The evidence demonstrates that older adults who sustain hip fractures have greater functional decline, institutionalization, and death. Given the burden of falls and hip fractures, all efforts should be made to protect older adults from this injury. This article describes the biomechanics of fall and hip protector clothing, including first generation hip protector clothing, and the innovative, smart technology Tango Belt, a wearable belt that sends real-time data to a smart app and utilizes airbag technology to mitigate fall related hip injuries. Although hip protector clothing is protective, implementation has been met with resistance by patients and clinicians. We review the evidence for acceptance and feasibility of Tango Belt in various settings and describe how artificial intelligence supports motion sensing decision-making in areas such as postural sway and gait patterns. Finally, we offer implications for practice and research, in the hope that awareness about artificial intelligence-based hip protector clothing will encourage nurses to add these effective products to their fall injury prevention toolkits.
Key Words: Aged; aged 80 and over; injury from falls; hip fracture; mobility and balance; multisensory integration; function; artificial intelligence; technology
The two leading solutions to reduce fall-related trauma are floor mats and hip protectorsFor over a decade, healthcare providers and medical device industries have made slow progress to integrate protective solutions at the point of care to reduce risk of fall-related trauma (van Schoor, Asma, Smit, Bouter, & Lips, 2003; Yang et al., 2020; Zubkoff et al., 2018). The two leading solutions to reduce fall-related trauma are floor mats and hip protectors (Quigley, 2016). Nurses have been, and continue to be, the primary clinicians leading both the acquisition and implementation of these solutions within mostly inpatient settings that include acute and long-term care (LTC) (Soncrant, Neily, Bulat, & Mills, 2020; Yang et al., 2020). Nurses integrate floor mats and hip protectors into patient safety programs, fall and injury prevention care planning, and patient education programs.
While limitations exist for both of these low-cost solutions (de Bot, Veldman, Witlox, van Rhijn, & Hiligsmann, 2020; Quigley, 2016), floor mats have achieved greater integration at the point of care. They are placed at bed or chair side by nursing staff, although this does not always occur (Bowers, Lloyd, Lee, Powell-Cope, & Baptiste, 2008; Soncrant et al., 2020). However, floor mats provide only limited protection when patients fall from bed or chair. Hip protectors, in contrast, are imbedded in clothing, worn by the patient and provide protection when patients fall, irrespective of the patient’s location.
There have been repeated requests for improvements in hip protectors to increase patient adherence and expand impact protection. There have been repeated requests for improvements in hip protectors to increase patient adherence and expand impact protection. This article discusses evidence about the Tango Belt, a new hip protector solution, that protects patients from fall-related hip fractures. Until the Tango Belt, first generation hip protectors were the only garments designed specifically to pad hips to reduce fracture risk (Bulat et al., 2008). The Tango Belt uses current airbag technology packaged as a belt, designed with predictive analytics to measure preestablished outcomes.
Smart airbag belts with position sensors, combined with smart app technology, provide data that measure and report just-in-time outcomes including patient adherence, balance, and gait, while preventing fall-related hip fracture. The airbag belt is offered to adults as a clothing accessory, providing a wearable safety solution against hip fractures. Nurses play an essential role in the introduction of this intervention to protect patients from fall-related hip fractures.
Biomechanical analysis and progressive published case studies provide evidence of effectiveness that hip fractures can be reduced with smart technology belts that directly link patients, nurses, and interdisciplinary team members to individualized fall prevention care management and protection from hip fracture. Our purpose is to inform nurses across roles and the continuum of care about the biomechanics of falls, burden of fall-related hip fractures, evidence of hip protector effectiveness, and issues associated with current hip protector adherence.
Burden of Falls and Hip Fractures
Most falls due to unsafe environments or known untreated risk factors...are preventable. All nurses know that falls are common, but among vulnerable and older patients, they are disabling and even deadly. Most falls due to unsafe environments or known untreated risk factors (e.g., orthostasis, lower extremity sensory neuropathy, medication side effects) are preventable. Nurses can change practice and make a difference by reducing falls, focusing on reversible fall risk factors. If a fall is prevented, harm is avoided; but not all falls can be prevented.
