A reduction of alarm fatigue was achieved by decreasing alarms in a single patient room (SPR) neonatal intensive care unit after nurses reported alarm fatigue had greatly increased. The reduction resulted from a nurse-driven quality improvement project through the unit-based council in collaboration with leadership and a multidisciplinary team. Nurses identified, developed, and implemented the project to decrease alarms by 25% within four months. Short alarm delays on patient monitors and communication devices were responsible for a high number of non-actionable alarms. A need for staff education on proper utilization of the monitor silence and pause functions was identified. The unit found 107,000 total alarms in one month;this number was reduced to 36,248 alarms after intervention. By reducing high non-actionable pulse oximeter alarms, the project achieved an overall 40% reduction in total alarms received by nurses.
Key Words: Nursing, alarm fatigue, alarm reduction, unit-based council, neonatal intensive care unit, quality improvement, Neuman’s Systems Model
Alarm fatigue has been a high safety priority for over a decade after the death of a patient in 2010 due to an alarm being turned off. This event was the catalyst for The Joint Commission (TJC), the Emergency Care Research Institute (ECRI), the Food and Drug Administration (FDA), and other regulatory and patient safety organizations to convene a Alarm fatigue has been a high safety priority for over a decade [...]summit to scrutinize alarm safety (Horkan, 2014). In 2013, TJC released a report on alarm related events which found 98 clinical events reported between 2009 and 2012. Eighty of these patients died, thirteen suffered permanent loss of function, and five instances led to unexpected additional healthcare needs. Subsequently, TJC released National Patient Safety Goal #6 stating that healthcare facilities improve safety of clinical alarms systems and decrease alarm fatigue by 2016 (The Joint Commission 2015).
Decreasing alarm fatigue by addressing unnecessary alarms lies within the nursing practice scope of quality improvement. The unit-based council (UBC) within a shared professional governance (SPG) framework provides a forum for nurses to exercise ownership of their practice and demonstrate accountability for quality of care in their unit (Porter-O’Grady, 2023). Concerns that sequelae of alarm fatigue would lead to nurse burnout and turnover fueled staff engagement through a UBC-led, nurse-driven quality improvement project to decrease non-actionable, high pulse oximeter alarms in the neonatal intensive care unit (NICU) of a midwestern Magnet® hospital.
Decreasing alarm fatigue by addressing unnecessary alarms lies within the nursing practice scope of quality improvement.
If you were a NICU nurse receiving notification of 500 alarms in a 12-hour shift, what would you do? Studies of alarm fatigue in nurses have been reported in a variety of multipatient (open bay) room layouts and single patient room (SPR) NICUs (Johnson et al., 2017; Simpson & Lyndon 2019, van Pul et al., 2015). The SPR environment enhances family centered care and developmental care of the neonate because parents can room-in with their sick newborns. However, nurses cannot see multiple patients at one time, raising concerns about decreased visibility of critically ill neonates and equipment used in provision of care. Handheld devices (HHD) that connect nurses to patient monitors communicate change in patient condition to nurses (Walsh et al., 2015). While HHDs were initially lauded as assisting nurses in awareness of patient alarms, the additional number of alarms received have been burdensome and contribute to NICU nurse alarm fatigue (Sowan & Reed 2017).
Background
Alarm Fatigue
Alarm fatigue is defined as sensory overload when clinicians are exposed to an excessive number of alarms. This fatigue can lead to alarm desensitization, resulting in delayed or no response to alarms as well as missed alarms (Horkan 2014; Sendelbach & Funk 2013). As the day progresses, alarm fatigue increases in nurses and so does the rate of slow response time to alarms, disabling of alarms or alarm volumes, setting unsafe alarm parameters, and hesitation As the day progresses, alarm fatigue increases in nurses [...] in acknowledging and responding to other nurses’ patients’ alarms (Bonafide et al., 2015; Simpson & Lyndon, 2019; Sowan & Reed 2017). The conundrum resulting from this pattern ultimately compounds alarm-related patient safety concerns.
Actionable versus Non-Actionable Alarms
Actionable or ‘red’ alarms require clinical intervention based on patient parameters displayed via a red light on the patient monitor. Non-actionable, nuisance or ‘yellow’ alarms do not require staff intervention, are often generated by artifact or poor conduction, and display on patient monitors with a yellow-colored light. The TJC estimates 85-99% of alarms are non-actionable (Fujita & Choi, 2021). NICU nurses report non-actionable alarms as the major contributors to nursing alarm fatigue; they recommend measures to decrease alarm fatigue such as utilizing appropriate patient specific alarm parameters and not receiving all alarms on their phones (Simpson & Lyndon, 2019, van Pul et al., 2015; Walsh et al., 2015).
The TJC estimates 85-99% of alarms are non-actionable
Monitor lead dysconnectivity is a major contributor to non-actionable alarms in multiple patient populations. Cleansing the skin and changing monitor leads daily has been found to decrease alarms (Hravnak et al., 2018). The necessity of high isolette temperatures and humidity for low-birth-weight neonates contributes to lead dysconnectivity creating subsequent alarms. Due to the fragile condition of neonatal skin, daily changing of leads is not an option in the NICU population to reduce false alarms.
