Discriminative nursing care (DNC) is the act of a nurse treating a patient differently from another patient based on the patient’s illness, diagnosis, lifestyle, personal choices, age, or socio-demographic status. As such, the patient perceives a variation in treatment. Health-related stigma and stereotyping contribute to DNC, especially towards patients with opioid use disorder (OUD) during hospitalization. This integrative review considered recent relevant literature related to DNC practices towards patients with OUD in the hospital setting to identify discriminatory actions and potential causes and to provide known and new recommendations to address DNC practices towards this patient population. Literature from 2016-2022 (n = 13) was searched and analyzed, revealing four emerging themes: Patients’ Perceptions of DNC, Nurses and Other Healthcare Providers’ Perceptions of DNC, Nurses’ Lack of Understanding, and Recommendations for Improvement. In this article, we discuss specific findings related to each theme, gaps in the current literature, additional recommendations, and important considerations for future research.
Key Words: Discriminative nursing care, discrimination, stigma, health-related stigma, stereotype, opioid, opioid use disorder, OUD, substance use disorder, SUD, abuse, addiction, dependence, recovery
A basic tenet of healthcare is that all patients deserve equal treatment regardless of health conditions or individual characteristics.A basic tenet of healthcare is that all patients deserve equal treatment regardless of health conditions or individual characteristics. Discriminative nursing care (DNC) is the antithesis of this principle. At its core, DNC is derived from the phenomenon of discrimination; in general, this means treating a person or a group of people differently from others (Merriam-Webster, 2021). In nursing, discrimination is the act of a nurse treating a patient or patients differently from others based on factors (or a combination of factors) that causes them to perceive a difference in treatment. Such factors may include their diagnosis, lifestyle, personal choices, age, or socio-demographic status.
DNC is a complex concept with more than one perspective...DNC is a complex concept with more than one perspective; it includes the actual discriminatory practices by the nurse toward the patient as well as the perception of those practices by the patient. The implications of DNC in the current healthcare system are hypothetically extensive due to the vast number of people potentially affected. Total hospital admissions in the United States (U.S.), excluding intensive care unit (ICU) admissions, numbered 36,241,815 in 2019 (American Hospital Association [AHA], 2021). This figure indicates that just over 10% of the population of the United States were admitted for hospital care in 2019 and likely received nursing care. Thus, conceivably, as much as 10% of the population could experience DNC during hospitalization.
Health-related stigma is a contributing factor to DNC.Health-related stigma is a contributing factor to DNC. In his groundbreaking 1963 book, Erving Goffman abstracted the concept of stigma and the ideas he presented still ring true today. Goffman (1963) explained that stigma is a personal or group attribute labeled as less worthy, less valuable, or different. The attribute is discredited when it is stigmatized, and the effects of stigma can be far-reaching and long-lasting. Health-related stigma results from labeling human differences and the degree to which a health condition is stigmatized depends on its social significance (Link & Phelan, 2006). A major element of health-related stigma is stereotyping which occurs when a person or group of people are marked with an unfavorable characteristic related to a health condition (Link & Phelan, 2006). The terms stigma and stereotype are often used interchangeably. While they can both apply to a health attribute concurrently, stigma is more precisely defined as the simultaneous occurrence of aspects such as stereotyping, discrimination, and labeling (Link & Phelan, 2001).
Opioid use disorder (OUD) is a chronic condition involving the misuse of opioids which falls under the umbrella of substance use disorder. Diagnosis of OUD is recognized by the American Psychiatric Association DSM-5 (Dydyk et al., 2022). It affects a very large number of the global population from all socioeconomic and cultural backgrounds (Centers for Disease Control and Prevention, 2022). To date, over 16 million people experience OUD internationally, including more than 2.1 million people in the United States. Additionally, over 120,000 people die from OUD each year (Dydyk et al., 2022).
Although OUD is far-reaching and affects people from all backgrounds, it remains highly stigmatized.Although OUD is far-reaching and affects people from all backgrounds, it remains highly stigmatized (Hawk et al., 2022). With OUD affecting so much of the population, many patients hospitalized for a separate illness or condition may have a comorbidity of OUD and thus could potentially experience DNC related to OUD. The purpose of this integrative review was to analyze current literature to answer the question: What discriminative nursing care practices towards patients with OUD exist in the hospital setting?