Statistics confirm why prevention of falls must be among the top patient safety priorities. Falls are a leading cause of injury in adults 65 and older and falls are the leading cause of unintentional injury death in adults 85 and older (Centers for Disease Control [CDC,] 2020). In 2010, researchers found that 45% of the inpatient hospital population in the United States was 65 years of age and older, among whom 19% were ages 75-84, and 9% were 85 years and older (Levant, Chari, & DeFrances, 2015). For nursing home residents who experienced hip fractures, between July 2005-2009, risk for loss of life after hip fracture was estimated at 36.2% within 6 months after hip fracture (Neuman et al., 2014). The risk is even higher when adjusted for those over the age of 90, with multiple co-morbidities and no surgical management (Neuman et al., 2014). For those partially dependent in locomotion at baseline, 53.5% died or developed new total dependence within 180 days. To protect these patients from falls and resulting injury, nursing care requires a population-based approach based on injury risk; the population in this case is those with osteopenia, osteoporosis or fracture history.
A core competency for all nurses who care for older adults is knowledge that fall risks increase with age; the reasons older adults tend to have higher rates of falls; and the risk or fall-related hip fracture (Gray-Micelli & Quigley, 2020). Adults 85 years of age and older are 10 times more likely to sustain a hip fracture than adults 65-69 years of age (Hung, Egol, Zuckerman, & Siu, 2012). Older adults who sustain hip fractures have greater functional decline, institutionalization, and death.
Older adults who sustain hip fractures have greater functional decline, institutionalization, and death.Nurses know that 95% of hip fractures are due to falls (Gray-Micelli & Quigley, 2020). Approximately 10 to 20% of patients with hip fractures have subsequent hip fracture, representing a 2.5-fold increase in risk (Hung et al., 2012). In 2013, the Agency for Healthcare Research and Quality’s (AHRQ) presented hip protectors in their national hospital fall prevention guidelines as the only intervention to protect from injury (Shekelle et al., 2013). These statistics provide compelling evidence that all fall prevention programs must prioritize protection from injury, especially hip fractures (Quigley, 2016).
The Department of Veterans Affairs (VA) launched a national approach to protecting older and frail adults from hip fractures in 2004 (Bulat et al., 2008). At this time hip protectors were made available to all veterans at risk for hip fracture. The VA is the only national healthcare system to implement a population-based approach to reduce serious fall-related injuries within acute and LTC settings. This population-based approach included those at risk for fracture, tested across 57 LTC facilities (Zubkoff et al., 2018). Yet, even when available as a result of this national policy, recent analysis of major injuries in the VA revealed that the highest percent of major injuries, 43% (66/128) were hip fractures. Further analysis revealed that hip protectors were not worn by these patients when they fell (Soncrant et al., 2020). In addition, while current hip protectors have been found to reduce hip fracture risk by slightly over twofold, fractures can still occur when hip protectors are worn, dependent on severity of fracture risk and sustained trauma (Yang et al., 2020).
Biomechanics of Fall and Hip Protector Clothing
The pelvis is not protected by the hip pads.For over 10 years, protecting patients from injurious falls has been the call-to-action (Boushon et al., 2012; Oliver, Healey, & Haines, 2010). While fall risks factors are complex, injuries such as hip fracture are directly linked to the direction of the body fall; velocity of impact; and severity of osteoporosis (Tarbert, 2020a; Yang et al., 2020; Unnanuntana, Gladnick, Donnelly, & Lane, 2010). The study of directional falls and impact velocity uses biomechanical analysis of simulated falls and video-recorded falls in LTC settings. Researchers studying the biomechanics of simulated falls have found that hip impacts occurred with trips during slow gait speed; stepping down during normal gait speed; and stepping up and slipping during fast gait speed (Smeesters, Hayes, & McMahon, 2007). Researchers who studied the biomechanics of video-recorded falls experienced by residents from two facilities found that hip protectors were protective against hip fractures that occurred from lateral falls (Yang et al., 2020). The hip protectors did not prevent pelvic fractures that occurred during a backwards fall. The pelvis is not protected by the hip pads.
First Generation Hip Protector Clothing
The vast majority of hip fractures result from a fall with direct impact on the greater trochanter of the proximal femur. Hip protector clothing was created as a protective garment to cover the greater trochanter to reduce impact forces on the hip. The clothing has been shown to attenuate the peak impact force on the hip by 37% to 95%, depending on type, model, and applied force impulse (Bulat et al., 2008). External hip protectors are girdle-like devices, with shells made of polyurethane (Kannus et al., 2000; Rubenstein, 2000). Multiple types of hip protectors are available on the market and can be divided into soft shell hip protectors that absorb the energy and re-distribute the force of fall; hard shell hip protectors that shunt the energy of the impact away from the head of the trochanter into the surrounding soft tissues; and hybrid models that combine the hard and soft shell (Holzer & Holzer, 2007). The devices are sewn into clothing such as male and female undergarments, pants, sweatpants, and shorts.
