Thrust forward by the COVID-19 crisis, with accompanying consumer and legislative pressure, telehealth has now become part of the standard of care. Telehealth and an adjunct tool, Remote Patient Monitoring, use the latest technological advancements to improve both access to and the quality of care. When used together, a powerful venue for a data-rich patient-provider encounter transpires. The method for this state of the science article included review of recent academic and gray literature to identify the breadth and depth of nurse-led innovations using these tools. Results of this rapid review of literature indicate that innovations reported in the gray literature surpass those in the academic literature in both volume and scope. Each article discussed is illustrative of the Nursing Now Challenge Global Solution Initiative (NNCGSI) which is designed to facilitate nurse-led large-scale change. The discussion asserts that nursing innovations in telehealth and RPM are understudied in the peer-reviewed literature. In conclusion, findings of this rapid review suggest that the state of the telehealth and RPM scientific literature is in its infancy.
Key Words: Telehealth, remote patient monitoring, artificial intelligence, gray literature, data analytics, informatics, nursing practice, Nursing Now
The use of telehealth and its popular companion tool, remote-patient monitoring (RPM), have been on the rise for a decade...The use of telehealth and its popular companion tool, remote-patient monitoring (RPM), has been on the rise for a decade (Lurie & Carr, 2018) and have surged significantly during the COVID-19 crisis. Conceived in an attempt to extend the reach of providers and improve continuity of care, telehealth has come into de facto use during COVID-19. It is defined by the California Department of Health Care Services (DHCS) as a
…mode of delivering health care services and public health via information and communication technologies to facilitate the diagnosis, consultation, treatment, education, care management, and self-management of a patient’s health while the patient is at the originating site and the provider is at the distant site” (DHCS, 2022, para. 2).
Telehealth has been redefined as part of routine care, not a novelty or a matter of convenience (Halamka & Cerrato, 2020). Yet, its use is without formalized best practices, especially when nursing interventions are considered.
The Nursing Now Challenge Global Solutions Initiative (NNCGSI) aimed to facilitate opportunities for nurses and midwives to advance novel nurse-led solutions to common global health challenges...For purposes of this review, RPM is defined as patient data collection and transmission outside of the customary environment of care, usually asynchronously and through technology as practices that aid clinical decision-making and care management (AMA, 2021). This state-of-the-science article will assist readers to understand a) the breadth and scope of nurse-led innovative telehealth and RPM projects and b) the best practices evolving from them. The Nursing Now Challenge Global Solutions Initiative (NNCGSI) aimed to facilitate opportunities for nurses and midwives to advance novel nurse-led solutions to common global health challenges (Nursing Now Challenge, 2021a). Each article chosen for review is consistent with the Nursing Now initiative commitment to advance the digital global health agenda (Nursing Now Challenge, 2021b).
The use of telehealth and adjunct tools such as RPM has exhibited a steep rise due to a variety of factors such as pressure from consumers and legislators as well as the COVID-19 crisis. The incentive for many healthcare stakeholders (e.g., providers, patients, payors) to move toward remote models of care is quite strong from resource consumption, infectious disease, and safety points of view (Mobbs et al., 2020). Prior to this predicament, relatively little evidence on either use or effectiveness of these modalities existed; only now are some trends emerging. According to Bestsennyy et al. (2022), telehealth is now used nearly forty times more often when compared to a comparable period in 2019. As this technology evolves, its promise is found in the large quantity of data flowing, a multitude encompassed in the term “Big Data.” These data, when fully deployed, will lead to highly-individualized care based on one person’s unique data (Brem et al., 2020). The COVID-19 pandemic has significantly accelerated the use of telehealth and thus is one factor in the state of the science; however, this review considered articles published both before and after this eventful period.
As this technology evolves, its promise is found in the large quantity of data flowing...As with most emergent care processes, exploring the scientific literature to describe practices is an important first step. Gray literature, which is professional literature that has not gone through a peer review process, is also included for a more balanced view of evidence (Paez, 2017). Much of the literature on telehealth and RPM has only relatively recently entered nursing and healthcare. A traditional literature review, coupled with a thoughtful examination of selected gray literature, will allow the entire horizon of the selected innovations to be seen, such as the scope of projects; sources of funding; and potential roles for nurses (e.g., data collectors, data scientists, subject matter experts, design thinkers). The review was conducted using the following research question: What is the state of the science in telehealth and RPM in the context of nursing innovations?
