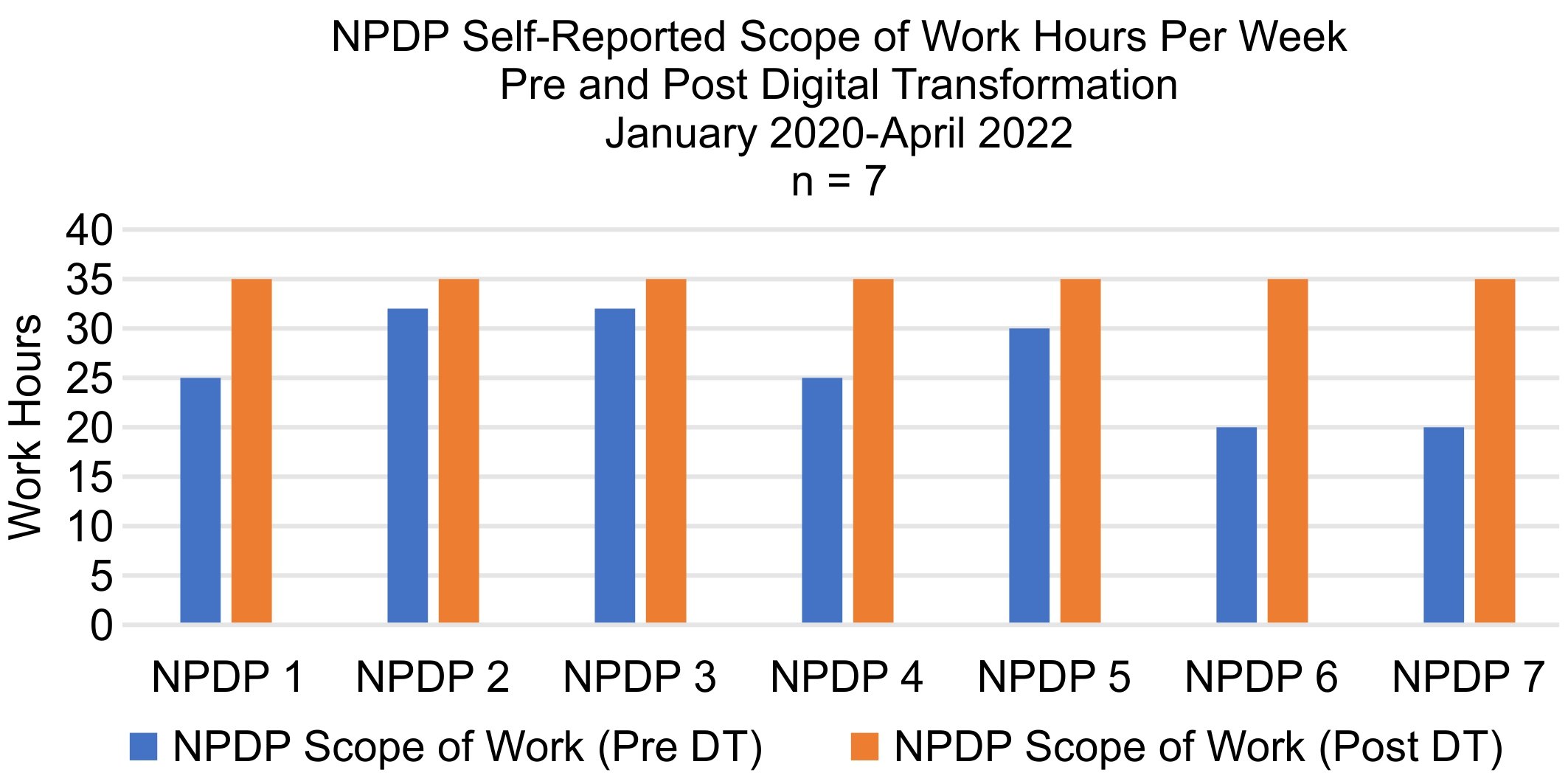
Transforming operations digitally can reduce workload and increase NPDPs' practice time. Seven out of 12 NPDPs who worked full-time equivalent in the department of nursing education were included in the analysis of reported work hours between January 2020 – April 2022. Five were excluded from the data analysis because they worked part-time or left the organization before April 2022. Figure 1 shows that all seven NPDPs included in this analysis reported reduced non-nursing administrative work hours. Consequently, figure 2 illustrates all seven NPDPs reporting increased work hours pertaining to their scope of practice.
