Poor communication within the healthcare team often leads to negative patient outcomes and diminishes patient perception of quality care. Literature has shown that healthcare team communication has been inconsistent, contributing to worsened patient outcomes and negative patient perceptions of care. This project examined the effect of an asynchronous, standardized virtual huddle on healthcare team engagement and the patient experience, as compared to the usual static huddles. We compared pre-and post-scores over a four week implementation period for healthcare team member huddle participation and patient experience scores on a national level survey. Findings demonstrated a statistically significant difference in team member participation between in-person static and asynchronous virtual huddle huddles, and a statistically significant difference in patient experience scores after virtual huddle implementation. The use of a virtual huddle promoted more inclusive engagement in communication within a unit by interdisciplinary providers, and also demonstrated improved patient perceptions of care during the time of its use. Findings from this project support that novel virtual huddles improved healthcare team engagement and the patient experience and may promote safer delivery of healthcare.
Key Words: communication, huddle board, virtual huddle, healthcare team, patient experience, interprofessional team, HCAHPS, patient experience, patient perception of care
Poor communication within the healthcare team leads to negative patient outcomes and diminishes patient perception of quality careCommunication has a direct effect on every outcome in the healthcare environment. Errors and patient safety directly relate to poor communication due to a lack of communication standards (Elkin et al., 2016). Poor communication within the healthcare team leads to negative patient outcomes and diminishes patient perception of quality care(Babiker et al., 2014; Burgener, 2017; McFarland et al., 2017). Miscommunication has contributed to 80% of serious medical errors and sentinel events (The Joint Commission, 2016; Burgener, 2017).
Communication failures precede healthcare errors and drive healthcare costs upward.Communication failures precede healthcare errors and drive healthcare costs upward. Gooch (2016) asserted that miscommunications in healthcare cost close to 1.7 billion in malpractice suits annually. Furthermore, communication failure has been identified as a foundational cause of unintentional patient harm and is responsible for 30% of malpractice cases (Bailey, 2016). As healthcare transforms into a value-based system, the importance of cost reduction and efficiency is more critical than ever before. Patients and healthcare teams must change quickly to improve patient safety through better, innovative communication techniques and decrease costs to all. Unfortunately, communication failures prevent improvements in the quality-of-care patients receive.
Background
The Concept of Huddles
In 1883, Paul Hubbard, a Gallaudet University football player, discovered a focus of attention of teammates on the field when communicating. This was the dawn of a huddle (Kelly, 2016). The huddle is a form of team communication utilized in healthcare to improve quality and thus has encouraged quality improvement (Agency for Healthcare Research and Quality [AHRQ], 2019). Today, in healthcare settings, huddles are part of the safety practice of almost all acute care facilities huddles are part of the safety practice of almost all acute care facilities(AHRQ, 2017). The use of a standardized method of communication, such as a huddle, provides healthcare team members with consistency and improves the patient experience through the efficient interchange of ideas and information (AHRQ, 2019; Institute for Healthcare Improvement [IHI], 2020).
Huddles and Team Communication
Communication among healthcare team members requires consistent and timely information exchanges to provide care that is seamless for patients. However, literature has shown that healthcare team communication has been inconsistent and has contributed to worsened patient outcomes and negative patient perceptions of care (Scoville et al., 2016, Burgener, 2017; Shahid & Thomas 2018; The Joint Commission [TJC], 2017). Finding effective methods of interdisciplinary dialogue is essential; moreover, ensuring team communication is clear and informs members of pertinent information is absolute (Chou & Cooley, 2018; Femstrom et al., 2016). Tools that facilitate frequent and effective team communication, such as huddle boards, have been translated into patient care improvements (IHI, 2020; AHRQ 2017). Team STEPPS 2.0 introduced the idea of team training and included the importance of huddles as part of the team dynamics to prevent patient harm and improve the quality of patient care (AHRQ, 2019). Additionally, huddle communication improved healthcare quality and solved problems within a group (Ore et al., 2019; Scoville, 2016). Huddles provided an outlet for healthcare team members to engage in care concerns and problem-solving skills. Huddles also promoted team cohesion (Sherman, 2017).