Hip protector clothing was created as a protective garment to cover the greater trochanter to reduce impact forces on the hip.Hip protector clothing, mostly a nurse-initiated solution, thus provides continuous direct protection to head of the trochanter during lateral impact. Within healthcare organizations, hip protectors are prescribed by nurses, physical therapists, or physicians. After measuring circumference of the hip, they are ordered by size and provided by the medical supply department.
Even though these devices are protective, implementation has been met with resistance. Providers in LTC had negative perceptions about hip protectors along with concerns of staffing shortages (Korall et al., 2018). In clinical settings, a hip protection unit peer champion is essential to achieve sustainability, reliability, and scalability (Korall et al., 2018). Patients found the clothing to be uncomfortable, bulky, and a source of stigma. Yet, little social marketing exists within the United States, possibly due to ageism bias, even though the grave consequences of hip fractures are widely known. These barriers to hip protector adoption and sustainability continue to impede progress to reduce the social and economic burden of hip fractures (Quigley, 2016; van Schoor et al., 2003; Yang et al., 2020). Thus, patients, especially older adults, would benefit from another option.
Even though these devices are protective, implementation has been met with resistance.To fill this urgent gap in patient safety, an innovative solution in the form of smart belt and smart application technology exists for nurses to incorporate into fall injury prevention at the point of care. In the next section, we discuss this intervention that offers adults a clothing accessory that provides a wearable safety solution as a fashionable touch and safety function.
Innovative Smart Belt Technology: The Tango Belt
The belt is specifically for the population who is most at risk of hip fracture.The Tango Belt is a smart wearable that was designed to overcome the adherence barrier of wearing hip pads. The belt is specifically for the population who is most at risk of hip fracture. A 3D sensor is located in the back portion of the device, offering valuable data via continual motion monitoring of balance and movement (see image 1). When buckled and worn on the human torso, the belt sensor is constantly capturing information about the motions that the individual is performing. When the belt recognizes that the person is entering into a fall motion that would likely result in a serious, hip-impacting fall it will deploy airbags surrounding both hips that significantly reduce the force of ground impact on the hip. Upon impact, the belt will then sound an alert to bring needed attention from staff to the individual who has suffered the fall.
Image 1
The Tango Belt, worn by older adult user

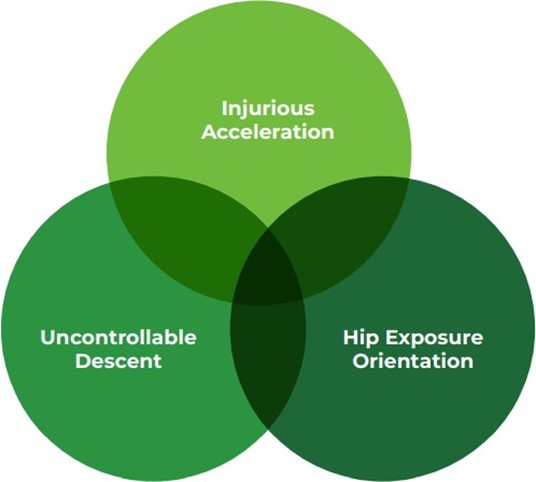
The design of the algorithm for accuracy in airbag deployment was developed based upon the previously discussed research about what aspects of human motion cause hip fractures. The artificial intelligence (AI) within the data gathered by the sensors feed into the algorithm, continually strengthening the specificity and sensitivity of the Tango Belt’s ability to distinguish falls that result in a hip fracture versus all falls. Currently, the Tango Belt has been worn for over 70,000 hours to collectively offer information to the system about when a trigger with airbag deployment should occur. The algorithm is based upon three major components to movement that leads to hip fractures: falling uncontrollably; falling in the direction of greatest hip impact potential; and falling at a dangerous rate of acceleration.
The artificial intelligence (AI) within the data gathered by the sensors feed into the algorithm...Falling uncontrollably refers to the inability to stop or slow oneself during the process of falling. The individual enters into a movement of “uncontrollable” descent toward the earth. Falling in the direction of greatest hip impact potential has been confirmed as lateral and posterior lateral in past and recent research, as noted previously. Positioning of the body during the fall motion in which the greater trochanter of the femur is in its most exposed position when striking the ground places the risk of hip fracture very high in the fall event. Falling at a dangerous rate of acceleration is the indication that the body is moving fast enough that it would contact the ground at an injurious velocity. These three factors must be simultaneously met within the sensor system, which then is relayed to the mechanism within the Tango Belt to deploy the airbags (see image 2)
Image 2
Criteria for Airbag Deployment in the Tango Belt Fall Recognition Algorithm
The best candidates for the utilization of hip protection, including a device such as the Tango Belt, include older adults with risk factors for falling and fragility fracture. The identified population most at risk are older adults who have been diagnosed with osteoporosis, or have at least two risk factors of osteoporosis, or who have had a history of any fracture beyond the age of 50. Individuals who have a history of falls, or fear of falling that limits their participation in daily activity, would also benefit from the smart wearable to reduce fear of falling (Stolee, Poss, Cook, Byrne, & Hirdes 2009; Unnanuntana et al., 2010).