Method
A rapid review of the telehealth and RPM literature (Cumulative Index of Nursing and Allied Health Literature [CINAHL], PubMed, ABI Inform, ProQuest & selected gray literature) was conducted for the years 2017-2021 in order to describe evolving practices in this rapidly growing digital care space. A rapid review is defined as, “a form of knowledge synthesis in which components of the systematic review process are simplified or omitted to produce information in a timely manner” (Tricco et al., 2015, p.2). This type of review is useful when a traditional review (e.g., a systematic or meta analysis review) would deprive the audience of timely and relevant research to be quickly applied to practice (Haby et al., 2016). A rapid review, then, is especially appropriate in light of how the COVID crisis triggered a huge increase in demand for wearables of all kinds, including smart watches, smart bands, and finger rings (Umair et al., 2021).
Articles were screened for description of nursing innovations in telehealth that involved RPM...The rapid search strategy and screening steps used to produce this non-exhaustive rapid review mirrors that of Douthit et al. (2022) and are elaborated below. Search terms for each data base were formed after consultation with a biomedical library science specialist and a nurse informaticist (see Table 1). The gray literature from the following societies and/or websites was purposively hand-searched for specific nurse-driven innovations: Health Information Management Systems Society (HIMSS); the American Nurses Association (ANA); Johnson & Johnson; Society of Nurse Scientists, Innovators, Entrepreneurs and Leaders (SONSIEL); and the American Organization of Nurse Leaders (AONL). A title/abstract review of the scientific and literature was then performed using the Zotero web application. Articles were screened for description of nursing innovations in telehealth that involved RPM and were produced from 2017-2021. Then, the investigator reviewed full-text articles for relevance of each scientific contribution; the results of this review are summarized below.
Table 1. Main Search Strategy, Telehealth & Remote Patient Monitoring Innovations, 2017-present
|
Source |
Location |
|
CINAHL |
https://www.ebsco.com/products/research-databases/cinahl-complete |
|
(home OR remote) AND (monitor* OR telehealth) AND (innovat*) |
|
|
Pub Med/Medline |
|
|
(home OR remote) AND (monitor* OR telehealth) AND nurs* AND (innovat*) |
|
|
ABI Inform |
|
|
(home OR remote) AND (monitor* OR telehealth) AND nurs* AND (APP OR innovat* OR award* OR compet*) |
|
|
ProQuest Dissertations & Theses Global: Humanities and Social Sciences Collection |
https://search-proquest-com.libproxy.lib.csusb.edu/pqdthss/productfulldescdetail?accountid=10359 |
|
(home OR remote) AND (monitor* OR telehealth) AND nurs* AND innovat* |
|
The search was delimited to English-language publications, those involving human subjects, and those for which a full-text article or complete report was available. Exclusion criteria included: non-English language reports, projects partially reported, and articles or reports not contained in either a peer-reviewed source or a vetted competition (e.g., Johnson & Johnson Quick Fire Challenge). Lastly, the Joanna Briggs Institute (JBI) Critical Appraisal Tools (2017) were used to appraise the quality (i.e., low, moderate, high) of each article from the traditional literature. This set of formal appraisal criteria, found at https://jbi.global/critical-appraisal-tools, was used because JBI is the recognized global leader in assessing the credibility and trustworthiness of the evidence-basis for healthcare.
Search Strategy Results
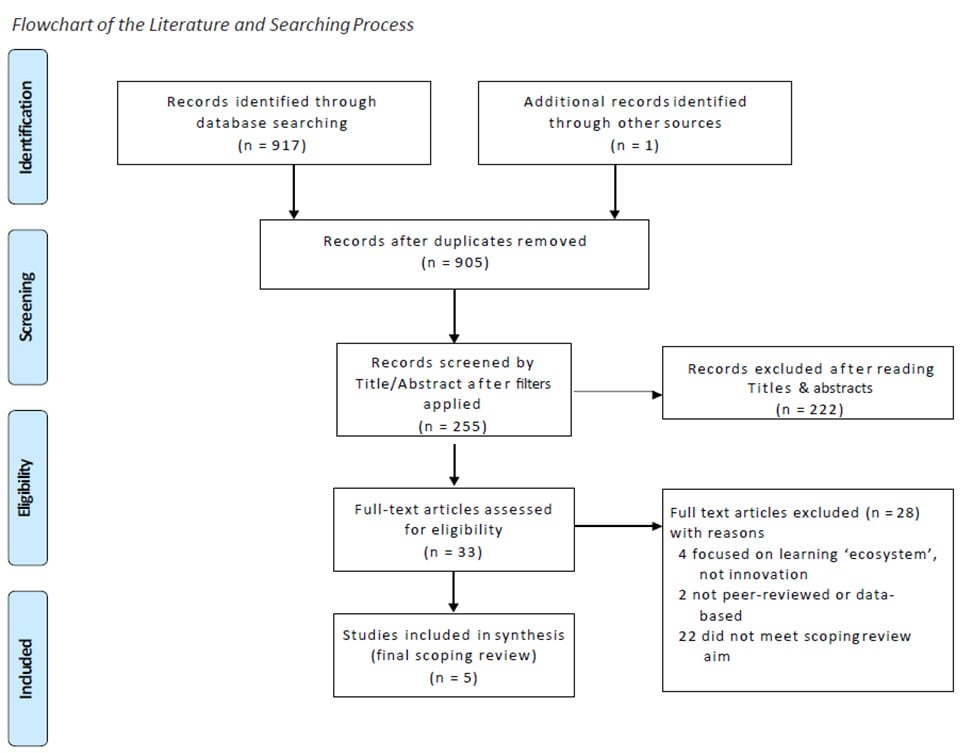
Upon completion of the search of scientific literature, 917 citations were retrieved from the combined inquiries of CINAHL, PubMed, ABI Inform and ProQuest Dissertations and Theses: Humanities and Social Sciences. One more article was identified incidentally for a total of 918. After 13 duplicates were merged and filters for English language, human subjects and research articles were applied, 255 citations remained. A title/abstract screen was performed to select the final 33 relevant articles for full review to partition the digital nurse innovations that involved both telehealth and RPM. After full review of these 33 peer-reviewed articles, five scientific articles remained for final inclusion in this rapid review, as shown in the PRISMA diagram (see Figure 1).