Huddle Boards versus Virtual Huddles
Huddle boards are a static tool that visualize team goals and plans for healthcare delivery.Huddle boards are a static tool that visualize team goals and plans for healthcare delivery. While the literature has shown that huddle boards promote better outcomes, barriers to participation exist. During huddles in a unit, typically a “board” is used, which is a static tool that documents visual aspects of the team goals and plans for healthcare delivery. However, a virtual huddle provides an electronic way of communicating with technology in an ongoing manner (Martinelli, et al., 2017). Newer technology promotes innovative ways to collaborate and communicate within the interdisciplinary team. Romano (2024) identified virtual huddles as a way to improve the distribution of information among the healthcare team. The virtual huddle provides a team with a tool for partnership and problem-solving beyond one shift or one moment in time.
Huddling with the Healthcare Team
The paradigm shift toward healthcare delivery as a collaborative team required a succinct communication style to ensure clear exchanges of ideas and plans for care. Team communication provides the most useful information for the patient and improves patient satisfaction (Wen & Schulman, 2014). Literature has shown miscommunication among the team leads to hospital readmissions, higher costs to patients and facilities, and poor patient experiences (McIlvennan et al., 2015; Will et al., 2019). Creating an environment of open communication and relationships among team members encouraged a climate of safety and increased quality of care (Bhatt & Swick, 2017; Chou & Cooley, 2018). ...miscommunication among the team leads to hospital readmissions, higher costs to patients and facilities, and poor patient experiences
Encouraging team communication requires a safe space, a flexible platform for exchange to happen, and direction when needed from team leaders. When multiple people interact, the chance of barriers to communication is high; there must be standards to prevent miscommunications (Babiker et al., 2014; Childress, 2015). In previous studies, standardization of communication between all healthcare team members helped to ensure active participation (Handberg & Voss, 2018). As the interprofessional team approach continues to establish the new norm, the need for efficient communication becomes vital to providing safe and quality care.
Patient Safety and Outcomes
The patient is the central core of the healthcare team. Positive patient outcomes are the driving force behind healthcare; everyone wants to feel well. Furthermore, measurements of patient outcomes now drive reimbursement (Shryock, 2019). Patient experience in the healthcare setting is measured through administration of a national, standardized survey after hospital or clinic care is provided (Centers for Medicare and Medicaid [CMS], 2019). Scores from this survey, the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), are used by CMS to measure the patient experience within the healthcare arena (CMS, 2019).
HCAHPS standards are the same across all healthcare systems in the United States, and therefore, the results are transferable and interpreted similarly across healthcare entities (CMS, 2019). Research has shown that HCAHPS scores have a direct relationship between the patient experience and healthcare team communication (Burgener, 2017). High patient experience scores and compliance with self-care measures are linked to positive effective communication (McFarland et al., 2017; Newcomb et al., 2018). Patient experience scores are important to understand the patient’s perspective of care and help to identify quality improvement needs in the healthcare setting.
Miscommunication, Costs, and Safety
Inconsistent communication styles between team members lead to communication barriers and breakdowns in care.Effective communication between team members and patients is imperative in a healthcare setting. However, inconsistent communication among healthcare team members affects patient safety and the perception of care provided. Inconsistent communication styles between team members lead to communication barriers and breakdowns in care. Therefore, establishing standards in communication with the healthcare team is essential to minimize disruptions and improve team dynamics (Shahid & Thomas, 2018). Listening is a vital part of effective communication; interruptions during speaking occur within 11 seconds in most encounters (Ospina et al. 2018). When multiple people interact, the chance of barriers to communication is high, and there must be standards to prevent these miscommunications (Childress, 2015).
Additionally, stressful situations in the healthcare environment can augment miscommunications (Kraut, 2018). When communication is most vital, the risk for miscommunication leading to sentinel events is highest. Childress (2015) suggested that communication assumptions happen in healthcare, and the goal of excellent communication is to ensure that all team members understand the exchange. Providing a standardized tool for team communications enhances quality and safety on medical-surgical floors (Shahid & Thomas, 2018). Teams who practice excellent communication all the time are less likely to have difficulty communicating in stressful situations, such as caring for a declining patient or emergent care concerns (Babiker et al., 2014). Teams who practice excellent communication all the time are less likely to have difficulty communicating in stressful situations...
Project Aim and Scope
While literature has indicated that team communication needs standardization (AHRQ, 2017), a gap in the literature existed as to what method of standardization was most effective (Chou & Cooley, 2016). The aim of this project was to examine the effect of an asynchronous, standardized virtual huddle on the patient experience and healthcare team engagement. The following clinical questions guided the project:
- Will a virtual asynchronous huddle increase healthcare team participation in the huddle process?
- Will a virtual huddle, by improving healthcare team participation, improve patients' perceptions of care as demonstrated through increased patient experience scores?