Figure 1.
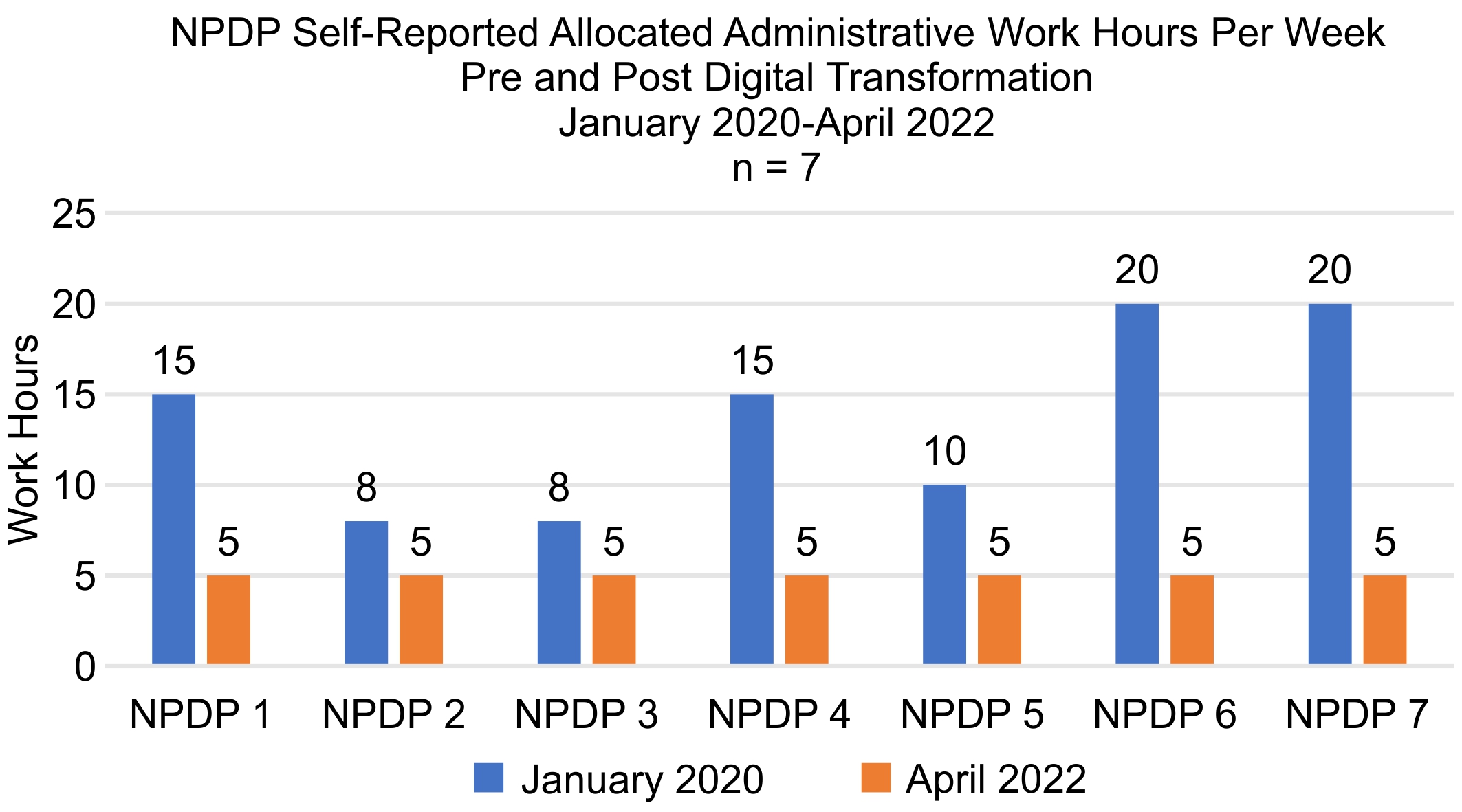
Figure 2.