Figure. Search Strategy

Data extraction, reported in Table 2, lists these descriptors for each study: a description of the innovation, study design, conceptual model, sample, sampling strategy, setting, data analysis or analytics techniques, concept deployed, quality of the research and the role of the nurse-author(s).
Table 2. Descriptors of Reported Innovation Studies, Scholarly Literature
|
Authors / Year |
Design or Level of Evidence |
Model |
Sample |
Sampling Strategy |
Setting |
Analytics or Analysis |
Concepts |
Quality |
Role of Nurse |
|
Butler-Tobah et al., 2019 |
Randomized Controlled Trial |
None |
267 obstetric patients |
Convenience, randomized into treatment & control |
One OB center of an academic medical center |
Multivariate statistics |
Quality |
High |
Data Collector, Triage Nurse, Co-author |
|
Guzman-Clark et al., 2020 |
Retrospective Cohort |
Anderson Behavioral Model |
3,349 patient records |
Convenience |
VA Home Telehealth Program |
Multivariate statistics |
Adherence |
High |
Telehealth Nurse, Lead Scientist, Co-authors |
|
Guzman-Clark et al., 2021 |
Retrospective Cohort |
Anderson Model of Environment |
3449 patient records |
Convenience |
VA Home Health National Program |
Regression |
Attrition |
High |
Coordina-tor, Lead Scientist |
|
Greenhalgh et al., 2018 |
Case Studies |
NASSS Framework |
4 clinical services in the NHS |
Convenience |
National Health Service |
Action Research |
Complexity |
Low |
Unstated |
|
Sittamagari et al., 2020 |
Prospective Case Series, Descriptive |
None |
1 hospital academic learning system |
N/A |
Large integrated Investor-Owned academic learning health system across 4 states |
Descriptive Statistics |
Design Process, Safety |
High |
Telemoni-tor for triage, Symptom Manager |
[View PDF]
For the gray literature, each site was searched for “telehealth remote patient monitoring.” This mechanical search yielded hundreds of results at four of the five sites and dozens at the remaining site (SONSIEL). Additionally, a close examination of select columns or functions in each site, for example, “Health and Wellness” and “Innovation” for the Johnson & Johnson site, was conducted using a title/abstract approach. No article or content fitting the criteria for this rapid review was found; however, many items offered a context for this study.
Review of Search Results
Study Selection and Review, Scientific Literature
A single reviewer performed each step in the process illustrated in Figure 1. For the full-text review, the record was reviewed in its entirety for relevance to the definitions of this rapid review. Articles were eliminated if they reported use of telehealth without RPM or the converse. Each of the five articles remaining for full review is summarized below with uniform descriptors of each in Table 2.
Article 1. The first article reviewed described an attempt to compare traditional obstetric care to an alternative bundled-care triad of virtual (phone and online) visits, RPM, and an online community (OB Nest). Butler-Tobah et al. (2019) conducted a randomized controlled trial in a single obstetric center of the Mayo Clinic that served over 2,400 pregnancies during 2014-2015. A registered nurse (RN) served as data collector, data manager, online discussion facilitator, triage nurse, and/or co-author. As anticipated, the OB Nest group experienced significantly fewer antenatal visits, yet had significantly longer encounters when those visits occurred. The arm of the sample (n = 134) who received usual care (UC) experienced significantly higher stress and lower self-reported satisfaction scores for the care experience when compared to their OB Nest counterparts (n = 133, p < 0.001). Quality of care, including communication and decision-making, was not significantly different upon comparison of both arms of the sample (p = 0.69, p = 0.12, respectively).