Methods
Integrative Review Framework
An integrative review is a summary of current literature published on a specific topic. Through various methodologies used to appraise available scientific data sources, the integrative review presents a thorough understanding of a concept, theme, or problem. The goal of an integrative review of a nursing topic is to enhance the general understanding of the topic in order to improve evidence-based practices. Through delivering a comprehensive summary of what is known, an integrative review becomes a building block for future research, clinical practice, and policy applications (Whittemore & Knafl, 2005). Our review incorporated aspects of Whittemore & Knafl’s (2005) methodology for conducting an integrative review and features of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 flow diagram for updated systematic reviews (Page et al., 2021).
...those experiencing OUD who are hospitalized for a separate illness may face discrimination by those providing care.Problem Identification
Tens of millions of people are hospitalized in the United States each year (AHA, 2021), and many of these patients have a comorbidity of OUD. Because OUD is a highly stigmatized illness (Hawk et al., 2022), those experiencing OUD who are hospitalized for a separate illness may face discrimination by those providing care. One aim of this integrative review was to identify what DNC practices exist toward patients with OUD in the hospital setting. Furthermore, we sought to elucidate specific causes of DNC concerning this patient population as well as to offer recommendations to address the problems.
Literature Search
We searched the literature using the Cumulative Index to Nursing and Allied Health Literature (CINAHL) database, PubMed, and Web of Science (WOS). Search terms were formulated with the assistance of University of Tennessee, Knoxville, Heath Science Librarians and included a range of related words and medical subject headings (MeSH terms). Examples of search terms used include opioid, heroin, fentanyl, oxycodone, disorder, misuse, abuse, OUD, discriminate, prejudice, bias, stigma, practice, behavior, nurse, hospital, and inpatient. The following MeSH terms were included in the PubMed database search: Social Discrimination; Stereotyping; Health Knowledge, Attitudes, Practice; Social Perception; Nurses; and Hospitals.
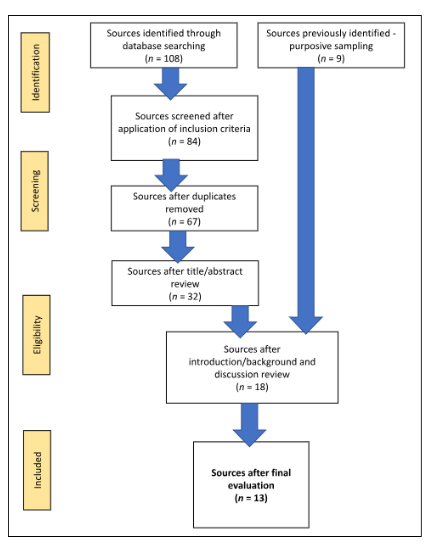
The initial database searches yielded the following number of articles: CINAHL = 24, PubMed = 57, and WOS = 27 (total n = 108). Inclusion criteria were: 1) peer-reviewed articles, 2) published between 2016-2022, 3) original research reports (i.e., primary sources), 4) written in English, and 5) associated with DNC and/or OUD in a hospital or related setting. Final selection of articles from each database totaled: CINAHL = 14 articles, PubMed = 49 articles, and WOS = 21 articles (n = 84). Literature search revealed redundancies across multiple databases (i.e., some articles were found on more than one database). Specifically, one duplicate article was found on both CINAHL and PubMed; one from both CINAHL and WOS; seven on both PubMed and WOS; and eight on all three databases (n = 17). These duplicates were removed, leaving 67 articles for data evaluation.
Data Evaluation
Whittemore & Knafl (2005) acknowledged that evaluating the quality of data for an integrative review is difficult and multifaceted. To achieve meaningful evaluation of articles produced in the initial database search, the author first reviewed the title and abstract (when available) of each article to identify key elements and excluded articles not germane to the aim of this review. This strategy eliminated 35 articles, leaving 32 articles for review. Purposive literature sampling from 2021-2022 provided nine additional articles to review, resulting in a revised article count of 41.