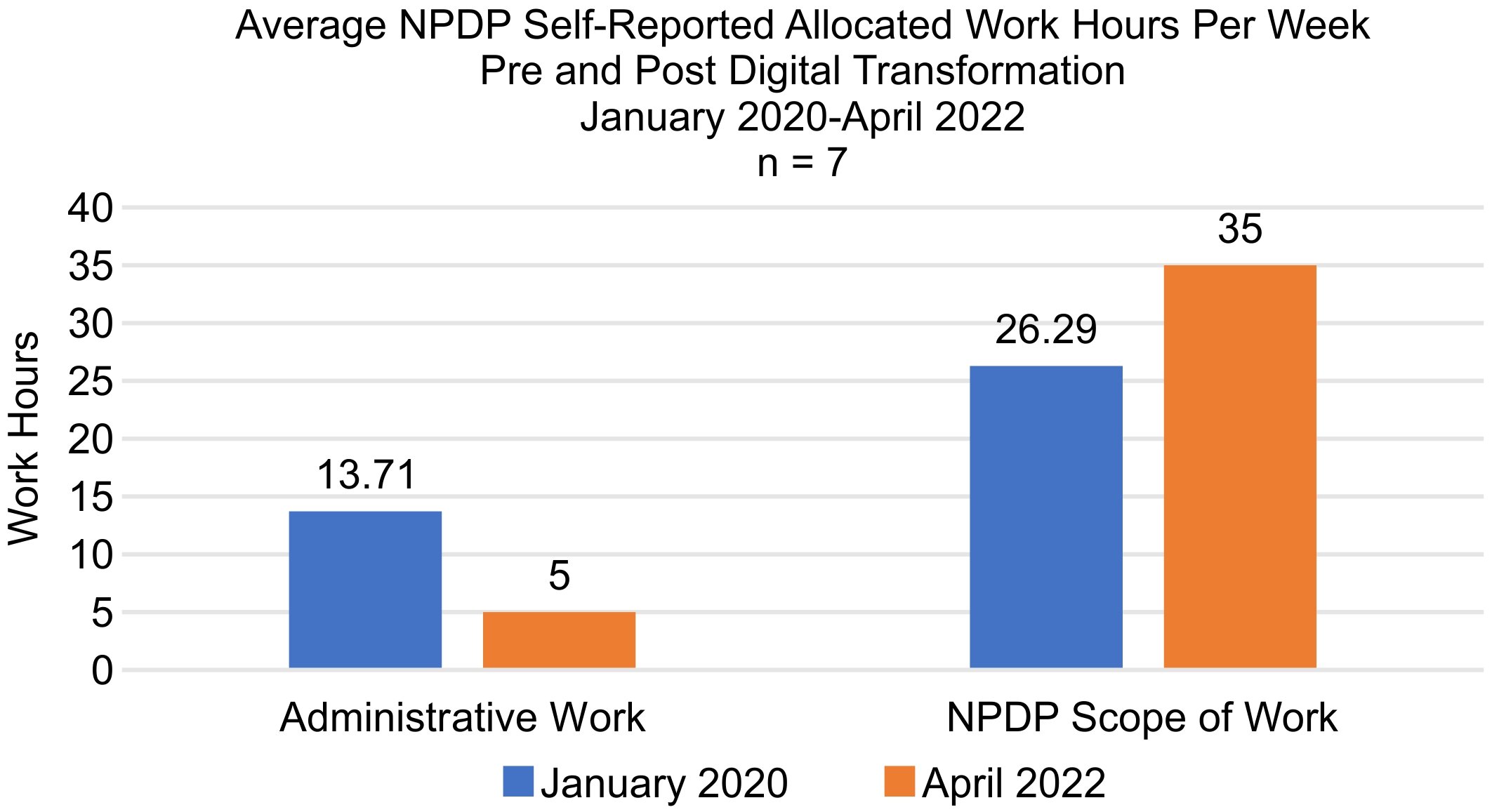
On average, figure 3 shows that NPDPs self-reported allocation of 13.71 hours per week (34.27%) to non-nursing administrative tasks before March 2020. With digital transformation, they could significantly reduce this to five hours per week (12.5%) for non-nursing-related administrative work. This implied a 63% reduction in allocated hours for administrative work, which is 13% higher than the projected outcome of 50%. Thus, the NPDPs reported increased work hours allocated to their scope of practice from 26.29 to 35 hours per week (Figure 3). Digital transformation enabled them to shift from manual processes to virtual solutions. This created more time to lead, facilitate, and collaborate with interprofessional teams, such as forming NPDP-led advisory committees, and helped redesign professional development programs successfully. Table 3 illustrates two NPD spheres of influence on collaborative partnership and scholarly work. With the transition to digital transformation and increased work hours to practice within their scope, the NPDPs could prioritize scholarly work by submitting 12 abstracts between March 2020 – April 2022, compared to an average of 2 – 3 abstracts before the digital transformation period. NPDP-led advisory committees exponentially increased from one to five, enhancing collaborative partnerships and engagement with key organizational stakeholders.
Figure 3.
Digital transformation is a key step taken in the nursing education department and organization for smooth and effective functioning. According to McKinsey & Company (2018), transformation is hard, and digital transformation is more challenging. Only 30% of organizations succeed in digital transformation,16% successfully improve and sustain performance, and the success rate, even in digitally savvy industries (high tech, media, telecom), is 4 - 11% (McKinsey, 2018). A few essential factors that made using digital tools a sustained success became evident. Various professional development programs were enhanced during the pandemic using the latest digital tools, such as BOX, Zoom, and MS Teams, to comply with COVID-19-related guidelines. The digital transformation eventually normalized the use of electronic and online platforms versus the traditional paper-based system. The progress of