...the OB Nest group experienced significantly fewer antenatal visits, yet had significantly longer encounters when those visits occurred.This study (Butler-Tobah et al., 2019) added to the relatively few randomized controlled trials that incorporate both telehealth visits and RPM as well as an online community experience as an intervention purportedly related to satisfaction, stress, or quality of care. The authors reported no difference in care quality between the two arms of the study. They recommended future testing of each component of the OB Nest bundle because this study only compared the bundled whole to UC. This study was assigned a high rating using the JBI Critical Appraisal Tool for systematic reviews.
Article 2. The second study (Guzman-Clark et al., 2020) was a retrospective program evaluation designed to gauge adherence to a Home Telehealth (HT) program within the Department of Veteran’s Affairs (VA). Program adherence was measured at one-, three-, six- and 12-months post-enrollment in the system-wide follow-up program for those diagnosed with heart failure. General estimating equations, with facility as a covariate, were used to isolate determinants of success (adherence) in a sample of 3,449 mostly white, male, older subjects. Using the Andersen Behavioral Model, a framework studying relationships between person, environment, and health behaviors, the variable of most interest was daily HT technology use. This technology that involved web browsers, interactive voice response, and in-home messaging devices (with and without peripherals for RPM) deployed disease management protocols, educational information and disease management tips via interaction with providers. During a study period in 2014 (January through June), this program continuance variable was operationally reported as Weekly Percent Adherence (i.e., number of days/week the individual patient logged in for use of the system).
...the variable of most interest was daily HT technology use.Variables significantly associated with higher weekly adherence were lower percent service connection, higher ejection fraction, no prior hospitalizations, and previous sustained use of the patient portal, My HealtheVet (all at p < 0.5 level). This is the first national study within the veteran population aimed at discovering covariates of adherence to the use of HT technology for heart failure management and monitoring. A major recommendation was to target subgroups such as those with depression, those of younger age, and those who are non-white, to determine if there is improved adherence. The study was assigned a high rating with use of the JBI Critical Appraisal Tool.
Article 3. The third article reviewed was a study designed to predict harbingers of home telehealth discontinuance and determine time to discontinuance in a sample of veterans with heart failure. Guzman-Clark and colleagues (2021) reported that older and sicker patients had a higher risk of cessation. This was the first national study of its kind; it was preceded by a similar study that sampled a medically heterogeneous population with respect to only one activity, polypharmacy use, and in only one facility. The VA Home Telehealth Program, underway since the early 2000s, uses disease management protocols for specific diseases (e.g., heart failure, chronic obstructive lung disease, diabetes).
The authors attributed the cessation or diminution of use of this technological vehicle to complexity...This program includes daily questions and education via telehealth technology, remote monitoring of health status and vital signs; these, in turn, drive care coordination and interventions. High health service use patients (e.g., frequent Emergency Department visitors) are targeted for this program which is equipped with secure hardware and software in the patients’ homes that guide them through daily reports of symptoms, remote monitoring of vital signs, in-home secure messaging and triage by a Care Coordinator or RN. Significant associated variables for the outcome of interest, attrition from the program, were advanced age, Caucasian race, and sicker patients with higher probability of readmission (p < 0.05). The study was assigned a high rating with use of the JBI Critical Appraisal Tool.
Article 4. The fourth article described an attempt to dissect factors associated with successes and failures of technology-supported programs (Greenhalgh et al., 2018). These investigators conducted a synthesis of the literature while simultaneously testing theories identified on a sample of six case studies. This partial report of their larger action research study of four clinical services (including a nurse-led heart failure service) indicated that there was strong support from clinicians and senior management for synchronous video consultation (a form of virtual-space-based strategy), but implementing such a program was logistically challenging, labor-intensive, and slow. At the end of the study period, use of video consultation for the antenatal diabetes service was discontinued and the same venue for the community heart failure service was paused. The authors attributed the cessation or diminution of use of this technological vehicle to complexity, especially as the study RNs reported profound fatigue for the heart failure group and a consequent decline in cognitive ability and/or mental health. This study, assigned a low rating using the JBI Critical Appraisal Tool, appears to be a collection of six separate case reports as opposed to a case series, per se.