Noise levels in NICUs have been found to reach 120 decibels (dB). The American Academy of Pediatrics and the World Health Organization recommendations are a maximum of 45dB (Mayhew et al., 2022). Noises vary based on the care level of NICU. For example, a Level IIIc or IV typically has the highest noise level, secondary to caring for the highest acuity patients and utilization of higher-level technology (Mayhew et al., 2022). High acuity NICUs care for the smallest and the sickest infants, along with surgical, cardiac, extracorporeal membrane oxygenation (ECMO) patients, as well as infants with less threatening health issues. High acuity NICUs tend to have more patient beds and higher census. The environment of SPR NICUs is quieter than open bay NICUs (Almadhoob & Ohlsson, 2020; Mayhew et al., 2022).
Noises vary based on the care level of NICU.
Alarms, phones, bedside conversations, overhead loudspeaker announcements, not silencing alarms quickly, and all equipment have been identified as contributing factors to increased NICU environmental noise levels (Mayhew et al., 2022). Noise resulting in overstimulation of both staff and neonates is a by-product of alarms. Changing alarm limits, increasing alarm delay settings, and instituting specific patient profile alarm parameters can safely reduce alarms in open bay NICUs (Johnson et al., 2017). Researchers acknowledged that these findings may not be easily duplicated in SPR NICUs that utilize telecommunication alarm pathways (Johnson et al., 2017).
Due to lack of multiple patient visibility in SPR NICUs, HHD technology links patient monitors to nurses. Telecommunication pathways forward patient monitor alarms to a nurse’s HHD device and central monitor after a predetermined amount of time. By connecting nurses to patient monitor alarms, response time is improved. Nurses can then acknowledge, correct, or, if unable to attend to the alarm, can escalate the alarm to someone else’s HHD. Escalated alarms are perceived as additional noise by nurses, and the lack of filtering non-actionable or false alarms is specifically cited as burdensome (Lewandowska, 2020; Sowan & Reed, 2017).
Noise resulting in overstimulation of both staff and neonates is a by-product of alarms.
Shared Professional Governance
Collaborative relationships between nurses, the interdisciplinary team, leaders, and managers have a positive impact on the workplace environment. According to Van Bogaert et al. (2016) these positive relationships occur in environments consisting of shared values, shared governance, and structural empowerment. Betty Neuman’s Systems Model in nursing practice states the client is an individual, family, and community living within a culture, the global community, and the world (Neuman, 1996). This environment for one client consists of physiologic, developmental, psychosocial, interactional, spiritual, and material factors (Aylward, 2006). The client is an open system interacting with the other parts of the environment. As with Neuman’s model, the positive workplace environment requires the system to work together to achieve wellness and health and to maintain homeostasis (e.g., positive nurse and patient outcomes). These factors come together at any one time for one nurse, and can provide touchpoints, or opportunities, for nursing intervention, engagement, and empowerment.
When buy-in aligns with a responsive manager and an engaged and empowered UBC, the impact on patient safety and the work environment is demonstrated through the council’s quality work. Using interdisciplinary teamwork, nurses can identify problems and implement changes to improve patient care and safety, nursing satisfaction, and a safe work environment. The opportunity to engage nurses in the decision-making process has resulted in positive outcomes in patient safety, quality improvement, and nurse satisfaction at the bedside (Kutney-Lee et al., 2016). A key component to staff engagement is the concept of buy-in, which according to Porter O’Grady and Malloch (2011) is essential for success.
Engaging bedside clinical nurses in shared governance decision-making impacts healthcare quality (Van Bogaert et al., 2016). The National Database of Nursing Quality Indicators (NDNQI) data provides evidence that nurse engagement has a direct impact on patient experience, clinical quality, and patient outcomes (Montalvo 2007). A NDNQI survey revealed that the most common reason nurses plan to leave a position within one or three years was dissatisfaction with the work environment (Press Ganey 2018). Data shows that highly engaged nurses are 87% less likely to leave the organization (Assi & Freeman, 2018).
Shared governance has been found to correlate with workplace empowerment and staff and job satisfaction; recent evidence has also demonstrated increased staff engagement, especially in quality improvement processes (Olender et al., 2020). Nurses who felt their professional decisions were valued and welcomed experienced feelings of control over their work, and increased meaning and impact in their work. They were more satisfied at work and had higher perceptions of an empowering workplace (Kretzschmer, 2017). Processes that allow equity in decision making, with bedside nurses leading the way, have demonstrated support of the shared governance framework (Brennan & Wendt, 2021).
This article describes a quality improvement project that enlisted the unit SPG UBC to reduce alarms in a level IV NICU in a Magnet® designated, midwestern, free standing pediatric hospital. This occurred after transitioning from open bay style to SPRs. The following nurse-driven quality improvement project exemplifies the concepts of nurse engagement and empowerment.