At the selected project site, static huddles consisted primarily of the unit nurses, and it was noted attendance was minimal. The identified lack of participation in static huddles contributed to the disconnection between communication and engagement in the wider healthcare team. Therefore, we proposed that an ongoing virtual electronic huddle with embedded communication training might facilitate participation and engagement and identify safety or care concerns to improve patient experience. We had several factors to consider:
- The project site used static huddles to encourage quality improvement in the processes but reported that the process was scattered and inconsistent due to the synchronous nature of the huddle.
- Team members were not always available at designated huddle times. Therefore, all team members did not have the opportunity to provide input in the process of quality improvement through huddles.
- The project site provided relationship-centered communication training for all physicians and advanced practice providers as part of the orientation process through the Patient Experience Team. This training, the ART of Communication, is an 8-hour in-person workshop. However, while other healthcare team members technically had the option to take the ART of Communication training, most had difficulty scheduling time for the course due to the length of the workshop. Therefore, non-physician/non-advanced practice providers rarely received any formal communication training.
This project sought to examine a virtual huddle option that allowed interdisciplinary healthcare team members to participate in the quality improvement process of a virtual huddle at an acute care facility through the use of asynchronous technology.
Project Methods
Theoretical Foundation
Two theoretical frameworks guided this project. Watson's (2008) Human Caring Theory provided a framework to construct caring communications and caring units to improve healthcare. Application of Watson's (2008) human caring theory concepts were embedded in this project in building positive team dynamics and trust through huddle interactions and safe communication.
The second framework used in this project was the relationship-based communication by Chou and Cooley (2018). An application of Chou and Cooley's model (2018) included the communication skillset of ask, respond, and tell, or the “ART” of Communication. The application of relationship-based communication (RCC), skills were used by the healthcare team to drive a team-centered approach to interactions within the inpatient setting. The RCC skillset intervention included training in using specific phrases during the communication exchange of huddle attendees.
The RCC intervention was utilized to improve communications between patient and provider and was also applied to healthcare team members to improve team communications. The relationship-centered communication style utilized in this project was based on three areas: rapport, perspectives, and teach-back. Building rapport consists of establishing rapport quickly, developing trust and gathering a list of concerns. Understanding the perception of others is accomplished through open-ended conversations, naming emotions, and using empathy. The final stage of RCC is closing the encounter by ensuring understanding through a technique called teach-back. In teach-back we share information through listening rather than telling, to ensure what the other person understands and what may need further explanation or education. During the virtual huddle, these steps were both utilized to facilitate the conversation and encouraged to be practiced in day-to-day activities for each participant.
Design and Setting
A quasi-experimental, pretest, and posttest intervention design was used to examine the effect of using a virtual huddle on 1) patient satisfaction scores on eight communication items on the HCAHPS survey, and 2) participation of healthcare team members in the huddle. The HCAHPS survey has eight communication questions that discuss nurses and doctors listening carefully during hospitalization (two questions); nurses and doctors explaining things in a way the patient can understand (two questions); explaining medications in a way the patient could understand during hospitalization (two questions) and finally, patient understanding after discharge regarding care and medication (two questions).
The project site was two acute care medical-surgical units in a Level 1, Magnet-recognized trauma center, 636-bed acute care hospital. This project was approved by the facility institutional review board. Coincidentally, we carried out the project over four weeks, from March 2020 through May 2020 at the very beginning of the COVID-19 pandemic.
Participants
We recruited a convenience sample of interprofessional healthcare team members (n=18) on two acute care hospital units. Healthcare team members included registered nurses (RNs), licensed vocational nurses (LVNs), physicians, social workers, pastoral care staff, ancillary staff, and residents. All healthcare team members in the two units were invited to participate in static and virtual huddles. During the static huddle participants were informed of the virtual huddles and then all potential staff on the two units received an email inviting them to participate in the virtual huddle. If they chose to participate, a link took them to the virtual huddle option.
Huddle Procedures
Usual Static Huddle. On the units, healthcare members conducted a daily huddle once per shift using a traditional static board. Data on the static huddle board included times and locations for huddles, participation, risks, hazards, and methods to improve patient safety.
Intervention Virtual Huddle. The intervention in this project was to transform the current static huddle by implementing a virtual version of the huddle to encourage the building of team collaboration (Karpeh & Bryczkowski, 2017; Persky, 2011). The new The new virtual huddle continued the same strategic operations and content as prior huddles but added communication strategies...virtual huddle continued the same strategic operations and content as prior huddles but added communication strategies using the ART of Communication training concepts from a program developed by the organization in partnership with the Academy of Communication in Healthcare (2020) to provide a standard way of communication across the healthcare organization. The communication strategies were deployed using a secure, intranet version of the application, Yammer. This application allowed non-synchronous communications between team members, similar to a social media site.