...the Virtual Hospital provided care to approximately 2/3 of the system’s COVID-positive population of 2,229 patients during the study period.Article 5. The remaining article (Sitammagari et al., 2020) describes response of one large organization to the rapid advancement of COVID-19 in March of 2020. The Atrium Health created a Virtual Hospital, the Atrium Health hospital at home (AH-HaH) that paralleled, in every way, the traditional brick and mortar hospital. Staffed by physicians, advanced practice nurses and others, the Virtual Hospital provided care to approximately 2/3 of the system’s COVID-positive population of 2,229 patients during the study period of March 23, 2020 to May 7, 2020. A rapid-response team of representatives of every type of provider and other professional or technical support or administrative staff persons united to design digital eligibility assessments; patient-and provider-facing information systems; health information technology integration; and workflows that mirrored that of traditional inpatient care (Sittammagari et al., 2020).
...the virtual hospital program, launched in only two weeks, successfully and safely kept most patients in their home...Funded completely by the Atrium Health system, the Virtual Hospital consisted of a “first floor” for the (lower level) Virtual Observation Unit (VOU) and the “second floor” for the Virtual Acute-Care-Unit (VACU). Screening processes, staff structure, hospital-at-home interventions and aspects of the proactive telemonitoring software (GetWellNetwork, Inc.) communicating with “virtual providers” are discussed in this descriptive study (Sitammagari et al., 2020). The only hard measures reported were descriptive statistics for the 1,293 VOU patients and the 183 VACU patients, illness progression (i.e., transfer, admission to traditional hospital, death), and length of stay by unit. Nonetheless, an important finding remains: the virtual hospital program, launched in only two weeks, successfully and safely kept most patients in their homes, with only 3% of VOU patients and 13% of VACU patients requiring traditional hospitalization. The Atrium Health achievement is memorable in that it built a scalable platform for the electronic health record (EHR) that mandated a data-informed patient eligibility milestone in mere weeks. This study, assigned a high rating using the JBI Critical Appraisal Tool, could represent one of the best-ever design thinking projects in recent healthcare history.
...each of these five studies constituted original research and used a variety of forms of telehealth...In sum, each of these five studies constituted original research and used a variety of forms of telehealth, including two-way audiovisual communication and at least some aspect(s) of RPM. Except for the study by the Butler-Tobah group (2019), which involved obstetric patients, all others reported on an exclusively adult or primarily adult population yet shared no other structural commonalities. As each of the studies represents research in its earliest stage (e.g., descriptive or case analysis), no mention of best practices appeared.
Article/Content Selection and Review, Society/Gray Literature
Website content, meeting proceedings, and innovation pages for each of the following nursing and healthcare societies were examined for nurse-led inventions in telehealth and RPM. These societies were selected because they each exhibit a commitment in their activities, calls for abstracts, meeting themes, or modern approaches to data-based care improvements. Each contains the language of healthcare “innovation” in their mission, vision, and values. Though no content items or full articles were retrieved that contribute to the state of the science, many items at each site contribute to a panoramic view of the state of practices related to rapidly-emerging scientific findings.
Health Information Management Systems Society and American Organization of Nurse Leaders. The HIMSS site has many governmental and quasi-governmental reports on issues such as digital workflow, interoperability, and rapid expansion of digital care or strategic planning for telehealth and RPM. The AONL site contains relevant tertiary articles (e.g., news briefs) and legislative or regulatory short pieces; it also has quality improvement articles on very recent repurposing of technology, such as telehealth within a hospital ward or intensive care unit or single-function reports like remote ventilator monitoring. Topical and educational articles abound at these and at all sites examined.
Johnson & Johnson and Society of Nurse Scientists, Innovators, Entrepreneurs and Leaders. The most promising and relevant material is found at the sites for Johnson & Johnson. Their website included projects in common with SONSIEL as well as launch projects from the ANA membership reported at their society site. Johnson & Johnson supports the work of nurses in a number of important ways, including the NursesHack4Health Hackathons and the Quick Fire Challenge Series. Each venue is designed to give voice to nurse innovations at their earliest stage of idea inception. NursesHack4Health Hackathons, a crowdsourcing opportunity to spin ideas into a viable business plan with the technological and mentoring support of SONSIEL and Microsoft, yielded such efforts as Project Flourish, a limited RPM project designed to connect minimal patient data to a provider in a rural population with little or no technologic literacy or present-day devices.