Processes that allow equity in decision making [...] have demonstrated support of the shared governance framework
Nature and Significance of the Local Problem
The NICU provides specialized care to premature and ill newborns who require continuous care and monitoring. The local problem of alarm fatigue emerged after transitioning from an open bay style to a SPR NICU. Prior to the transition, the open bay style NICU afforded simultaneous observation of several infants, and nurses were able to address monitor alarms of any patient they could see or hear. After the transition to SPRs, nurses could no longer see multiple patients. Hand-held devices were instituted to connect nurses to patient monitors due to staff apprehension about inhibited visibility of patients and concern for patient safety after moving from an open bay style NICU to a SPR environment.
The local problem of alarm fatigue emerged after transitioning from an open bay style to a SPR NICU.
This technology utilized narrow alarm limits to communicate patient alarms to the HHD. Narrow alarm limits from patient monitors to HHD have been a customary practice for neonatal units moving to SPRs, secondary to similar concerns (Walsh et al., 2015). The patient monitor factory default was set at a 15 second delay and transfers to the HHD after another 20 seconds; this gives nurses minimal time to address alarms. The alarm escalates to other nurses’ HHDs and central monitor banks, leading to a high number of alarms and environmental noise.
Nurses began to report excessive alarm numbers on their HHD to UBC leaders within four months of the unit’s transition to SPRs. UBC leaders requested that nurses continue reporting the number of alarms received during their shift. This request generated an overwhelming response of a high number of alarms per shift received by nurses on their HHD, including as high as 543 alarms in 12 hours, and 120 alarms in 2 hours. Nurse concerns and data were reported to unit leadership during UBC meetings.
Unit leadership investigated the unit alarm data, which revealed high numbers of non-actionable alarms. Text messages between nurses were found on HHD stating, “I can’t take this anymore; I don’t want to come back,” highlighting an urgent need for intervention. These comments, along with high numbers of alarms reported, raised concern of nurse dissatisfaction, turnover, staff burnout, and potential patient safety events related to alarm fatigue.
Nurses began to report excessive alarm numbers [...] within four months of the unit’s transition to single rooms.
As leadership acknowledged the nurses’ concerns and began to examine the issue, nurses became more engaged and empowered. Clinical systems analysts reviewed monthly alarm logs and trends. Nurse leaders proposed the development of an alarm fatigue committee in collaboration with the UBC. A NICU Alarm Fatigue Committee was convened, comprised of twelve staff nurses, nursing leadership, a NICU Quality Improvement nurse, respiratory therapists, physicians, and the clinical systems nurse analyst. The UBC co-chairs, nurse manager, and NICU medical director shared committee chair responsibilities. The nurses engaged by joining the committee and working on identified root causes of alarms through subcommittees. Nurses reported their work through the UBC and continued to report on HHD alarm numbers by open communication with the UBC leaders.
Rationale and Aims
The NICU UBC recognized that concerns raised by the nurses required engagement and active participation. The council members engaged leadership to address nurse alarm fatigue by identifying the local problem at their meetings. Nurses identified the problem, helped design solutions, and were proactive in implementing and evaluating the change. These actions demonstrated their ownership of the alarm reduction project and supported the developing theory of implementing change from the bottom-up by recognizing the expertise and input of the bedside nurse to facilitate quality improvement (Bergstedt & Wei, 2020, Bleich, 2018).
Nurses identified the problem, helped design solutions, and were proactive in implementing and evaluating the change.
A global aim of alarm reduction was established with a smart aim to reduce alarms by shift, and total number of alarms by 25% within six months. The Alarm Fatigue Committee identified key drivers for investigation and resolution of unit alarm fatigue (See Figure 1). The key drivers established methods for improvement processes with technology usage and staff knowledge. The Alarm Fatigue Committee determined reducing non-actionable alarms would reduce nurse alarm fatigue and improve workflows while not impairing patient safety. The nurse clinical systems analyst reviewed monthly alarm logs and trends and reported 87,000 – 107,000 alarms/1000 patient days at the start of the project.