The virtual huddle began each day with a relationship-centered communication tip and training from the skillset that focused on building rapport, listening, or ‘paying attention’ and assessing understanding (Academy of Communication in Healthcare, 2020).The healthcare team was a central focus for the huddle portion of the project, whereas the patient was the central focus of the care received. The virtual huddle provided an ongoing electronic method of communication that could be held remotely rather than standing by a static board in the unit. The virtual huddle was also “available” at all hours of the day. The virtual huddle was also “available” at all hours of the day.
Project Measures
Static Huddle Tracking. The first variable, healthcare team member participation in the huddle, was measured through daily participation tallies. In the static (i.e., traditional, in-person) huddle, a person shows up, places his or her name on a board and then is counted as participating, no additional steps are required to be ‘counted’ in the huddle. Huddle participation via the “huddle audit” was tracked daily and logged for reporting to the nursing director and then monthly to the facility. The Data trends yielded limited input from the team.baseline data were derived from daily tracking logs for a period of 12 weeks before establishing a weekly and daily average participation score. Data trends yielded limited input from the team. Although huddle communication exchange included a discussion of data on the board, participation was minimal, sometimes without attendance.
Virtual Huddle Tracking. Participation for the asynchronous virtual huddle was in an electronic form and allowed for similar daily tallies. Virtual huddle participation was measured electronically when the team members replied to the initial posts for the huddle. The huddle was provided daily via Microsoft SharePoint, and participants were able to reply to the initial and subsequent posts. Each reply counted as additional participation. The participants in the virtual huddle had to do more than show up, they were required to actively make a statement or ask a question to be counted as a participant. Participation numbers were tabulated for each reply on each day of the post over four weeks of data collection. The asynchronous huddle enabled the healthcare team members to participate more than once in a single huddle; therefore, the need for an additional measurement became evident, leading to the calculation of the number of times a single member participated in a single huddle, which was an unexpected finding as part of the project. Virtual huddle participation data for the four weeks were then compared to baseline static huddle participation data. The participants in the virtual huddle had to do more than show up...
Patient Perception Tracking. The second variable was patient perceptions of care as demonstrated through increased patient satisfaction scores calculated by the HCAHPS survey. The Cronbach α for the HCAHPS survey is 0.97 (Press Ganey, 2010). The reliability and validity of HCAHPS scores have been established since 2005 through numerous studies demonstrating reliable analysis for the instrument (CMS, 2019; Westbrook, et al., 2014).
Press Ganey, as a third-party surveyor, provided real-time results in a percentile ranking as opposed to the open-source website that provides public results but often for a longer timeline (Press Ganey, 2017). The Press Ganey results utilized for this project provided real-time results that matched the project timeline, which is called a Comparison Quick Report. The HCAHPS survey data baseline was established from the scores 60 days before the intervention and included only the domains for communication (8 items). The HCAHPS survey data were then reviewed 30 days post-intervention to assess for changes in the scores. Questions are scored on a Likert-like scale from 1 (never) to 4 (always). The culmination of these questions provided a score that represented the overall patient satisfaction with the communications received during hospitalization. Data from Press Ganey provided to the facility were reported and shared with the project units.
Data Analysis
Data were analyzed using inferential statistics in Statistical Package for Social Sciences (SPSS) v26. Descriptive statistics for demographics of the healthcare team participants were completed. A McNemar test was used to determine if there was a difference between the variables of two related groups, the healthcare team participants in a static huddle before the intervention, and the healthcare team participants during the virtual huddle project. Data for patient perceptions of care through patient experience scores were evaluated using the HCAHPS scores reported by Press Ganey. Pre and post intervention data for patient satisfaction scores (n=88) were collected. Analysis was completed using an independent samples t-test was used to determine whether the HCAHPS score differed for patients who were among the static huddle group, or the patients were among the virtual huddle group.
Results
Demographics
Healthcare team participants were primarily female, with 88.9% (n=16) women and 11.1% (n=2) men. Educational attainment data demonstrated that the majority held a bachelor’s degree in nursing (n=7). Other degrees included associate degrees and doctoral degrees, as seen in Table 1.