The next step included secondary review of article titles and abstracts along with evaluation of the introduction/background section(s) and discussion sections. This allowed for evaluation of the content of each article and facilitated the decision to include or exclude articles. Articles that were included pertained in some way to discriminatory health care treatment, nursing care, health-related stigma, and OUD or an associated substance use disorder (SUD). Of the 41 articles, nine remained from the initial database search and four from the purposive sampled articles which brought the total count to 13 (see Figure 1). Detailed information demonstrating how each article met the inclusion criteria, including key findings and theme(s) emerging from each article, was documented and is available through a supplemental link.
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Flow Diagram6
Data Analysis
Data were extracted from peer-reviewed primary sources and analysis was guided by Whittemore & Knafl’s (2005) updated methodology for conducting an integrative review. The classification system used for data reduction comprised isolating key findings from each source and grouping the findings according to emerging themes identified during evaluation.
Results
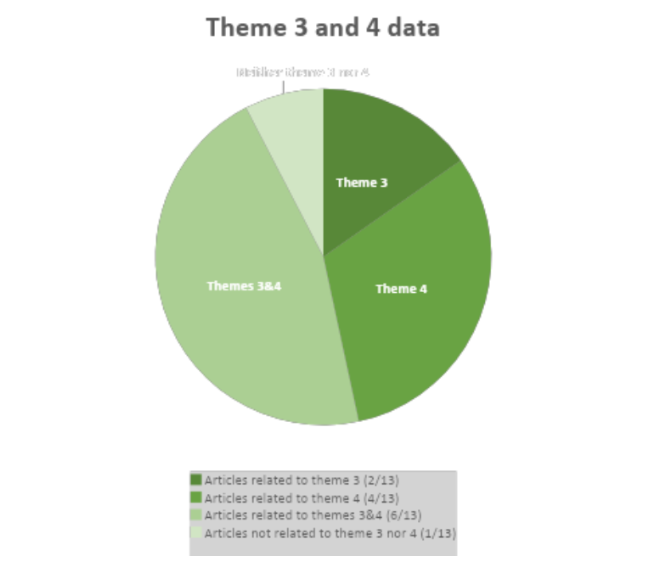
Thirteen research articles were analyzed to explore the research question, what discriminative nursing care practices towards patients with OUD exist in the hospital setting? Two primary themes emerged: Theme 1 was “Patients’ Perceptions of DNC,” and Theme 2 was “Nurses and Other Healthcare Providers’ Perceptions of DNC.” Data from each source supported either or both themes. Subsequently, two secondary, or subthemes, were developed because of supplementary data presented in most articles. Theme 3, "Nurses' Lack of Understanding," and Theme 4, "Recommendations for Improvement," were subthemes to both Themes 1 and 2. The DNC themes found in the included articles are shown in the Table.
Table. Description of Discriminative Nursing Care (DNC) Themes in Included Articles
|
Themes |
Articles n (%) |
Topic Relation to DNC |
|---|---|---|
|
1: Patients’ Perceptions of DNC |
5 (38%) |
Concepts that comprise DNC |
|
2: Nurses and Other Healthcare Providers’ Perceptions of DNC |
7 (54%) |
Concepts that comprise DNC |
|
Both 1 & 2 |
1 (8%) |
Concepts that comprise DNC |
|
3: Nurses’ Lack of Understanding |
2 (15%) |
Causes or perpetuates DNC |
|
4: Recommendations for Improvement |
4 (31%) |
Resolutions to DNC |
|
Both 3 and 4 |
6 (46%) |
Causes or perpetuates DNC or resolutions to DNC |
|
Neither 3 nor 4 |
(8%) |
-- |
Display of thematic extracted data is presented in Figures 2 and 3. Following these figures, the themes are discussed in more detail below.