Each venue is designed to give voice to nurse innovations at their earliest stage of idea inception.The Quick Fire Challenge Series enables individual nurses and small nursing teams to move from idea generation to a testing stage with small grants for new devices, new uses for existing devices and/or treatment protocols. Projects such as the Care Station, a low-cost telehealth enabled tablet, allowed a qualified nurse to remotely screen for COVID-19 at the entrances of homeless shelters. Projects such as these, while meaningful, are not completed studies, are often in the proposal formation stage, and are usually communicated through partial results with a full article at scale or funding pending. They serve as valuable resources for ecologically-valid hypotheses or theses.
American Nurses Association. ANA offers incentives, awards, and recognitions such as the NursePitch™ Contest and the ANA Innovation Award powered by Beckton, Dickinson, and Company. The latter venue highlights, celebrates, and rewards nurse-led innovations (e.g., cash prizes, incubator opportunities) for individuals and small teams with the aim of sponsoring such ideas through translational research phases including prototyping, testing, and product implementation. A prominent award-winning product, iN, is a wall-mounted device placed directly behind the patient bed that uses computer vision to monitor prodromal activities predictive (through custom algorithms) of patient injury and aggregates data from the EHR and other devices. The Pitch Contest offers small-scale entrepreneurial projects the opportunity to be “pitched” to judges in a 5-minute rapid-fire format with competitors responding to queries on costs, uses, re-deployment potential, and target markets. Each takes place in a yearly event with the competition phase open to the entire global nursing public.
Discussion
The paucity of such studies is likely a reflection of the rapidity with which these nursing practices evolved...Overall, nursing innovations in telehealth and RPM are understudied in the peer-reviewed literature. The paucity of such studies is likely a reflection of the rapidity with which these nursing practices evolved as well as a lack of capacity in new research and analytics methodologies suitable to their exploration. As the number of vetted standards for structured information exchange in healthcare grows and guidelines for proper use of available Big Data are translated to practice (Weigel et al., 2020), it is anticipated that many more nursing innovations will develop, as evidenced in numerous reports of start-up efforts in the gray literature.
Of the five studies reported, three used a conceptual framework (Guzman-Clark et al., 2020; Guzman-Clark et al., 2021; Greenhalgh et al, 2018) and only one (Butler-Tobah et al., 2019) used primary patient data. The remaining studies used secondary data from individual patient records or a hospital system/subsystem. All research reports used traditional biomedical statistics for analysis and not a more sophisticated means of pattern identification or other analytics available through artificial intelligence/machine learning (AI/ML). All but one study (Greenhalgh et al., 2018) reported the contribution of the nurse in a coordinating role; two studies (Guzman-Clark et al., 2020; Guzman-Clark et al., 2021) reported that a professional nurse led the study.
One promising change on the horizon includes development of Nursing Innovation Centers.The descriptive nature of the most promising current research leads naturally to a need for replication in different populations, health systems, and countries. Outcomes explored in the select studies included: adherence, attrition, satisfaction, program discontinuance, and appropriateness of virtual hospital care. As awareness and acceptance of telehealth and RPM evolves (Weigel et al., 2020) and, hopefully, data science becomes increasingly utilized within our ranks (Schultz et al., 2021), the large data sets now available will be more fully deployed using AI/ML to explore phenomena of interest to nursing and beyond. One promising change on the horizon includes development of Nursing Innovation Centers (Albert, 2018). Dedicated to invention and improvement within the healthcare environment, some see the novel practices and infrastructures in these environments as more conducive to testing and diffusion of innovation in practice and research than in traditional research settings, such as academic medical centers.
Each of the well-known organizations and sites provides inspiration for researchers to invent new practices or improve existing ones, most notably patient monitoring. Technology improves patient surveillance or monitoring, a long-term function of the nurse advocate, by extending nurses’ reach to check physiologic and environmental factors. Additional time points for data establish trends (e.g., blood sugar or blood pressure readings) which are transmitted in real time and conjoin in exceptionally large data bases from which clinicians and researchers can predict an emergent clinical condition or the need for an urgent treatment change.
Only recently has nursing research begun to move toward the advanced analytics necessary to identify and organize data patterns in these vast data sets...Only recently has nursing research begun to move toward the advanced analytics necessary to identify and organize data patterns in these vast data sets to improve care. These technological advances coincide with biologic discoveries in genomics and the environment that have resulted in exponential change in possibilities for care improvement through data science. The steep rise in the use of data science methods for actual predictive capabilities within these large data sets has accelerated the innovations reported by major provider websites. This is in stark contrast to the academic literature, which relies on traditional scientific methods and biostatistics to explore phenomena of interest to nursing and healthcare at a much slower rate and limited scope.