Table 1. Educational Attainment of Healthcare Team Participants
|
Level of Education |
N |
Percent |
|---|---|---|
|
Associate degree (non-nursing) or Less |
4 |
22.2% |
|
Associate Degree in Nursing (ADN) |
5 |
27.8% |
|
Bachelor of Science in Nursing (BSN) |
7 |
38.9% |
|
Master of Science in Nursing (MSN) |
0 |
0 |
|
Doctorate (any field) |
2 |
11.1% |
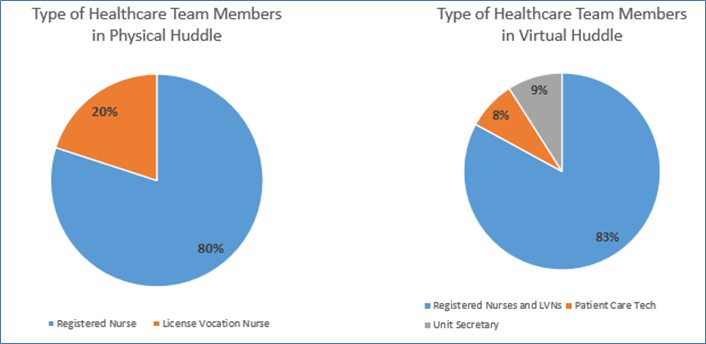
A comparison of type of healthcare team members in each type of huddle is demonstrated in Figure 1.
Figure 1. Types of Healthcare Team Members in Huddle
Huddle Participation
Regarding healthcare team member participation, the McNemar test determined a statistically significant difference in the proportion of the healthcare team member participants pre- and post-intervention, p = .002. The change in participation after the virtual huddle was statistically significant as seen in Table 2. The intervention goal was to increase huddle participation, and the demonstrated increase in participation suggests a positive change.
Table 2. Healthcare Team Member Participation (Over Four Weeks)
|
Participation |
Static Huddle (In Person) |
Virtual Huddle (Intervention) |
|---|---|---|
|
Total Number of Healthcare Team Member Participants Weekly Participation |
8 |
18 |
|
Total Number of Times Participating Over 4-Week Timeline |
26 |
210 |
Patient Perception of Care
Results demonstrated a significant difference in HCAHPS scores between the static huddle and the virtual huddle post-intervention.Pre- and post-intervention means of the HCAHPS survey scores related to the communication components were provided. An independent samples t-test was used to determine whether the mean HCAHPS score differed from pre-intervention to post-intervention scores. The HCAHPS scores range from 1-100. The mean score for the static huddle was M = 76.0, SD = 0.13 and the HCAHPS mean score for the virtual huddle was M = 79.27, SD = 0.14, (t (86) = -98.75, p = .000). Results demonstrated a significant difference in HCAHPS scores between the static huddle and the virtual huddle post-intervention. A Levene test for equality of variances was completed and indicated that the variances of the HCAHPS scores of the two groups did not differ significantly, F(1, 86) = 2.84, p > 0.096; therefore, the assumption is homogeneity assumption of variance is met, and equal variance is assumed.
Discussion
Healthcare Team Participants
The findings of this virtual huddle project showed an increase in participation in the new huddle and patient experience scores were higher. These findings are in alignment with previous literature about using huddles to promote team communication and better patient outcomes (AHRQ, 2017). The outcomes of this project suggested that healthcare team members are ready and open to accepting innovative technology that would improve communication. The virtual huddle offered a modality for more individuals on the healthcare team to participate, and participation increased compared to the current traditional methods.
Findings also demonstrated that healthcare team members participated multiple times over a shift, implying that ongoing communication was important. This was an unexpected finding, in that while there were only 18 healthcare team members who participated, the virtual huddle participation had multiple “postings” each day by these participants, greatly surpassing the static huddle. The virtual huddle acquired momentum between team members to acknowledge suggestions, build rapport to address weaknesses, and offer leadership for needed improvement, which is the original purpose of huddling. Findings also demonstrated that healthcare team members participated multiple times over a shift, implying that ongoing communication was important.
Healthcare teams complete endless quality checks that promote continuous improvement. The virtual huddle allowed participants to participate outside the standard set huddle times, which increased opportunities for involvement. Additionally, the virtual huddle enabled team members to be in different locations but remain connected for communications through the use of either a smartphone or computer. Moreover, team members who may experience communication apprehension are more apt to be involved in asynchronous communications than face-to-face encounters. During the project one unit manager shared that some participants in the virtual huddle had never attended the regular huddle. The virtual huddle may have offered a safe venue and empowered these team members to express opinions and ideas without physical confrontation, increasing diversity in thoughts and ideas. ...one unit manager shared that some participants in the virtual huddle had never attended the regular huddle.