Figure 2. Data Analysis – Primary Thematic Data Display
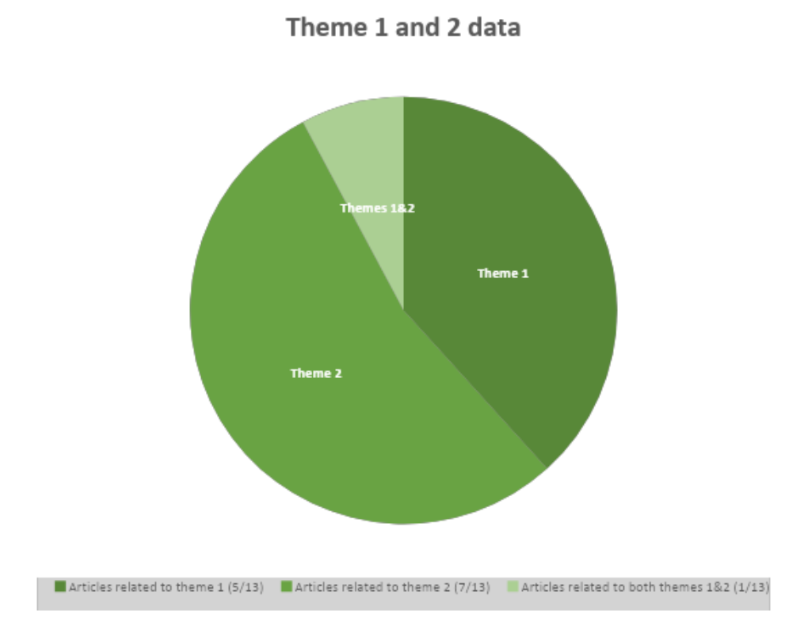
Figure 3. Data Analysis – Secondary Thematic Data Display
The discussion of the themes supports the previous assertion that DNC includes perspectives from both providers (i.e., discriminatory practices by caregivers towards patients) and recipients of care (i.e., perception of these practices). The first two themes identified pertain to the concepts that comprise DNC. Description of the third theme (Nurses’ Lack of Understanding) includes patient- and nurse-reported issues that can cause or perpetuate discriminatory care. The fourth theme describes recommendations to address DNC from the patients’ and nurses’ perspectives.
Patients described receiving generally disparate treatment as compared with patients who did not experience OUD or a related illness.Theme #1: Patients’ Perceptions of DNC
A primary theme extracted from the integrative review process was patients’ perceptions of being treated differently from other patients because they experienced OUD or a related illness, either presently or in the past. Some DNC practices reported by patients included feelings of judgement and blame (Blair et al., 2021; Simon et al., 2020); minimization of pain and medical issues (Hawk et al., 2022); and superficial treatment, ineffective communication, delays in care, and poor attitudes (Jaiteh et al., 2019). Patients described receiving generally disparate treatment as compared with patients who did not experience OUD or a related illness (Blair et al., 2021; Simon et al., 2020). Furthermore, patients expressed how healthcare professionals’ biases and attitudes can be extremely influential, either intentionally or unintentionally, and can sway the treatment choices of people with OUD (Shreffler et al., 2021).
Patients’ perceptions of DNC not only affect their hospital stay, but also influence healthcare services after hospitalization.Patients’ perceptions of DNC not only affect their hospital stay, but also influence healthcare services after hospitalization. Furthermore, DNC can negatively affect the treatment success of those working through substance withdrawal. Dineen (2021) explored the discriminative actions that people with OUD experienced during continued care after hospitalization and found that some nursing, post-acute medical, and rehabilitation facilities do not admit patients with a known OUD or other substance use disorder. Simon et al. (2020) explored the reasons people with substance use disorders, including OUD, who are experiencing withdrawal symptoms choose to leave the hospital against medical advice and found that DNC was a factor in the decision. Patients explained that their withdrawal symptoms and related issues were ignored and inadequately treated. They also reported stricter restrictions, such as lack of permission to leave the floor on which their room was located, no ability to go outside, and limits for the number of visitors allowed.
Theme #2: Nurses and Other Healthcare Providers’ Perceptions of DNC
Stigmatizing patients with a substance use disorder was reported in several research studies...The second primary theme derived from the integrative review included perceptions of DNC by nurses and other healthcare providers. These groups were combined into one theme because of their common role of caring for patients with OUD. Nurses reported placing guilt and shame on people with OUD (Reese et al., 2021) and, at times, their families (Sapp & Hooten, 2019). Medical students observed nurses and physicians stigmatizing patients with a substance use disorder during treatment (Shreffler et al., 2021). Stigmatizing patients with a substance use disorder was reported in several research studies (El Rasheed et al., 2016; Horner et al., 2019; Shreffler et al., 2021) and was found to compromise the quality of health care provided to these patients. Stigmatizing behaviors resulting in compromised care included, but are not limited to, insufficient pain control, inadequate time spent with the care provider, a delay in care provided (Horner et al., 2019), and generally inequitable care compared with those without a substance use disorder (El Rasheed et al., 2016).