Published studies provide evidence of acceptance and protection from hip fracture (Quigley, Singhatat, & Tarbet, 2019; Tarbert, 2020b). The next section discusses current evidence to support the use of wearable smart hip protection devices.
Acceptance and Feasibility
Recognition of fall and fracture risk are embedded in most admissions and ongoing care assessment examinations in senior care settings. Care planning subsequently includes treatment strategies based upon identified risk factors. Passive hip pad garment-type protectors have traditionally been allocated using this risk identification system, as well as the previously discussed floor mats. Due to the limited acceptance of passive hip protector garments, the wearable smart hip protection device has been introduced to several settings of care. Within, data is collected for analysis that would indicate successful adoption.
Short Term Rehabilitation
Feasibility of the device in short term rehabilitation was established with >70% adherence to care plan orders.Feasibility of the device in short term rehabilitation was established with >70% adherence to care plan orders. The rehabilitation department led the intervention and candidate identification with fall risk and balance training as part of the rehabilitation care plan. Outcomes of this feasibility trial included increased distance over surface from admission to discharge by those who wore the Tango Belt as compared to those who did not wear the belt. Also noted was a reported increase in balance confidence, measured by the short version of the Falls Efficacy Scale International, by an overall average of 22% (Tarbert, 2019).
Long Term Care
Use of the smart wearable in the LTC community setting has been successfully achieved with embedding of the device in the daily grooming and dressing routine for the resident. Many of those who are candidates in this setting wear the hip protection device 24 hours a day as falls occurring overnight with ab lib ambulation are a frequent occurrence. Tango Belt wear is consistently greater than 80% as compared to care plan orders with regular removal of the belt for cleaning, showering, and charging times (Tarbert & Singhatat, 2021). Balance confidence, compliance, daily wear, and postural sway are recorded in the individual wearer dashboard metrics, on the mobile app (see image 3).
Image 3.
Individual Dashboard Metrics

Home and Community Setting
The light-weight aspect of the belt and positioning with individual fitting offers comfort for freedom of use during all functional activities...Utilization of the innovative smart wearable in the home and community setting has also demonstrated strong adherence, especially in cases of users who are internally motivated to avoid fall injuries and when there is supportive caregivers and interdisciplinary approaches applied (Tarbert, 2020a). The application of the smart belt being integrated into daily care and routine for users creates a seamless application process without complications or need of additional equipment. The light-weight aspect of the belt and positioning with individual fitting offers comfort for freedom of use during all functional activities (other than bathing). Incontinence management is not hindered by tightfitting garments or a need to remove the hip protection belt during toileting or clothing management. These aspects of the formfitting smart wearable belt have increased duration of wear across multiple settings.
Artificial Intelligence: Motion-Sensing Decision-Making
In recent years, rapid technological advancement in the fields of low-cost motion sensors; low-power Internet of Things (IoT) devices; and cloud-based scalable systems have made it possible to conduct motion-sensing decision-making on wearable devices (Dang, Piran, Han, Min, & Moon, 2019). Briefly for context, the Internet of Things (IoT) is is the network of connected sensors found throughout our environments in objects we typically wouldn’t expect to have internet connectivity, that constantly share data in communication with a cloud and other sensors. Cloud-based scalable systems are the virtual repository where data is stored and computed to report outcomes when accessed that have the ability to expand and grow in storage and computing abilities with more and more data sources. The utilization of smart devices to continuously monitor health behaviors is growing from counting steps to measuring blood glucose. The 3D sensor that sits on the back of the Tango Belt to continuously monitor human motion can also contribute to the valuable information care providers and individuals are able to gather for critical decision making. We discuss two examples of this below in postural sway and gait patterns.
Postural Sway
Sensors use the placement of the belt to identify the individual’s natural midline posture...Postural sway is often measured in the amount of motion away from the Center of Pressure (CoP) when a human is in standing position. The degrees the body moves away from center can provide valuable insight as to movement produced by the individual during postural challenges (Quijoux et al., 2019). Sensors use the placement of the belt to identify the individual’s natural midline posture and will offer continual understanding of postural sway based upon this midline. The sensor captures this motion throughout the time of wearing the belt while standing upright and moving around.