In addition, during a pandemic or disaster crisis, such as COVID-19, virtual huddles allowed for ongoing and streamlined communication that would otherwise have been unavailable due to social distancing requirements or other priorities. Finally, implementing a virtual huddle offered access to providers from multiple interprofessional disciplines who otherwise did not attend the usual static huddle, thus an opportunity to participate in patient care and quality improvement initiatives.
Patient Experience Perspectives
Another consideration from this project was the significant difference in HCAHPS scores between the static huddle and the virtual huddle post-intervention. This outcome may translate into higher-quality communications among the healthcare team and patients. When patients perceive quality care, patient satisfaction and experience increases. The findings in this project support the conclusions made by Wen and Schulman (2014) that team communication provides the most helpful information for the patient and improves patient experience.
Furthermore, higher scores on the HCAHPS post-intervention also support the idea that quality healthcare team communication increases positive perceptions of care, as postulated by McFarland et al. (2017). Because the patient experience is part of CMS reimbursement, use of the virtual huddle may influence reimbursement and reduce costs. Furthermore, improved communication and frequency of communication may decrease sentinel events and errors. The results of this project may not be generalized because of the small number of participants but nonetheless offer strategies to promote alternative methods to facilitate interdisciplinary participation in huddle format and promote positive patient experiences and outcomes.
Limitations
Convenience sampling was a limitation to this project, as well as the small sample size. Another limitation was that the healthcare team members varied in number and areas of expertise every day. The literature review had limitations, as it offered little specificity on the varied use of huddle boards and was not specific to virtual huddle board tools (Lubinesky et al., 2015). Additional limitations included the use of technology in the setting, specifically participant comfort with the technology. The project inception was at the beginning of the COVID-19 pandemic and was launched after the pandemic was in full force. This greatly affected personnel, physical huddle norms and staffing in all healthcare units. The project was initially planned for eight weeks and had to be reduced to four weeks due to pandemic challenges.
Lastly, the third-party surveyor data collection timelines using HCAHPS scores were a limitation. The HCAHPS survey rotates, sent within a timeframe of discharge from a facility. The timeliness of responses to the survey is random and complex. The HCAHPS survey is completely voluntary on the part of the patient (i.e., patients may decline to participate, and their views are then not reflected). Surveys are deployed from 48 hours to six-weeks post discharge; with the short to timeframe of this project, an association may not provide exact representations of the patients served within the time constraints of the project (CMS, 2019).
Conclusion
Changing huddle participation in healthcare is essential. Engagement and diverse input have never mattered more in healthcare. Engagement and diverse input have never mattered more in healthcare.Findings from this project support that novel virtual huddles improve healthcare team engagement, and the patient experience. The virtual huddle provided the healthcare team with multiple, dynamic opportunities to engage a diverse group of team members without a static timeline. During the height of the COVID-19 pandemic, the virtual huddle provided a new avenue of communication for the healthcare team and proved very timely during an unprecedented occurrence. The virtual huddle provided a communication outlet when social distancing was a requirement. This project adds to the literature on communication among healthcare teams and the use of technology to improve communication and patient satisfaction. Adopting and standardizing the use of virtual huddle processes and offering an asynchronous option for huddling may result in a safer delivery of healthcare for all.
Declaration of Conflicts of Interest: None. Authors have no financial, competing, or personal relationship disclosures related to this work. No funding was received for this work.
Authors
Stacy D Cooper, DNP, RN, NEA-BC
Email: Stacy.cooper@bswhealth.org
ORCID ID: 0000-0001-5332-6432
Stacy D. Cooper is currently a Manager of Quality Improvement/Patient Experience at Baylor Scott and White Health. Dr. Cooper has 27 years of nursing and leadership experience. She holds a DNP from Grand Canyon University, an MSN in Nursing Education from Angelo State University, and BSN from University of Texas Arlington. She is also board certified as a Nurse Executive-Advanced. Dr. Cooper serves on the American College of Surgeons Curriculum Committee, Baylor Scott and White Health Women’s Health Council; is Chair of the Baylor Scott and White System Nursing Research Council; and is a peer reviewer for various journals and conference abstracts.