Figure 1. NICU UBC Alarm Fatigue Project
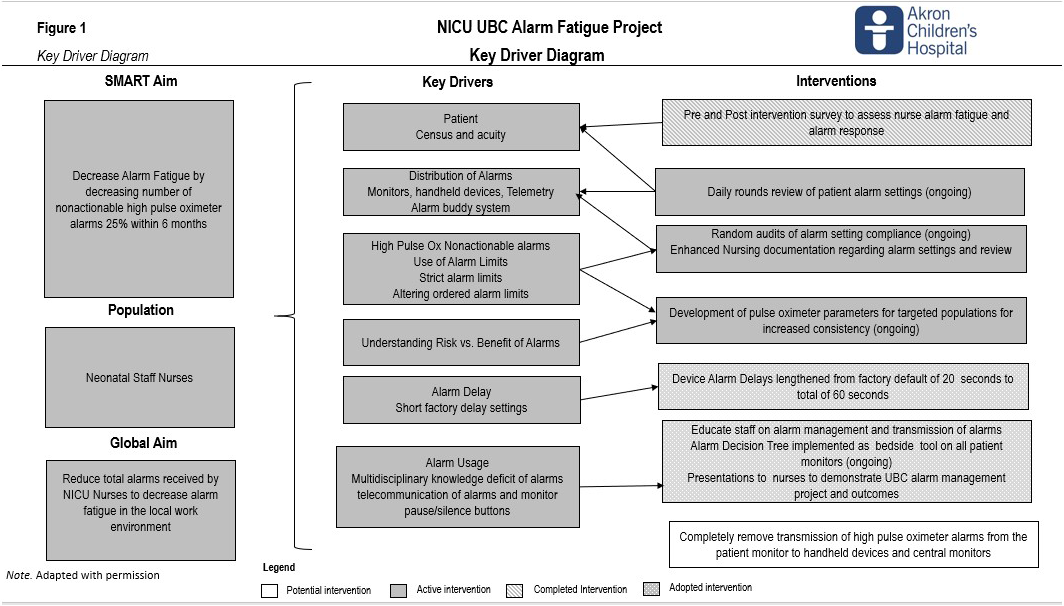
The Alarm Fatigue Committee identified key drivers for investigation and resolution of unit alarm fatigue
Alarm Fatigue Methods
Subcommittees were formed with nurses present in each group to address the identified issues of concern.
Interventions
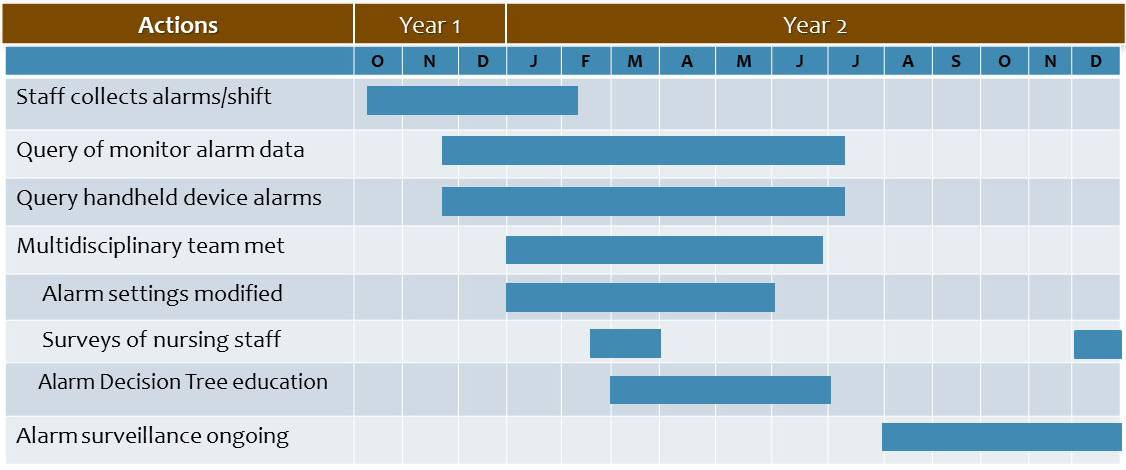
The committee established a project timeline (See Figure 2) and conducted an anonymous, web-based pre-intervention survey of nurses to gain insight into nurse perception of alarm fatigue. The survey queried nurses about disruption of workflow from alarms received, and observations on underlying causes of delayed response to alarms, secondary to alarm fatigue. The survey response rate of 79% (n = 150; n =119) demonstrated nurse engagement and enabled the Alarm Fatigue Committee to identify contributing factors to high alarm numbers. Root causes identified through the survey were separated into action categories including knowledge, culture change, environmental impact, and change in technology. Subcommittees were formed with nurses present in each group to address the identified issues of concern. The unit nurse manager ensured staff continued participation by providing compensated project time to support involvement.
Figure 2. Timeline NICU UBC Fatigue Alarm Project
Review of the literature by UBC leaders revealed little evidence to support alarm fatigue management in the neonatal population. The initial alarm data audit review supported the high number of alarms experienced by nurses. Non-actionable alarms had the greatest impact on workflow and alarm fatigue, as identified by nurses completing the pre-intervention survey. Thus, the committee focused on reduction of high non-actionable pulse oximeter alarms.
Non-actionable alarms had the greatest impact on workflow and alarm fatigue[...]
Environmental Noise
The nurse pre-intervention survey identified that the environmental noise generated by phones and monitor banks was overwhelming. The process in the new unit was that only secretaries would answer phones due to the size of the unit and their ability to easily locate call recipients. The process did not recognize the impact of loud noise from phones ringing at nurses’ stations, where nurses were not permitted to answer. This was addressed by silencing the phones at the nurses’ station.
Each wing in the NICU has central monitor banks located at each nurse’s station. These monitors display trends and alarms for each patient and were also identified as environmental noise. The monitors sounded for all patient alarms, such as heart rate, respiration, and oxygen saturation levels, as well as artifact. At times, with multiple babies alarming at once, the sound level at the nurses’ stations was found to be 85dB. This is comparable to standing near a running lawnmower. Further investigation found that the central monitors were set at the factory default volume of 10, the loudest level, since installation in the new unit. The volume level on all central monitor banks was reduced to a hospital mandated safe volume of two out of ten with positive environmental results (Akron Children’s Hospital, 2021).