Along with stigmatization, stereotyping of persons with OUD was linked to nursing care...Along with stigmatization, stereotyping of persons with OUD was linked to nursing care (Cooney & Broglio, 2017) and the reasons cited for these actions were numerous. Nurses claimed to have insufficient knowledge to identify and manage the care of patients with addiction issues, which may lead to a negative emotional response that, in turn, perpetuates stigma toward this patient population (El Rasheed et al., 2016). Nurses identified personal safety threats from patients with OUD and experienced an internal conflict when treating the pain of patients with OUD; they questioned their own role in the patient’s potential addiction-recovery cycle. Nurses also described feelings of burnout after lengthy periods of caring for patients with OUD, who they considered a more-demanding population (Horner et al., 2019).
Nurses’ motivation was found to be significantly related to their personal experiences.Another nurse perception of DNC is the relationship between motivation level and discriminatory behaviors. Mahmoud et al. (2021) explained that the motivation level of nurses to care for patients with substance use issues, including opioid use issues, can either positively or negatively impact the care received by these patients. More specifically, low motivation in nurses was linked to negative patient outcomes, such as delays in problem identification, limited healthcare access and resources, and an increased likelihood to drop out of withdrawal treatment. Nurses’ motivation was found to be significantly related to their personal experiences. If the nurse had a family member with a current or previous substance use issue, that nurse was more motivated to provide quality care to patients with substance use issues. Additional aspects of nursing related to higher motivation in caring for patients with substance use issues included past work experience in substance use treatment, receiving continuing education related to substance use, nurse role adequacy, role support, work satisfaction, and self-efficacy (Mahmoud et al., 2021).
A major cause of DNC was insufficient nursing knowledge to adequately care for patients with substance use issues.Theme #3: Nurses’ Lack of Understanding
A secondary theme describing nurses’ lack of understanding was revealed during literature appraisal, and it is related to perceptions of both nurses and patients. A major cause of DNC was insufficient nursing knowledge to adequately care for patients with substance use issues. Many nurses, even psychiatric nurses, did not feel they have sufficient knowledge to identify and manage patient care associated with addiction issues (El Rasheed et al., 2016). Uninformed and deficient preparation has been linked to emotional responses triggered in nurses caring for patients with substance issues which can lead to a higher level of stigma toward this population (El Rasheed et al., 2016). Furthermore, patients with OUD felt that staff working in emergency departments lack the knowledge required to adequately understand and treat OUD and are, consequently, ill-equipped to do so (Hawk at al., 2022). In one study by Simon et al. (2020), patients with substance use disorder experienced feelings of mistrust from healthcare staff and speculated that the poor treatment they received could have been the result of the staff not understanding substance use disorders.
Along with the educational and knowledge level of nurses, the perspectives of nurses caring for patients with substance use issues was linked to DNC. Shreffler et al. (2021) found that nurses valued the difficulty of recovering from substance use disorders less than physicians and medical students treating this population. This could result from inadequate instruction in nursing school and inadequate continuing education. Accordingly, the perspectives of nurses caring for patients with OUD may be a result of the very insufficient nursing knowledge discussed above.
Theme #4: Recommendations for Improvement
A common recommendation for improvement from patients and nurses was to increase the educational preparation and knowledge base of nurses and others...A majority of the articles reviewed included one or more recommendations for improvement, and thus this emerged as a secondary theme. A common recommendation for improvement from patients and nurses was to increase the educational preparation and knowledge base of nurses and others who care for patients with OUD (Horner et al., 2019; Reese et al., 2021). Another recommendation for improvement was increased effective communication. More specifically, effective interdisciplinary communication as well as open group communication between the patient and all members of the healthcare team were recommended because both were identified as major factors in successful treatment of people with OUD (Horner et al., 2019). Additional recommendations for improvement included refining patient transitions from the hospital to the community, standardizing care for those with OUD, and enhancing the emotional support available to patients with OUD (Horner et al., 2019). Turner et al. (2018) emphasized the importance of effective care planning, from compassionate and empathetic screening to discharge planning geared toward open communication with the outpatient provider and supplementary resource provisions.