using smart sheets and MS Teams channels over time was a success due to the leadership’s encouragement for experimentation of innovative ideas and support for training and availability of resources to equip the team. Advantages of adopting digitalization include improved transparency, team management, increased interdepartmental collaboration and socialization, and great learning opportunities. Using Kotter’s eight-step process for leading change model, the department of nursing education of this non-profit, Californian, academic teaching medical center successfully orchestrated and carefully considered processes essential for leading the digital transformation.
Table 3. Evidence of Increase NPDP Practice within Their Scope
|
NPDP Throughputs |
Prior to March 2020 |
March 2020 – April 2022 |
|---|---|---|
|
Scholarly work |
|
|
|
Collaborative partnerships |
|
|
Lessons Learned and Future Considerations
The COVID-19 pandemic restricted the usual routines across most industries, and their management needed to prepare for the consequent changes. One limitation was the lack of time to conduct proper assessments or analyses of daily workflow and employee skills before implementing digital tools within the department. Team members had to step in to identify the best approaches to stay on track. With any virtual platform or software application, time should be allotted to review the purpose of the digital technology and its functionalities to determine if it meets the needs of a given department. Therefore, an implementation and training plan should be included to assist team members in learning the relevant technology. Opportunities to practice in the playground should also be available when providing support. Although this article focused on the department of nursing education being well equipped with the latest gadgets and technologies, some NPDPs demonstrated resistance or lack of interest in learning new skills or embracing digital transformation. Their reasons included lack of time due to competing priorities, various technologies to choose from, comfort with traditional approaches and current daily routine, and difficulty understanding operational processes. However, more than half of the team members showed great enthusiasm and determination in adopting new platforms and developing new skills.