The nurse pre-intervention survey identified that the environmental noise generated by phones and monitor banks was overwhelming.
Alarms
The nurse clinical systems analyst provided projected data on how proposed alarm delay changes in the communication pathway from patient monitor to HHD would impact alarm numbers prior to actual changes. Initially, all monitor alarm delays to HHD were increased from factory default settings of 20 seconds to 35 seconds when data review revealed a significant increase in alarm numbers to 107,000 due to a practice change through a national collaborative to reduce retinopathy of prematurity. Progressive changes were made based on projections until a final alarm delay of 60 seconds from patient monitor to HHD was reached. These progressive changes resulted in nurses having more time to respond to alarms prior to escalation. A post-intervention survey was conducted six months after implementation of interventions. This six-month interval allowed time for nurses to implement and integrate the interventions learned into practice.
Alarm Orders
Random audits of providers and staff during rounds ensured alarm order compliance was instituted and ongoing. Daily review of pulse oximeter orders on rounds was implemented to prevent multiple current orders in the patient chart. The development of pulse oximeter parameters for targeted patient populations was implemented to increase consistency with provider orders. Nursing documentation was updated to reflect daily discussion of pulse oximeter by providers. Providers receive reminders that ventilator settings might need adjustment for patients using 21% oxygen and experiencing high pulse oximeter alarms, indicating an opportunity for ventilator weaning.
Random audits of providers and staff during rounds ensured alarm order compliance was instituted and ongoing.
Education
The Alarm Fatigue Education Subcommittee developed an educational intervention to improve alarm management skills for all staff. The unit educator, UBC chair, and nurses met with monitor representatives to learn the alarm pathway from the patient monitor to the nurses’ HHD and to the central monitors. The differences between the monitor alarm pause and silence buttons were defined and an algorithm, named the Alarm Decision Tree, was developed to guide staff in alarm management decision-making (See Figure 3).
Figure 3. Alarm Decision Tree
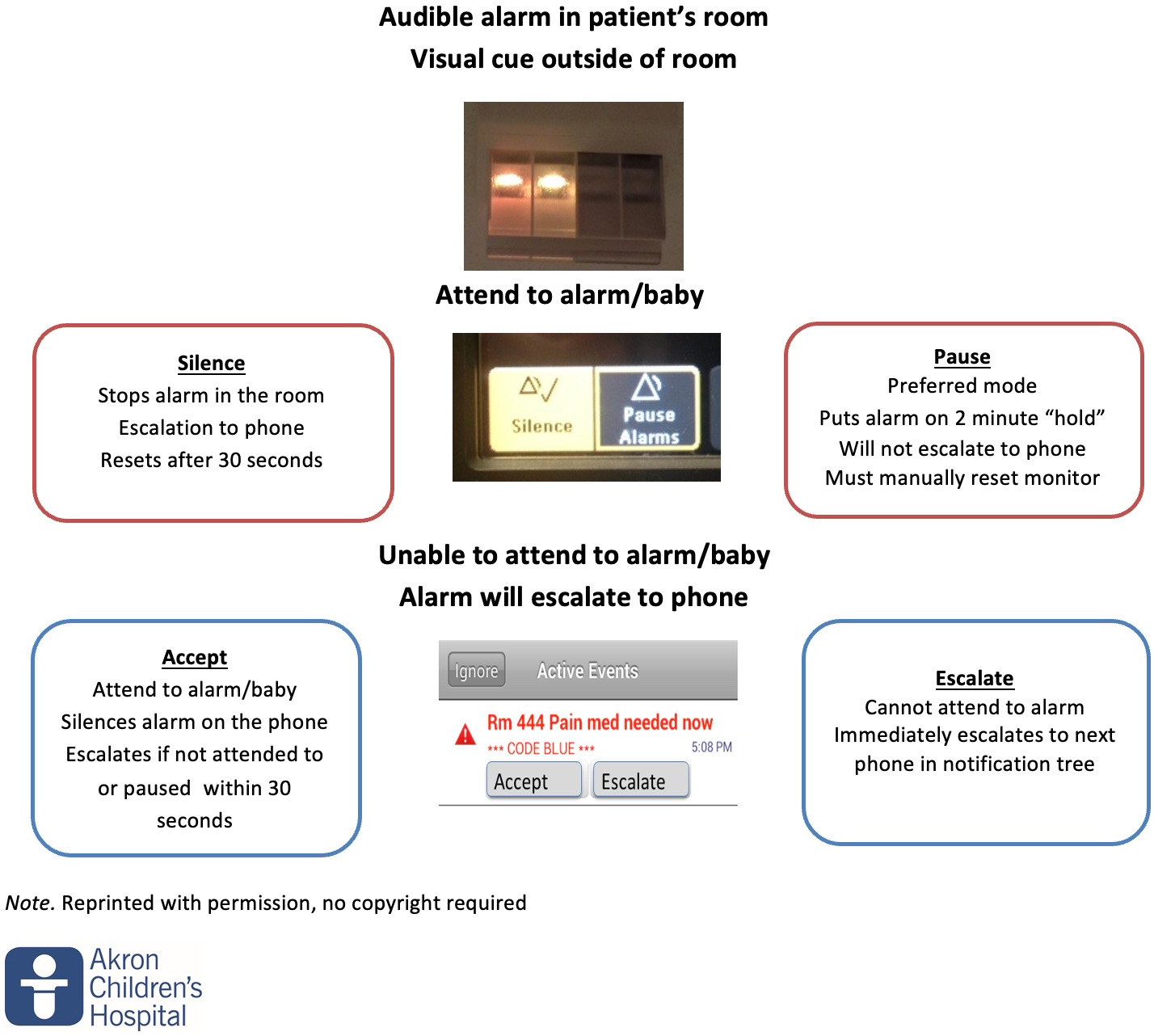
The Alarm Decision Tree is an educational visual algorithm placed at every patient monitor to assist staff with choosing an alarm silence mode. The Alarm Decision Tree was developed, reviewed, and instituted after piloting by nurses and review by the NICU Quality Improvement Council. This directs nurses about how to pause, silence, and suspend patient alarms, which thereby blocks escalation of alarms to devices, peers, and other staff. Nurses took the education one step further by ensuring that ancillary staff who entered patient rooms were educated on alarm management and how to safely silence alarms. Nurse education was implemented and communicated via in-services, information sheets, picture algorithms at the bedside, email updates, pre-shift huddles, UBC and nursing staff meetings, and face to face communication.
Results
Environmental Noise
The web based anonymous pre-post intervention survey on unit alarm fatigue queried nursing staff (n = 150) about disruption of workflow from the non-actionable alarms that they received. This provided nurse observations on underlying causes of delayed response to critical alarms secondary to alarm fatigue, and suggestions for improvement. Nurses were engaged as evidenced by a pre-intervention survey response rate of 75% (n = 119) and post-response rate of 53% (n = 80) at the six-month point.
We asked nurses about the percentage of clinical alarms they encountered that did not require clinical intervention.