Conclusion
Findings of this rapid review suggest that the state of the telehealth and RPM scientific literature is in its infancy. Big Data use is new to healthcare, so actionable insights from such data mining are only evolving now. Few nurses have trained as Data Scientists so most do not possess the expertise in data analytics necessary to wrestle with the plethora of data yielded. This gap in applied statistic and methodologies versus advanced analytic training presents barriers to the full realization of a rapidly growing body of practice and opportunities in telehealth and RPM. Recommendations are twofold: more nurses must be prepared as Data Scientists and existing nurse researchers must add to their repertoire through interprofessional work with methodologists and scientists prepared in AI/ML.
Findings of this rapid review suggest that the state of the telehealth and RPM scientific literature is in its infancy.As healthcare organizations worldwide begin to examine their Analytics Maturity to derive the maximum utility from this data tsunami (Carvalho et al., 2019), it could be that these types of studies will soon join the already exponential exploration of healthcare data through AI/ML published in journals of computer science and medicine. The gray literature portends the permanence of telehealth and RPM in the global healthcare landscape, thus identifying new fertile ground for nursing research in this space. The Nursing Now Challenge espouses a commitment to person-centered care (Nursing Now, 2021b) making it poised to continue its considerable influence on nurse-led innovative care based on individual patient and/or consumer health data.
Acknowledgement: I have no known conflict of interest to disclose.
Author
Mary Anne Schultz, PhD, MBA, MSN, RN, FAAN
Email: Masupland@gmail.com
ORCID ID: https://orcid.org/0000-0002-8874-6610
Mary Anne Schultz is Professor and Informaticist in the Department of Nursing at the California State University, San Bernardino. She is a former Department Chair and Associate Dean who is now a Consultant specializing in Precision Health. She holds a gubernatorial appointment (California, Newsom) to the state’s Advisory to Advance Precision Medicine and she chairs a workgroup of a CMS-sponsored committee on Post-Acute Care Interoperability (PACIO) under the CARIN Initiative. She holds numerous awards for scholarship and writing in data science and informatics. Correspondence concerning this article can be sent via email or mailed to Dr. Mary Anne Schultz, Department of Nursing, California State University, San Bernardino, CA 92407.
References
Albert, N. M. (2018). Operationalizing a nursing innovation center within a health care system. Nursing Administration Quarterly, 42(1), 43-53. https://doi.org/10.1097/NAQ.0000000000000266
American Medical Association. (2021). Defining the telehealth landscape. Telehealth resource center. https://www.ama-assn.org/practice-management/digital/telehealth-resource-center-definitions
Bestsennyy, O., Gilvert, G., Harris, A., & Rost, J. (2021, July 9). Telehealth: A quarter trillion dollar post-COVID-19 reality? McKinsey & Company. https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality
Brem, A., Viardot, E., & Nylund, P. A. (2021). Implications of the coronavirus (COVID-19) outbreak for innovation: Which technologies will improve our lives? Technological Forecasting and Social Change, 163. https://doi.org/10.1016/j.techfore.2020.120451
Butler-Tobah, Y. S., LeBlanc, A., Branda, M. E., Inselman, J. W., Morris, M. A., Ridgeway, J. L., Finnie, D. M., Theiler, R., Torbenson, V. E., Brodrick, E. M., Meylor de Mooij, M., Gostout, B., & Famuyide, A. (2019). Randomized comparison of a reduced-visit prenatal care model enhanced with remote monitoring. American Journal of Obstetrics and Gynecology, 221(6), 638.e1-638.e8. https://doi.org/10.1016/j.ajog.2019.06.034
Carvalho, J. V., Rocha, A., Vasconcelos, J., & Abreu, A. (2019). A health data analytics maturity model for hospital information systems. International Journal of Information Management, 46, 278-285. https://doi.org/10.1016/j.ijinfomgt.2018.07.001
Department of Health Care Services. (2021). Telehealth frequently asked questions. https://www.dhcs.ca.gov/provgovpart/Pages/TelehealthFAQ.aspx