Kathy Smith, EdD, APRN, FNP-BC, ACNP-BC
Email: kss123@txstate.edu; cksmith1975@yahoo.com
ORCID ID: 0000-0001-6173-1809
Dr. Kathy Smith is the Graduate Program Director and an Assistant Professor at Texas State University. Dr. Smith has 21 years of experience in nursing practice, education, and higher education administration. In addition to Associate and BSN Degrees in Nursing from New Mexico State University, she earned an MSN in Nursing Tech at University Health Science Center. Dr. Smith holds an EdD in Leadership Administration in Higher Education from the University of Mary Hardin Baylor. She is dually board-certified as an Advanced Practice Registered Nurse in Acute Care and Family Practice. Her research endeavors include perceptions of support for academic nursing administrators, innovation and improvement in graduate nursing education, and health disparities in the LGBTQI community.
References
Academy of Communication in Healthcare. (2020). Better communication. Better relationships. Better care. Retrieved from https://www.achonline.org/About-ACH/Mission-Vision.
Agency for Healthcare Research and Quality. (2019). Team STEPPS 2.0. Retrieved from https://www.ahrq.gov/teamstepps/instructor/index.html.
Agency for Healthcare Research and Quality. (2017). Daily huddle component kit. Retrieved from https://www.ahrq.gov/hai/tools/ambulatory-surgery/sections/sustainability/management/huddles-comp-kit.html
Agency for Healthcare Research and Quality. (2017). What is patient experience. Retrieved from https://www.ahrq.gov/cahps/about-cahps/patient-experience/index.html
Bailey, M. (2016). Communication failures linked to 1,744 deaths in five years, U.S. malpractice study finds. STAT News. Retrieved from https://www.statnews.com/2016/02/01/communication-failures-malpractice-study/
Babiker, A., El Husseini, M., Abdurrahman, A. N., Abdurrahman, A. F., Juryyan, N. A., Mohamed, O. F., & Zamil, F. A. (2014). Current opinion healthcare professional development: Working as a team to improve patient care. Sudanese Journal of Pediatrics, 14(2), 9-16.
Bhatt, J., & Swick, M. (2017). Focusing on teamwork and communication to improve patient safety. American Hospital Association. Retrieved from https://www.aha.org/news/blog/2017-03-15-focusing-teamwork-and-communication-improve-patient-safety
Burgener, A. (2017). Enhancing communication to improve patient safety and increase patient satisfaction. Health Care Manager, 36(3), 238-243. https://doi.org/10.1097/HCM.0000000000000298
Center for Medicare & Medicaid Services, (2019). HCAHPS: Patients' perspectives of care survey. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS
Chou, C. & Cooley, L. (2018). Communication Rx transforming healthcare through relationship-centered communication. New York, NY: McGraw Hill Education.
Childress, S.B. (2015). Team communications: It's about patient safety. American Society of Clinical Oncology 11(1). https://doi.org/10.1200/JOP.2014.002477
Elkin, P.L., Johnson, H.C., Calahan, M.R., & Classen, D.C. (2016). Improving patient safety reporting with the common formats: Common data representation for patient safety organizations. Journal of Biomedical Informatics 64(2016), 116-121. https://doi.org/10.1016/j.jbi.2016.09.020
Femstrom, K. M., Shippee, N. D., Jones, A. L., & Britt, H. R. (2016). Development and validation of a new patient experience tool in patients with serious illness. BMC Palliative Care, 15, 99. https://doi.org/10.1186/s12904-016-0172-x
Gooch, K. (2016). The chronic problem of communication: Why it's a patient safety issue, and how hospitals can address it. Becker's Clinical Leadership and Infection Control Journal. Retrieved from https://www.beckershospitalreview.com/quality/the-chronic-problem-of-communication-why-it-s-a-patient-safety-issue-and-how-hospitals-can-address-it.html
Handberg, C. & Voss, A.K. (2018). Implementing augmented and alternative communications in critical care settings: Perspectives of healthcare professionals. Journal of Clinical Nursing 27(1-2), 102-114. https://doi.org/10.1111/jocn.13851
Institute for Healthcare Improvement. (2020). Huddles. Retrieved from http://www.ihi.org/resources/Pages/Tools/Huddles.aspx
Karpeh, M.S., & Bryczkowski, S. (2017). Digital communications and social media use in surgery: how to maximize communication in the digital age. Innovative Surgical Science. https://doi.org/10.1515/iss-2017-0019
Kelly, K. (2016). The football huddle: When was it first used? America Comes Alive. Retrieved from https://americacomesalive.com/2016/10/05/the-football-huddle-when-was-it-first-used/
Kraut, N. (2018). Effects of poor communication patterns between nurses and providers. Retrieved from https://www.healthstream.com/resources/blog/blog/2018/12/03/the-impact-of-poor-communication-patterns-between-nurses-and-providers
Lubinesky, M. (2015). Huddle up for patient safety. Retrieved from https://www.myamericannurse.com/huddle-patient-safety/
Martinelli, R.J., Waddell, J.M. & Rahschlte, T.J. (2017). Project without boundaries: Successfully leading teams and managing projects in a virtual world. Hoboken, New Jersey: John Wiley & Sons Inc.