We asked nurses about the percentage of clinical alarms they encountered that did not require clinical intervention. In the pre intervention survey, participants (n = 71) indicated that alarms were non-actionable 60% of the time more than 50% of their shift; post intervention respondents (n = 30) rated this at 38% (see Table 1). Additionally, nurses reported that these false or non-actionable alarms were disruptive to their daily workflow 91% (n = 108) pre, and 74% (n = 60) post intervention, again more than 50% of their shift time. Committee members discovered the need for alarm pathway education when nurses reported what they observed as the underlying cause for staff delay in response to an alarm. Forty-two percent ( n = 35, pre) answered that they watched the central monitor and knew the alarm did not need action, with 44% (n = 37, pre) stating they were waiting for the patient to self-correct. When asked to rank the increase in alarm fatigue since moving to SPRs, nurses completing the preintervention survey 88% (n = 105) indicated that responded alarm fatigue had greatly increased, while in the post survey this number decreased to 55% (n = 44).
Table 1. Pre and Post Intervention Survey Results
| Item | Pre survey (n = 119) |
Post survey (n = 80) |
||
|---|---|---|---|---|
| n | % | n | % | |
| Of all the clinical alarms you encounter, estimate the percent that are false or irrelevant (the patient does not require clinical intervention) | ||||
| No Response | 1 | 1 | 0 | 0 |
| 0-10% | 2 | 2 | 3 | 4 |
| 11-25% | 10 | 8 | 21 | 26 |
| 26-50% | 35 | 29 | 26 | 32 |
| 51-75% | 59 | 50 | 28 | 35 |
| 76-100% | 12 | 10 | 2 | 3 |
| How disruptive are false or nuisance clinical alarms to your daily workflow? | ||||
| No Response | 4 | 3 | 6 | 8 |
| 0-24% of time | 3 | 3 | 7 | 9 |
| 25-49% of time | 4 | 3 | 7 | 9 |
| 50-74% of time | 43 | 36 | 45 | 56 |
| 75-100% of time | 65 | 55 | 15 | 18 |
| What is the most common complication/frustration you have felt regarding monitor alarms | ||||
| No Response | 0 | 0 | 0 | 0 |
| I am not frustrated by alarms | 3 | 3 | 7 | 9 |
| I am frustrated by answering my "buddy's" alarms as well as my own | 6 | 5 | 9 | 11 |
| Alarms are not easily adjusted to be patient specific | 29 | 24 | 20 | 25 |
| Most alarms sound for nuisance reasons, not patient physiologic reasons | 21 | 18 | 8 | 10 |
| Alarms sound so frequent they awaken/upset the patient/family | 9 | 7 | 3 | 4 |
| Alarms sound so frequently | 51 | 43 | 33 | 41 |
| Has alarm fatigue increased since being in single patient rooms with the Voalte phones? | ||||
| No Response | 2 | 2 | 4 | 5 |
| Alarm Fatigue has not increased | 2 | 2 | 5 | 6 |
| Alarm fatigue has increased slightly | 10 | 8 | 27 | 34 |
| Alarm Fatigue has increased greatly | 105 | 88 | 44 | 55 |
| Since moving to single patient rooms, if you have witnessed a delay in response from an urgent situation due to alarm fatigue, what was the underlying cause? | ||||
| No Response | 3 | 3 | 1 | 1 |
| Waiting to see if patient corrects | 44 | 37 | 31 | 39 |
| Waiting for primary nurse to respond | 22 | 18 | 17 | 21 |
| Waiting for another to respond | 8 | 7 | 9 | 11 |
| Could see the monitor (or central station) and knew that alarm did not need action | 42 | 35 | 22 | 28 |
The pre-intervention survey results included 68 individual nurse suggestions and comments on how to reduce alarm fatigue, some extremely detailed. Over 50% of these comments were specific to removing high non-actionable alarms or expressed dissatisfaction specifically with the number of these type alarms. Environmental issues were identified factors, such as volume on central monitors, ringing nurse station phones, and the transmission of alarms from the assigned nurse to a neighboring nurse, resource person and charge nurse. Factors were identified regarding strict alarm limits, factory set short delays in the telecommunication pathway, variance in alarm limits, and noncompliance with ordered alarm limits. Also highlighted was a cross-disciplinary knowledge deficit for all staff regarding telecommunication process of alarms and use of monitor silence and pause buttons.