The data that informs the sensory system platform allows advanced motion/gait analytics on the backend, which operate in the cloud. Capturing this data in real-time during the performance of standing and walking functional movement allows the Tango Belt to deploy airbags as needed in the case of falling that indicates serious, hip-impacting motions from a standing height. This also offers the ability of the belt to capture and share an average degree from postural midline that wears exhibit in their performance of daily activities.
Information about postural reactions to balance and postural disturbances throughout functional life for the wearer can inform clinical care management of strategies critical to reduce risk of falling. Establishment of a “baseline” postural sway with use of the wearable belt can offer insight to individuals and care team members to inform changes in the objective measure of balance. This information can indicate the need for screening and possible intervention to identify the causation of the changed sway metric. Technology is continuing to offer increased real-time variables to inform patient management as well as identification of risk factors.
Gait Patterns
As the use of this wearable continues to feed the algorithm of human motions, the system recognizes movement and postures with ever increasing detail. Computing resources between the deep learning and cloud infrastructure employs advanced machine learning and AI-based techniques to scan the motion, and analyze the wearer motion and gait pattern. This will in turn render valuable insights to view on a dashboard that is accessed via a mobile or desktop app.
Information shared in the app can help the care team better monitor the wearer’s health to make better informed decisions. Information shared in the app can help the care team better monitor the wearer’s health to make better informed decisions. Strengthening of the ability of the sensor and algorithm to improve data sharing capabilities continues with future iterations of the technology. Aspects to be analyzed and reported include gait pattern specifics such as stride time variability and cadence; and index of how much daily activity was performed by the individual. All data points combine to produce analytical evidence to support clinical decision making and the ability to provide interactive platforms for healthcare providers to test functional performance.
Implications for Practice and Research
Healthcare providers have the moral imperative to protect patients from harm when they fall. Nurses continue to have the primary responsibility to implement fall and fall injury prevention programs, which are not working. Not all patients have the same level of injury risk, which requires nurses to implement a population-based approach to injury reduction. Adults aged 85 and older are 10 times more likely to sustain a hip fracture than adults 65 to 69 years (Hung et al., 2012). Also, older adults who sustain hip fractures have greater functional decline, institutionalization, and death. Statistics provide compelling evidence that fall prevention programs must change the paradigm for practice to preventing falls and their injuries. Thus, all efforts should be made to protect older adults from hip fractures across all setting of care.
Nurses continue to have the primary responsibility to implement fall and fall injury prevention programs...Nurses, in collaboration with interdisciplinary team members, are uniquely positioned to integrate AI-assisted hip protector technology and AI-based algorithms into fall and injury prevention programs and patient education programs. Such integration will provide real-time data-based insights into patient adherence with wear and functional performance; these data offer a better source of information about fall risk than a calculated single score. Thus, the technology-based AI system of a wearable device such as the Tango Belt enables safe mobility and protection of hips during a fall event.
The coordinated efforts of nurses and other clinicians to identify and mitigate fall risk (and fall injury risk) creates a culture of mobility and safety for the patient population. Combined work between nurses and rehabilitation therapists to establish appropriate environmental modifications, medication reconciliation, incontinence management, and mobility strategies individualized for the patient with fall risk is a core aspect of care management in the older adult population. Standardization of fall risk screening upon admission into acute and long-term care facilities, as well as reassessment, triggers factors that lead to the increased fall risk.
Patient tolerance...of wearable hip protectors greatly influences the efficacy of these devices.For some individuals, injury risk reduction, even with the best evidence-based mitigation and identification of risk of fall injury, becomes the paramount intervention. Patient tolerance (i.e., utilization) of wearable hip protectors greatly influences the efficacy of these devices. Inclusion of current AI-based technology into the care plan, with consistent communication that supports use and application, can achieve success with adherence.
Evidence confirms that hip protectors are protective (Bulat et al., 2008; Sawka et al., 2007). While no studies have been conducted in hospitals, these devices are being used, though not widely, due to barriers previously discussed. Additional barriers that limit use in practice are staff adherence, product availability, and organizational acceptance. These barriers are setting-dependent and can influence patient knowledge and access to such products (Quigley, 2016). Even considering these barriers to implementation, it is important for nurses to keep abreast of technology innovations to protect vulnerable and at-risk populations from hip fractures.