Discussion
The major recommendation was to increase nurses’ knowledge in general about OUD...This integrative review focused on analysis of recent relevant literature related to DNC practices towards patients with OUD in the hospital setting. Our evaluation sought to identify DNC practices and the causes of DNC, and to provide known and new recommendations to combat DNC practices towards this patient population. Two main themes emerged: nurses’ lack of knowledge and understanding of OUD and the perspectives from which nurses provide care to this patient population. Several recommendations to address DNC practices towards people with OUD were expressed in the reviewed literature. The major recommendation was to increase nurses’ knowledge in general about OUD as a disease through directed education, comprehensive training, and experiential learning (Horner et al., 2019; Reese et al., 2021). Nurses need more education about OUD as a disease, the lasting consequences of OUD to those who experience it as well the impact on the community, and best practices to care for patients with OUD. Through comprehensive training and education experiences, nurses will gain a more complete understanding of OUD (Horner et al., 2019; Reese et al., 2021). Ideally, dedicated education will lessen the instances of DNC toward patients with OUD.
Providing holistic, non-judgmental, non-discriminatory care throughout the patient’s hospitalization and into the discharge process is essential...Increasing nurses’ knowledge about OUD has the potential to change the perspectives from which they care for patients with OUD. The literature revealed that nurses with experience caring for people with substance use issues (e.g., caring for a family member with OUD) were typically more motivated to provide quality care to this patient population (Mahmoud et al., 2021). The perspectives from which these nurses cared for patients with substance use issues were more positive than those of nurses without such experience. Because nurses typically spend the most time with patients during a hospitalization, their knowledge, and the attitudes and perspectives derived from this knowledge, are vital components of holistic nursing care (Shreffler et al., 2021). Providing holistic, non-judgmental, non-discriminatory care throughout the patient’s hospitalization and into the discharge process is essential to a successful treatment plan.
When patients receive disparate treatment, they are made to feel “less than” and, perhaps, less worthy of quality care.The results of this review are important to the discipline of nursing and to patient care outcomes. Nurses carry their knowledge and life experiences with them when providing care, which can lead to unintentional or intentional stigmatization towards patients with OUD. The four themes revealed during literature appraisal directly affect patient care and, therefore, patient outcomes. When patients receive disparate treatment, they are made to feel “less than” and, perhaps, less worthy of quality care. OUD is a highly stigmatized illness (Hawk et al., 2022) and patients with OUD could potentially experience DNC during hospitalization. DNC influences not only the experiences of hospitalization (Blair et al., 2021; Hawk et al., 2022; Jaiteh et al., 2019; Simon et al., 2020), but also the outcomes of hospitalization and post-discharge care (Dineen, 2021; Simon et al., 2020).
The purpose of an integrative review is to deliver a comprehensive summary of current scientific literature to spark future research and to recommend ways to improve clinical practice and policy applications (Whittemore & Knafl, 2005). After conducting the current review, the key recommendation to decrease DNC towards people with OUD is to improve the educational preparation of nurses, both in nursing school and within the hospital setting, through initial and continuing education and focused patient discussion. This recommendation aligns with a recent Nursing Economics call-to-action (Neville & Foley, 2020) for all nurses to combat the opioid epidemic from the perspectives of education, leadership, policy, economics, and research and focuses on the education of nurses in school and in the clinical setting. Nursing programs and the faculty charged with building curricula should expand instruction about OUD as a disease and highlight the potential implications of OUD for patients, communities, and the nurses who provide their care. Hospital systems should incorporate continuing education courses dedicated to OUD. This education should focus on how to recognize OUD, how to effectively manage the care of patients experiencing OUD, and ways to decrease stigma affecting this patient population.
Hospital systems should incorporate continuing education courses dedicated to OUD.Research about nurses’ attitudes and actions to decrease and eliminate stigma associated with OUD would provide helpful information. Studies related to nurses’ attitudes and DNC practices towards patients with OUD are needed to understand the etiologies of DNC and the subsequent ramifications for nurses and patients. Researchers could consider additional factors that cause nurses to treat patients with OUD differently than other patients, and the immediate repercussions of DNC during hospitalization. For example, from the patient perspective, a research question might be: How does experiencing DNC affect the current health status of patients with OUD at the time of the discriminatory treatment and immediately following the treatment? From the nurse’s perspective, one might ask how delivering DNC to patients with OUD affects the nurse’s perception of the quality of care they deliver, or how delivering DNC to this population compares to care delivered to patients without OUD. Longitudinal research might examine the long team effects of DNC towards patients with OUD on overall patient health status as well as to the patient relationship with opioids. Finally, longitudinal study could be helpful to investigate nurses’ coping mechanisms and evolving treatment of patients with substance use issues over the length of a career.