The pre-intervention survey results included 68 individual nurse suggestions and comments on how to reduce alarm fatigue[...]
Other contributing factors identified were implementation of high pulse oximeter limits set at 99% to reduce retinopathy of prematurity, multiple pulse oximeter order sets on patient charts, and provider resistance to changing pulse oximeter limits. Nurses emphasized that infants with an order for a set oxygen concentration with high pulse oximeter alarm limits set at 99% frequently rang. In these cases, the nurses could not decrease the oxygen, yet were not allowed to turn the high limit to 100%. In this instance, the alarm limit of 99% could cause continual alarm notifications.
Nurse Excerpt in Comments from Alarm Fatigue Survey
The following quote was provided by a NICU nurse in the presurvey.
In this unit, if you are anywhere near the desk you get: alarms high and low for your babies on your phone, alarms for your babies high and low from monitors in the room, alarms high and low for your babies from the central monitors, alarms high and low from your buddies babies on your phone, alarms high and low from your buddies’ babies from the monitors in the rooms, alarms high and low from your buddies’ babies on the central monitors, IV alarms from all babies in your areas, feeding pump alarms from all babies in your area, Isolette alarms from all babies for water, 02 calibration, too hot, too cold, etc. the tube system alarms when too many canisters are there (not to mention the noise when they drop in or take off), vent alarms for all babies/for ALL kinds of stuff. Heaven forbid they have a leak, and you cannot control the alarming. Every time anyone uses their badge to get in or out of their computer, go in or out of the med room etc., it BEEPS. In the couple of minutes it took me to fill this out my brain has been inundated with ALL these noises-and I was just interrupted with a false alarm page overhead that seems to happen at least once daily. I am sure there are more, these are just the ones I’ve noticed in these couple of minutes- multiply that by 12 sometimes 16 hours.
Neonatal Nurse (submitted anonymously)
In contrast to the 68 comments on the pre-intervention survey, 35 nursing comments were received on the post-intervention survey suggesting a reduced concern with alarm fatigue. Comments on the post survey showed continued desire to decrease alarms and less concern for non-actionable alarms.
Alarms
The global aim of reducing high pulse oximeter alarms by 25% within six months was achieved within four months. Pre-intervention, initial alarm data showed over 87,000 alarms were generated to nurses’ HHD within a period of one month. The three wings in the 75-bed level IV NICU are comprised of twenty-five bed units. The acute care wing experienced 82% of alarms with the sub-acute wing receiving 17% and the convalescent wing receiving 1%. Data review identified the major contributor to number of alarms received were non-actionable high pulse oximeter alarms. These numbers represented an alarm frequency as high as one alarm every 1-2 minutes for NICU patients sent to nurses’ HHDs.
The global aim of reducing high pulse oximeter alarms by 25% within six months was achieved within four months.