...it is important for nurses to keep abreast of technology innovations to protect vulnerable and at-risk populations from hip fractures.In clinical practice, hip protector belts should be offered to patients at risk for or with a history of hip fracture. Safety is not setting-specific, but rather is person-specific. Hip protector belts are low cost, low risk interventions to reduce hip fractures from falls. As leaders of interdisciplinary teams, nurses must examine the current best evidence and consider practices to protect patients from injury, while acknowledging that not all falls can be prevented.
Research opportunities to add evidence about smart technology options are vast. The success of any intervention depends upon many variables, such as culture, fidelity, and reliability of implementation; staff and patient attitude; and acceptable and meaningful data on effectiveness and efficiency. More research is needed on Tango Belt and smart technology adoption, utilization, and integration into daily living practices of patients at risk for hip fracture. Patient perceptions and use of smart-technology dashboards to improve gait, balance, and function; reduce fall risks; and protect from hip fractures would contribute valuable knowledge regarding the interaction between innovative technology, patient engagement, and supportive autonomy. Nurse and rehabilitation researchers can develop a collaborative research agenda to test the effectiveness of artificial dashboard metrics and specific populations at greatest risk for falls and evaluate detailed gait and balance patterns that generate models of improved function and reduced fall risk. Finally, research is needed to identify the most effective social marketing solutions to inform prescription of the Tango Belt, supported by evidence, by clinicians for patients at risk for falls and hip fractures.
Conclusion
Many interventions to prevent falls and fall-related injuries have been tested, but they require multidisciplinary support for program adoption and reliable implementation for specific at-risk and vulnerable subpopulations, such as the frail elderly and those at risk for injury. Nurses, as leaders of care teams, introduce innovations into practice through product testing, quality improvement, and research. Working collaboratively, nurses, therapists, and quality improvement specialists can monitor and sustain program implementation to reduce the risk of hip fractures, educate patients about options while they are in our care, and increase adherence. Across populations and settings of care, nurses must care for patients at risk for injury differently than those at risk for falling.
Nurses, as leaders of care teams, introduce innovations into practice through product testing, quality improvement, and research. Limitations to patient use are similar to those of other protective technology: staff attitudes, provider acceptance, product and social marketing, and cost. However, it has become increasingly evident that patient and provider acceptance and use of a belt that looks like a clothing accessory is greater than hip protector clothing that creates the appearance of wider hips. The introduction of clinically relevant patient adherence data from an AI-based, smart technological solution is an important contribution to care to predict and quantify biomechanics, identify fall risks, and protect hips from fall-related fracture. Additional use and data collection can only further inform predictive analytics for risk, individual care management, and treatment effectiveness.
Disclosures
Patricia A. Quigley, Independent Consultant and Fall Prevention Expert, ActiveProtective Technologies, Inc. Rebecca J. Tarbert, Director of Clinical Programs, ActiveProtective Technologies, Inc.
Authors
Patricia Quigley, PhD, MPH, APRN, CRRN, FAAN, FAANP, FARN
Email: pquigley1@tampabay.rr.com
Dr. Quigley, a Nurse Consultant and Nurse Scientist, Retired Associate Director, VISN 8 Patient Safety Center of Inquiry, is both a Clinical Nurse Specialist and a Nurse Practitioner in Rehabilitation. Her contributions to patient safety, nursing and rehabilitation are evident at a national level – with emphasis on clinical practice innovations designed to promote elders’ independence and safety. She is nationally known for her program of research in patient safety, particularly in fall prevention. The falls program research agenda continues to drive research efforts across health services and rehabilitation researchers. Pat is an Independent Consultant with ActiveProtective, Technologies, LLC.