Douthit, B., J., Walden, R. L., Cato, K., Coviak, C. P., Cruz, C., D’Agostino, F., Forbes, T., Gao, G., Kapetanovic, T. A., Lee, M., A., Pruinelli, L., Schultz, M. A., Wieben, A., & Jeffery, A. D. (2022). Data Science Trends relevant to nursing practice: A rapid review of the literature. Applied Clinical Informatics Journal, 13(01), 161-179. https://doi.org/10.1055/s-0041-1742218
Greenhalgh, T., Wherton, J., Papoutsi, C., Lynch, J., Hughes, G., A'Court, C., Hinder, S., Proctor, R., & Shaw, S. (2018). Analyzing the role of complexity in explaining the fortunes of technology programmes: Empirical application of the NASSS Framework. BMC Medicine, 16(66), 1-15. https://doi.org/10.1186/s12916-018-1050-6
Guzman-Clark, J. G., Yefimova, M., Farmer, M. M., Wakefield, B. J., Viernes, B., Lee, M. L., & Hahn, T. J. (2020). Home telehealth technologies for heart failure: An examination of adherence among Veterans. Journal of Gerontological Nursing, 46(7). 26-34. https://doi.org/10.3928/00989134-20200605-05
Guzman-Clark, J., Farmer, M. M., Wakefield, B. J., Viernes, B., Yefimova, M., Lee, M. L., & Hahn, T. J. (2021). Why patients stop using their home telehealth technologies over time: Predictors of discontinuation in Veterans with heart failure. Nursing Outlook, 69(2), 159–166, https://doi.org/10.1016/j.outlook.2020.11.004
Haby, M. M., Chapman, E., Clark, R., Barreto, J., Reveiz, L. & Lavis, J. N. (2016). What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: A rapid review. Health Research Policy and Systems, 14(1), 83–83. https://doi.org/10.1186/s12961-016-0155-7
Halamka, J., & Cerrato, P. (2020). The digital reconstruction of health care. NEJM Catalyst Innovations in Care Delivery, 1(6). https://doi.org/10.1056/CAT.20.0082
Joanna Briggs Institute (2017). Critical Appraisal Tools. https://jbi.global/critical-appraisal-tools
Lurie, N., & Carr, B. G. (2018). The use of telehealth in the medical response to disaster. JAMA Intern Medicine, 178(6), 745-746. https://doi.org/10.1001/jamainternmed.2018.1314
Mobbs, R. J., Ho, D., Choy, W. J., Betteridge, C., & Lin, H. (2020). COVID-19 is shifting the adoption of wearable monitoring and telemedicine (WearTel) in the delivery of healthcare: Opinion piece. Annals of Translational Medicine, 8(20). https://doi.org/10.21037/atm-20-3678
Nursing Now Challenge (2021a). New NNCGSI challenges coming soon. https://www.nursingnow.org/news/new-nncgsi-challenges-coming-soon
Nursing Now Challenge (2021b). WISH sponsors Nursing Now Challenge. https://www.nursingnow.org/news/wish-sponsors-nursing-now-challenge-global-solutions-initiatives-on-climate-change-and-digital-health
Paez, A. (2017). Gray literature: An important resource in systematic reviews. Journal of Evidence-Based Medicine, 10(3), 233-240. https://doi.org/10.1111/jebm.12265
Schultz, M. A., Walden, R. L., Cato, K., Coviak, C., Cruz, C., D’Agostino, F., Douthit, B. J., Forbes, T., Gao, G., Lee, M., Lekan, D., Weiban, A., & Jeffery, A. D. (2021). Data Science methods for Nursing-relevant patient outcomes and clinical processes: The 2019 literature year-in-review. CIN: Computers, Informatics, Nursing, 39(11), 654-667. https://doi.org/10.1097/CIN.0000000000000705
Sitammagari, K., Murphy, S., Kowalkowki, M., Chou, S-H., Sullivan, M., Taylor, S., Kearns, J., Batchelor, T., Rivet, C., Hole, C., Hinson, T., McCreary, P., Brown, R., Dunn, T., Neuwirth, Z., & McWilliams, A. (2020). Insights from rapid deployment of a “Virtual Hospital” as standard care during the COVID-19 pandemic. Annals of Internal Medicine, 174(2), 192-199. https://doi.org/10.7326/M20-4076
Tricco, A. C., Antony, J., Zarin, W., Strifler, L., Ghassemi, M., Ivory, J., Perrier, L., Hutton, B., Moher, D., & Straus, S. E. (2015). A scoping review of rapid review methods. BMC Medicine, 13(224), 1-15. https://doi.org/10.1186/s12916-015-0465-6
Umair, M., Cheema, M. A., Cheema, O., Li, H., & Lu, H. (2021). Impact of COVID-19 on IoT adoption in healthcare, smart homes, smart buildings, smart cities, transportation and industrial IoT. Sensors, 21(11), 3838. https://doi.org/10.3390/s21113838
Weigel, G., Ramaswamy, A., Sobel, L., Saiganicoff, A., Cubanski, J., & Freed, M. (2020, May 11). Opportunities and barriers for telemedicine in the U. S. during the COVID-19 emergency and beyond. KFF Women’s Health Policy. https://www.kff.org/womens-health-policy/issue-brief/opportunities-and-barriers-for-telemedicine-in-the-u-s-during-the-covid-19-emergency-and-beyond