Limitations
The limitations of the current review included the restricted date range of articles published between 2016 and 2022 and the inclusion criteria of peer-reviewed articles written in English. Important data and themes in literature published before 2016 may have been missed, and a future review could include a broader date range to include studies conducted before and at the beginning of the opioid crisis. Additionally, because OUD is a highly stigmatized illness, the responses of individuals in the studies reviewed may be incomplete or reserved based on the fear of judgement or ramifications from their statements/responses. A final important limitation is the review of only literature pertaining primarily to OUD, which excluded the wide range of literature concerning SUD and related areas.
Conclusion
Discrimination in the provision of nursing care for anyone is an unacceptable practice.Discrimination in the provision of nursing care for anyone is an unacceptable practice. This integrative review provided an up-to-date, insightful summarization of DNC practices towards patients with OUD in the hospital setting. Relevant literature was evaluated, and data and themes were extracted and organized to provide a comprehensive view of the relationships between those experiencing OUD, the nurses who care for them, and others involved. It is our hope that the key contributing factors to DNC that we identified, the recommendations to eliminate discrimination toward this population by nurses, and our suggestions for future research will inform the next steps to support quality, appropriate care for all patients who experience OUD.
Authors
Jeanne Bernier, MSN, RN, CNL-BC
Email: jbernier@vols.utk.edu
ORCID ID: 0000-0001-7607-8363
Jeanne Adam Bernier is the director of the MSN-Clinical Nurse Leader (CNL) program at Mississippi College School of Nursing. She is a student in the PhD in Nursing program at the University of Tennessee Knoxville and her research area of interest is stigma and discrimination towards individuals with opioid use disorder. Jeanne holds a BSN from the University of Alabama Capstone College of Nursing, an MS in Nursing Education from the University of Mississippi Medical Center, and CNL certification from the Commission on Nurse Certification (CNC).
Cristina S. Barroso, DrPH, MPH
Email: cbarroso@utk.edu
ORCID ID: 0000-0002-4354-9058
Cristina S. Barroso is a health equity researcher who partners with community organizations, local and regional health departments, and policymakers to provide a more equitable physical and social environment so that all populations can achieve high health status to enable them to thrive in their communities. Cristina holds a BS in biology from the University of Michigan at Ann Arbor and an MPH and DrPH in health promotion-health education from the University of Texas School of Public Health.
References
American Hospital Association. (2021, January). Fast facts on U.S. hospitals, 2021. https://www.aha.org/statistics/fast-facts-us-hospitals
Blair, L. M., Ashford, K., Gentry, L., Bell, S., & Fallin-Bennett, A. (2021). Care experiences of persons with perinatal opioid use. The Journal of Perinatal and Neonatal Nursing, 35(4), 320-329.https://doi.org/10.1097/JPN.0000000000000597
Centers for Disease Control and Prevention. (2022). Opioid use disorder. U.S. Department of Health and Human Services. https://www.cdc.gov/drugoverdose/index.html
Cooney, M. F. & Broglio, K. (2017). Acute pain management in opioid-tolerant individuals. The Journal for Nurse Practitioners, 13(6), 394-399. https://doi.org/10.1016/j.nurpra.2017.04.016
Dineen, K. K. (2021). Disability discrimination against people with substance abuse disorder by postacute care nursing facilities: It is time to stop tolerating civil rights violations. Journal of Addiction Medicine, 15(1), 18-19. https://www.doi.org/10.1097/ADM.0000000000000694
Dydyk, A. M., Jain, N. K., & Gupta, M. (2022). Opioid use disorder. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK553166/
El Rasheed, A. H., El Sheikh, M. M., El Missiry, M. A., Hatata, H. A., & Ahmed, N. (2016). Addiction stigma among mental health professionals and medical students in Egypt. Addictive Disorders and Their Treatment, 15(4), 165-174. https://doi.org/10.1097/ADT.0000000000000090
Goffman, E. (1963). Notes on the management of spoiled identity. Simon & Schuster.