Rebecca J Tarbert, PT, DPT, GCS, CLT
Email: rebecca@aciveprotective.com
Dr. Rebecca Tarbert is a physical therapist and board certified geriatric clinical specialist with 20 years of experience primarily focused on the care and mobility of the older adult. Graduating in 1999, she received her bachelor’s degree in health sciences and master’s degree in physical therapy from the University of the Sciences in Philadelphia and achieved her Doctorate in Physical Therapy from Temple University in 2013. She currently serves as the Director of Clinical Programs with Active Protective Technologies providing clinical insight in the development of technology aimed on supporting the safe mobility of older adults at most risk of fall injuries. Rebecca’s history includes working with large senior care corporate initiatives for fall management, coordination of fall management across setting transitions, authoring, and presenting continuing education courses to rehabilitation providers and providing one on one physical therapy services for older adults. She has presented on topics of wellness, mobility, and evidence-based practice in geriatrics at several national and international conferences including ICAA, APTA, GSA and FFN. Rebecca’s publications have been focused on fall risk awareness, management, mobility participation, fall injury reduction and the role of rehabilitation in geriatric care
References
de Bot, R. T. A. L., Veldman, H. D., Witlox, A., van Rhijn, L. W., & Hiligsmann, M. (2020). Hip protectors are cost-effective in the prevention of hip fractures in patients with high fracture risk. Osteoporosis International, 31(1), 1217-1229. https://doi.org/10.1007/s00198-019-05252-8
Boushon, B., Nielsen, G., Quigley, P., Rutherford, P., Taylor, J., Shannon, F., & Rita, S. (2012). Transforming care at the bedside how-to-guide: Reducing patient injuries from falls. Institute for Healthcare Improvement. Retrieved from: http://www.ihi.org/resources/Pages/Tools/TCABHowToGuideReducingPatientInjuriesfromFalls.aspx
Bulat, T., Applegarth, S., Wilkinson, S., Fitzgerald, S., Ahmed, S., & Quigley, P. (2008). Effect of multiple impacts on protective properties of hip protectors. Clinical Interventions in Aging, 3(3), 1–5. https://doi.org/10.2147/cia.s2529
Bowers, B., Lloyd, J., Lee, W., Powell-Cope, G., & Baptiste, A. (2008). Biomechanical evaluation of injury severity associated with patient falls from bed. Rehabilitation Nursing, 33(6), 253-260. https://doi.org/10.1002/j.2048-7940.2008.tb00237.x
Centers for Disease Control and Prevention (CDC). (2020). Death from older adult falls. Injury Center. Retrieved from: https://www.cdc.gov/falls/data/fall-deaths.html.
Dang L.M., Piran M. J., Han D., Min K., & Moon H. (2019). A survey on internet of things and cloud computing for healthcare. Electronics, 8(7), 768. https://doi.org/10.3390/electronics8070768
Gray-Micelli, D. & Quigley, P. (2020). Assessing, managing, and preventing falls in acute care. In Boltz, M., Capezuti, E., Zwicker, D., Fulmer, T. (Eds). Evidence-based geriatric nursing protocols for best practice (pp. 375-408). Springer Publishing Co.
Hung, W. W., Egol, K. A., Zuckerman, J. D., & Siu, A. L. (2012). Hip fracture management: Tailoring care for the older patient. Journal of the American Medical Association, 307(20), 2185-2194. https://doi.org/10.1001/jama.2012.4842
Holzer, G., & Holzer, L. A. (2007). Hip protectors and prevention of hip fracture in older persons. Geriatrics, 62(8), 15-20. https://pubmed.ncbi.nlm.nih.gov/17668960/
Kannus, P., Parkkari, J., Niemi, S., Pasanen, M., Palvanen, M., Jarvinen, M., & Vuori, I. (2000) Prevention of hip fractures in elderly people with the use of a hip protector. New England Journal of Medicine, 343(21), 1506-13. https://doi.org/10.1056/nejm200011233432101
Korall, A. M. B., Loughin, T. M., Feldman, F., Cameron, I. D., Leung, P. M., Sims-Gould, J., Godin, J., & Robinovitch, S. N. (2018). Determinants of staff commitment to hip protectors in long-term care: A cross-sectional survey. International Journal of Nursing Studies, June, 82: 139-148. https://doi.org/10.1016/j.ijnurstu.2018.03.014
Levant, S., Chari, K., & DeFrances, C. J. (2015). Hospitalizations for patients age 85 and over in the United States, 2000-2010. NCHS Data Brief. No. 182. Retrieved from: https://www.cdc.gov/nchs/data/databriefs/db182.pdf
Neuman, M. D., Silber, J. H., Magaziner, J. S., Passarella, M. A., Mehta, S., & Werner, R. M. (2014). Survival and functional outcomes after hip fracture among nursing home residents. Journal of the American Medical Association Internal Medicine, 174(8), 1273-1280. https://doi.org/10.1001/jamainternmed.2014.2362