Plans include the creation of a committee responsible for innovation and digitalization to employ digital toolkits and user guides so that the NPDPs and other team members can utilize digital platforms and social media in their daily work lives. A special advisory council will be developed to analyze the daily workflow in the department and provide recommendations for future digital tools and training support to support the journey toward digital transformation.
Conclusion
Like most healthcare organizations, at the beginning of the pandemic, the department of nursing education needed to prepare for the necessary situational changes. The department focused on finding the latest innovative digital tools that comply with COVID-19-related guidelines and hospital policies. Kotter’s eight-step model for leading change facilitated the rapid digital transformation was the project framework. Leadership support, vision, and encouragement to experiment with innovative ideas were vital in empowering the team to continue testing what worked well for the team and the organization. It was essential to bring in leaders with the vision for transformation and the ability to unleash the potential of team members. This was key to ensuring a shift in mindset, culture, and agility to promote and sustain a workforce that was future-ready. Digital transformation, education, and professional development programs became visible and accessible to the organization, enabling interprofessional and interdepartmental collaboration and transparency in communication. More importantly, it paved the way for the NPDPs to practice within their scope by leading the change, managing projects, facilitating, mentoring, coaching, and teaching the future healthcare workforce.
Authors
Anupa Roshan, MSN, RN, CCRN-K, NPD-BC*
Email: Anupa.Roshan@cshs.org
Anupa Roshan, MSN, CCRN-K, NPD-BC is an experienced nurse professional development practitioner (NPDP), with 22 years of experience in nursing. She is the Training Center Coordinator for the American Heart Association (AHA) and American Red Cross (ARC) Resuscitation Programs and Nurses Improving Care for Healthsystem Elders (NICHE) in the Geri and Richard Brawerman Nursing Institute at Cedars Sinai Medical Center. The Resuscitation Digitalization and NICHE/ American Board of Internal Medicine (ABIM) Choosing Wisely ® Trailblazer Award were achieved under her leadership. She led the transformation of data collection from a manual process to an online digital platform with her expertise in setting up and training teams using Redcap ® as an online survey tool for different programs.
Janette V Moreno, DNP, RN, NEA-BC, NPD, BC
Email: Janette.Moreno@cshs.org
Janette V Moreno, DNP, RN, NEA-BC, NPD-BC is an experienced nursing leader and the Director of Nursing Education at the Brawerman Nursing Institute, with more than 20 years of nursing and leadership experience. She is a forward-thinking and passionate professional respected for guiding hospital-wide nursing services by designing key programs and aligning organizational vision. She is an out-of-the-box thinker and has led the digital transformation and believes in utilizing expertise with current theories, technologies, techniques, and approaches to achieve nursing excellence.
Millicent G De Jesus, PhD, RN-BC, NPD-BC
Email: Millicent.Dejesus@cshs.org
Millicent G De Jesus, PhD, RN-BC, NPD-BC, has over 25 years of nursing experience. She is currently an NPDP at Cedars-Sinai Medical Center (CSMC). As a subject matter expert, she actively participated and led various organizational initiatives involving technology such as, barcoding medication administration, device integration, nursing workflows in the build of CSMC’s electronic medical record, and simulation-based clinical education. She is currently the lead of competency management and provides consultation on house-wide competency-based education rollouts using various electronic resources and tools. Presently, she is leading the transformation of competency assessment forms following the Donna Wright Competency Model, from paper to digital format.
Rebecca Ely, MSN, RN, CCRN-K, NPD-BC
Email: Rebecca.Ely@cshs.org
Rebecca Ely, MSN, RN, CCRN-K, NPD-BC currently works in the Brawerman Nursing Institute as an NPDP at Cedars-Sinai Medical Center. She leads the Shared Leadership Councils and has led the implementation of the virtual mentor program. Rebecca was part of the team that worked on transforming the department into a digital format. She transitioned the Academic Placement program from a manual process to a completely electronic process.