McFarland, D.C., Johnson, S.M., & Holcombe, R.F. (2017). Predictors of satisfaction with doctor and nurse communications: A national study. Health Communications 32(10), 1217-1224. https://doi.org/10.1080/10410236.2016.1215001
Mcllvennan, C. K., Eapen, Z. J., & Allen, L. A. (2015). Hospital readmission reduction program. Circulation, 131(20), 1796-1803. https://doi.org/10.1161/CIRCULATIONAHA.114.010270
Newcomb, A.B., Liu, C., Trickey, A.W., Lita, E., & Dort, J. (2018). Patient perspectives of surgical residents' communication: Do skills improve over time with a communication curriculum. Journal of Surgical Education 00(00), 1-8. https://doi.org/10.1016/j.jsurg.2018.06.015
Ore, S., Rosvold, E. O., & Helleso, R. (2019). Lessons learned from introducing huddle boards to involve nursing staff in targeted observation and reporting of medication effects in a nursing home. Journal of Multidisciplinary Healthcare, 12, 43-50. https://doi.org/10.2147/JMDH.S182872
Ospina, N.S., Phillips, K.A., Rodriguez-Gutierrez, R., Castaneda-Guarderas, A., Giofriddo, M.R., Branda, M.E. & Montori, V. M. (2018). Eliciting the patient's agenda – secondary analysis of recorded clinical encounters. Journal of General Internal Medicine. https://doi.org/10.1007/sl1606-018-4540-5
Persky, S. (2011). Employing immersive virtual environments for innovative experiments in health care communications. Patient Education and Counseling, 18(3), 313-317. https://doi.org/10.1016/j.pec.2010.12.007
Press Ganey. (2010). Inpatient survey psychometrics report. Retrieved from https://cdn.mdedge.com/files/s3fs-public/journals/supporting/jhm2297-sup-0003-suppinfo.pdf
Press Ganey. (2017). Press Ganey improvement portal user guide. Retrieved from https://helpandtraining.pressganey.com/lib-docs/default-source/ip-training-resources/ImprovementPortal_UserGuide.pdf?sfvrsn=8
Romano, C.C. (2024). Safety Huddles revisited: Lessons learned during a pandemic. Nurse Leader 22(1), 104-106. https://doi.org/10.1016/j.mnl.2023.11.004
Scoville, R., Little, K., Rakover, J., Luther, K. & Make, K. (2016). Sustaining improvement: IHI whitepaper. Cambridge, Ma: Institute for Healthcare Improvement.
Shahid, S. & Thomas, S. (2018). The situation, background, assessment, recommendation (SBAR) communication tool for handoff in healthcare- A narrative review. Safety in Health 4(7). https://doi.org/10.1186/s40886-018-0073-1
Sherman, R.O. (2017). Building trust in your leadership. American Nurse Today 12(6), 24-26.
Shryock, T. (2019). Does value-based pay have a future? Medical Economics, 96(18). Retrieved from https://www.medicaleconomics.com/news/does-value-based-pay-have-future
The Joint Commission. (2016). Summary data of sentinel events reviewed by The Joint Commission. Retrieved from https://www.jointcommission.org/resources/patientsafety-topics/sentinel-event/sentinel-event-data-summary/
Watson, J. (2008). Nursing: The philosophy and science of caring. Boulder, CO: University Press of Colorado.
Wen, J. & Schulman, K.A. (2014). Can team-based care improve patient satisfaction? A systematic review of randomized controlled trials. PLOS One 9(7), 1-9. https://doi.org/10.1371/journal.pone.0100603
Westbrook, K.W., Babkus, E., & Grant, C.C. (2014). Measuring patient-perceived hospital services quality: Validity and managerial usefulness of HCAHPS scales. Health Marketing Quarterly 31(2), 97-114. https://doi.org/10.1080/07359683.2014.907114
Will, K. K., Johnson, M. L., & Lamb, G. (2019). Team-Based care and patient satisfaction in the hospital setting: A systematic review. Journal of patient-centered research and reviews, 6(2), 158–171. https://doi.org/10.17294/2330-0698.1695