Oliver, D., Healey, F., & Haines, T. (2010). Preventing falls and fall-related injuries in hospitals. Clinics in Geriatric Medicine, 26(4), 645-692. https://doi.org/10.1016/j.cger.2010.06.005
Quigley, P. (2016). Evidence levels: Applied to select fall and fall injury prevention practices. Rehabilitation Nursing, 41(1), 5-15. https://doi.org/10.1002/rnj.253
Quigley, P. A., Singhatat, W., & Tarbet, R. J. (2019). Technology innovation to protect hips from fall-related fracture. Physical Medicine and Rehabilitation Research, 4(3), 1-4. https://doi.org/10.15761/PMRR.1000205
Quijoux, F., Vienne-Jumeau, A., Bertin-Hugault, F., Lefèvre, M., Zawieja, P., Vidal, P. P., & Ricard, D. (2019). Center of pressure characteristics from quiet standing measures to predict the risk of falling in older adults: A protocol for a systematic review and meta-analysis. Systematic Reviews, 8(1), 232. https://doi.org/10.1186/s13643-019-1147-9
Rubenstein, L. (2000). Hip protectors: A breakthrough in fracture prevention. New England Journal of Medicine, 343(21), 1562- 1563. https://doi.org/10.1056/nejm200011233432109
Sawka, A. M., Boulos, P., Beattie, K., Papaioannou, A., Gafni, A., Cranney, A., Hanley, D. A., Adachie, J. D., Papadimitropoulos, E. A., & Thabane, L. (2007). Hip protectors decrease hip fracture risk in elderly nursing home residents: A Bayesian meta-analysis. Journal of Clinical Epidemiology, 60(4), 336–344. https://doi.org/10.1016%2Fj.jclinepi.2006.07.006
Shekelle, P. G., Wachter, R. M., Pronovost, P. J., Schoelles, K., McDonald, K. M., Dy, S. M., Shojania, K., Reston, J., Berger, Z., Johnsen, B., Larkin, J. W., Lucas, S., Martinez, K., Motala, A., Newberry, S. J., Noble, M., Pfoh, E., Ranji, S. R. … Winters, B. D. (2013). Making health care safer II.: An updated critical analysis of the evidence for patient safety practices. Agency for Healthcare Research and Quality. Retrieved from: http://www.ahrq.gov/research/findings/evidence-based-reports/ptsafetyuptp.html
Smeesters, C., Hayes, W. C., & McMahon, T. A. (2007). Determining fall direction and impact location for various disturbances and gait speeds using articulated total body model. Journal Biomechanical Engineering, 129(3), 393-399. https://doi.org/10.1115/1.2737432
Soncrant, C., Neily, J., Bulat, T., & Mills, P. (2020). Recommendations for fall-related injury prevention. Journal Nursing Care Quality, 35(1), 77-82. https://doi.org/10.1097/ncq.0000000000000408
Stolee, P., Poss, J., Cook, R. J., Byrne, K., & Hirdes, J. P. (2009). Risk factors for hip fracture in older home care clients. The Journals of Gerontology; Series A, 64A(3), 403-410. https://doi.org/10.1093/gerona/gln035
Tarbert, R. J. (2019). Role of rehabilitation in innovative models for mobility in the short-term care setting. HSOA Journal of Physical Medicine, Rehabilitation, & Disabilities, 5, 035. https://doi.org/10.24966/PMRD-8670/100035
Tarbert, R. J. (2020a). Hip fractures can be prevented with use of emerging technology. Journal of Emergency Medicine Trauma and Surgical Care, 7, 040. https://doi.org/10.24966/ETS-8798/100040
Tarbert R. J. (2020b). Multi-factorial management of fall risk in the home setting with use of innovative technology: A case study. International Journal of Studies in Nursing, 5(4), 12- 15. https://doi.org/10.20849/ijsn.v5i4.830
Tarbert, R. J., & Singhatat, W. (2021). Skilled nursing resident adherence with wearable technology to offer safer mobility and decreased fall injuries. Journal of Patient Safety and Risk Management, 26(1), 41-45. https://doi.org/10.1177%2F2516043520979193
Unnanuntana, A., Gladnick, B. P., Donnelly, E., & Lane, J. M. (2010). The assessment of fracture risk. The Journal of Bone and Joint Surgery American, 92(3), 743-753. https://doi.org/10.2106%2FJBJS.I.00919
van Schoor, N. M., Asma, G., Smit, J. H., Bouter, L. M., & Lips, P. (2003). The Amsterdam hip protector study: Compliance and determinants of compliance. Osteoporosis International, 14(4), 353-359. https://doi.org/10.1007/s00198-003-1382-7
Yang, Y., Komisar, V., Shishov, N., Lo, B., Korall, A., Feldman, F., & Robinovitch, S. N. (2020). The effect of fall biomechanics on risk for hip fracture in older adults: A cohort study of video-captured falls in long-term care. Journal of Bone and Mineral Research, 35(10), 1914- 1922. https://doi.org/10.1002/jbmr.4048
Zubkoff, L., Neily, J., Quigley, P., Delanko, V., Young-Xu, Y., & Mills, P. (2018). Preventing falls and fall-related injuries in state veterans’ homes: Virtual breakthrough series collaborative. Journal of Nursing Care and Quality, 33(4), 334-340. https://doi.org/10.1097/ncq.0000000000000309