Charisse Murakami, MSN, RN, NPD-BC
Email: Charisse.Murakami@cshs.org
Charisse Murakami, MSN, RN, NPD-BC is an experienced NPDP, with 13 years of experience in nursing. She is one of the program site coordinators for the New Graduate RN Residency Program (NGRP) and the Chair of the Professional Development Committee (PDC). She supported the NGRP and PDC digital transformation from manual processes to the use of box file sharing, MS teams channel for team collaboration, redcap and surveymonkey for digital data collection and analysis. She also supported converting traditional classes to virtual learning environments.
Robert D Viana, MSN, RN, NPD-BC
Email: Robert.Viana@cshs.org
Robert DeLemos Viana, MSN, RN, NPD-BC is an experienced NPDP at Cedars-Sinai Medical Center. He is one of the program site coordinators for the New Graduate RN Residency Program (NGRP) who led the digital transformation of the program from manual process to use of box file sharing, MS teams channel for team collaboration, redcap and surveymonkey for digital data collection and analysis, and converted classes to virtual learning environments.
Jerome Finuliar, MSOD, PMP
Email: Jerome.Finuliar@cshs.org
Jerome Finuliar, MSOD, PMP is a project management professional, with over 10 years in health care, collaborating with leadership teams to identify improvement opportunities and develop a clear strategy for implementation. He’s led various digitization initiatives within the Brawerman Nursing Institute at Cedars-Sinai Medical Center and provided support for the use of digital tools to increase department effectiveness.
Margo B Minissian, PhD, ACNP, FAHA
Email: Margo.Minissian@cshs.org
Margo B. Minissian, PhD, ACNP, NEA-BC, FAHA, FNLA is the Executive Director, Geri & Richard Brawerman Nursing Institute and the Simms/ Mann Family Foundation Endowed Chair of Nurse Education, Innovation and Research. As the Executive Director of the Brawerman Nursing Institute (BNI), Dr. Minissian oversees the Departments of Nursing Education and the Department of Nursing Research with 40 staff members. The BNI provides professional development to over 800 nursing students across the medical center, including 21 doctorate students.
References
Association for Nursing Professional Development. (2022). Nursing professional development: Scope & standards of practice (Fourth edition). Chicago, IL: Association for Nursing Professional Development.
Chou, S.Y. (2019). The fourth industrial revolution. Journal of International Affairs, 72(1), 107-120. Retrieved from: https://www.jstor.org/stable/10.2307/26588346
Iyamu, I., Xu, A.X.T., Gómez-Ramírez, O., Ablona, A., Chang, H., McKee, G., & Gilbert, M. (2021). Defining digital public health and the role of digitization, digitalization, and digital transformation: Scoping review. JMIR Public Health and Surveillance, 7(11), pp. 1-14. e30399. https://doi.org/10.2196/30399
Khanmohamed, A. (2020, August 22). How much manual process in your business costs? AimInsight. Retrieved from: https://www.aiminsight.com/blog/how-much-manual-process-in-your-business-costs/
Kotter (n.d.) The 8-step process for leading change. Retrieved June 15, 2022, from https://www.kotterinc.com/8-step-process-for-leading-change/
McGrow, K. (2021). Overview and summary: Advancing technology in healthcare: Are you on board? OJIN: The Online Journal of Issues in Nursing, 26(3). https://doi.org/10.3912/ojin.vol26no03manos
McKinsey & Company (2018). Unlocking success in digital transformation. Retrieved from https://www.mckinsey.com/business-functions/people-and-organizational-performance/our-insights/unlocking-success-in-digital-transformations
Nachit, H., & Belhcen, L. (2020). Digital transformation in times of COVID-19 pandemic: The case of Morocco. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.3645084
Whitelaw, S., Mamas, M. A., Topol, E., & Van Spall, H. G. (2020). Applications of digital technology in COVID-19 pandemic planning and response. The Lancet Digital Health, 2(8), pp. e435-e440. https://doi.org/10.1016/s2589-7500(20)30142-4