Hawk, K., McCormack, R., Edelman, J., Coupet Jr., E., Toledo, N., Gauthier, P., Rotrosen, J., Chawarski, M., Martel, S., Owens, P., Pantalon, M., O’Connor, P., Whiteside, L. K., Cowan, E., Richardson, L. D., Lyons, M. S., Rothman, R., Marsch, L., Fiellin, D., & D’Onofrio, G. (2022). Perspectives about emergency department care encounters among adults with opioid use disorder. JAMA Network Open, 5(1), 1-12. https://doi.org/10.1001/jamanetworkopen.2021.44955
Horner, G., Daddona, J., Burke, D. J., Cullinane, J., Skeer, M., & Wurcel, A. G. (2019). “You’re kind of at war with yourself as a nurse”: Perspectives of inpatient nurses on treating people who present with a comorbid opioid use disorder. PLoS ONE, 14(10), 1-15. https://doi.org/10.1371/journal.pone.0224335
Jaiteh, C., Steinauer, R., Frei, I. A. (2019). Individuals with opioid dependence using polysubstances: How do they experience acute hospital care and what are their needs? A qualitative study. Journal of Addictions Nursing, 30(3), 177-184. https://doi.org/10.1097/JAN.0000000000000294
Link, B. G, & Phelan, J. C. (2001). Conceptualizing stigma. Annual Review of Sociology, 27, 363-385. https://doi.org/10.1146/annurev.soc.27.1.363
Link, B. G., & Phelan, J. C. (2006). Stigma and its public health implications. Lancet, 367. 528-529. https://doi.org/10.1016/S0140-6736(06)68184-1
Mahmoud, K. F., Finnell, D. S., Sereika, S. M., Lindsay, D., Schmitt, K., Cipkala-Gaffin, J., Pushkar, K. R., & Mitchell, A. M. (2021). Personal and professional attitudes associated with nurses’ motivation to work with patients with opioid use disorder and opioid use-related problems. Substance Abuse, 42(4), 780-787. https://doi.org/10.1080/08897077.2020.1856287
Merriam-Webster. (2021, September 2). Discrimination. https://www.merriam-webster.com/dictionary/discrimination
Neville, K., & Foley, M. (2020). The economic impact of the opioid use disorder epidemic in America: Nurses’ call to action. Nursing Economics, 38(1), 7-51.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hrobjartsson, A., Lalu, M. M., Li, T., Lodler, E. W., Mayo-Wilson, E., McDonald, S., McGinness, L. A., Stewart, L. A., Thomas, J., Tricco, A. C., Welch, V. A., Whiting, P., & Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372(71). https://doi.org/10.1136/bmj.n71
Reese, S. E., Riquino, M. R., Molloy, J., Nguyen, V., Smit, M. C., Tenort, B., Gezinski, L. B., & Cleveland, L. (2021). Experience of nursing professionals working with women diagnosed with opioid use disorder and their newborns: Burnout and the need for support. Advances in Neonatal Care, 21(1), 32-40. https://doi.org/10.1097/ANC.0000000000000816
Sapp, A. J., & Hooten, P. (2019). Working with families impacted by the opioid crisis: Education, best practices, and providing hope. Archives of Psychiatric Nursing, 33, 3-8. https://doi.org/10.1016/j.apnu.2019.08.013
Shreffler, J., Shaw, I., McGee, S., Bishop, C., The, S., O’Brien, D., Price, T., & Huecker, M. (2021). Perceptions diverge on aspects related to substance use disorder: An analysis of individuals in recovery, physicians, nurses, and medical students. Substance Abuse, 42(4), 896-904. https://doi.org/10.1080/08897077.2021.1892014
Simon, R., Snow, R., & Wakeman, S. (2020). Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Substance Abuse, 41(4), 519-525. https://doi.org/10.1080/08897077.2019.1671942
Turner, C. C., Fogger, S. A., Frazier, S. L. (2018). Opioid use disorder: Challenges during acute hospitalization. The Journal for Nurse Practitioners, 14(2), 61-67. https://doi.org/10.1016/j.nurpra.2017.12.009
Whittemore, R. & Knafl, K. (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52(5), 546-553. https://doi.org/10.1111/j.1365-2648.2005.03621.x