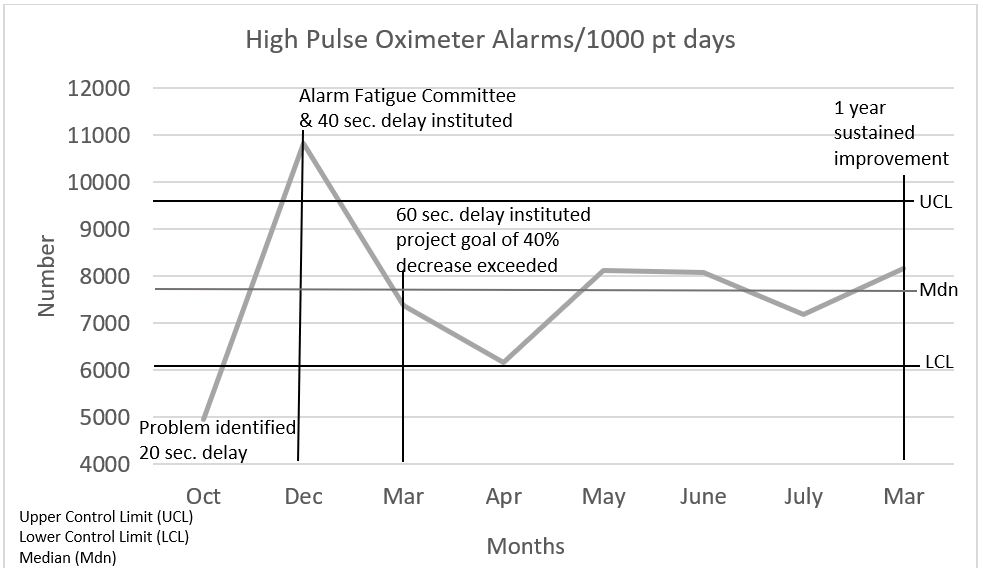
Four months after initiating interventions, the monthly high saturation pulse oximeter alarm data review showed a total of 6,166 alarms/1,000 patient days compared to 10,834 alarms/1,000 patient days prior to the interventions (see Figure 4). The alarm delay from patient monitor to HHD was changed incrementally over a period of four months from a total 35 second delay to a total delay of 60 seconds. The last change to a delay of 60 seconds was reviewed after two weeks of implementation and resulted in a reduction of high pulse oximeter alarms from a total of 10,834alarms/1,000 patient days to 7,380 alarms/1,000 patient days during that time frame. The progressive changes in the monitor communication pathway resulted in decreased non-actionable alarms and allowed nurses more time to respond to alarms before they escalated to peers and other staff. The post intervention alarm review showed that alarm frequency decreased to one alarm every four to five minutes, resulting in an average of 180 – 223 alarms in a 12-hour shift for nurses.
Figure 4.
Discussion
Nurses were engaged and committed to solving the issue to improve their work environment, prevent staff turnover, and assure patient safety. The high pulse oximeter non-actionable alarms were found to be high in frequency and the most mentioned by staff in an alarm fatigue survey as a nuisance. Staff nurses continued engagement was confirmed by a post-intervention survey response rate of 53% (n=80) which was decreased by 66% compared to the pre-survey response rate (n=119). This response rate along with the dramatically reduced alarm numbers, impacted by the project interventions, indicated an increase in nurse satisfaction (see Table 1).
Nurses were engaged and committed to solving the issue to improve their work environment, prevent staff turnover, and assure patient safety.
Interpretation
Nurses were adapting to a new practice environment of a SPR NICU while experiencing one alarm every 1-2 minutes to their HHDs. Alarm fatigue created the stimulus needed for NICU nurses to take ownership of this project. Nurses communicated the problem to UBC leadership and engaged in the design, trial, implementation, and follow up on this project to reduce alarm fatigue. The ability of the UBC to align staff nurses with nursing leadership and physicians to address and problem solve was key to the success of this project.
The alarm fatigue reduction project had a positive impact on the NICU. Environmental noise was reduced by quieting monitor banks and desk phones. The overall decrease in alarms and nurses’ post intervention survey responses support a decrease in risk of patient safety from alarm fatigue in the NICU. This, along with the reduction in alarm data, reflected the quieter environment for nurses and patients. The project was recognized within our hospital, resulting in hospital wide UBCs seeking assistance with their unit alarm fatigue. While alarm related patient safety was not specifically measured in this project, patient safety metrics for the unit were maintained and the literature provides convincing evidence that alarm fatigue impacts patient safety. The NICU UBC demonstrated what can be accomplished when nurses are not only heard, but listened to, and leadership is dynamic and responsive (Kretzschmer et al., 2017).
The influx of new nurses has significantly increased due to the “great resignation” of 2020 and the trend of travel nursing (Martin et al., 2023). For nurses who are new or lack previous exposure to alarms, receiving one alarm every four to five minutes is still perceived as burdensome and requiring attention. The UBC is in the process of re-examining the alarm process to gain insight into further reduction of alarms.
The alarm fatigue reduction project had a positive impact on the NICU.
Limitations
A gap when dealing with neonatal patients is the lack of descriptive safe parameters for pulse oximeter limits, especially in premature infants. The physiologic pattern of neonates having wide swings in pulse oximeter readings secondary to presence of sporadic movement, a patent ductus arteriosus, compliant chest walls, and variable respiratory patterns contribute to bedside alarms. The NICU continues to participate in The Vermont Oxford Network to establish safe pulse oximeter alarms for our patients (Edwards, Ehret, Soll, & Horbar, 2019).
The lack of literature specific to alarm fatigue in SPR neonatal units is confounded by the inability to generalize studies. The SPR environment creates a different scenario than the open bay style NICU due to use of HHD, which can impact alarm fatigue. This NICU is a level IV and had high census and acuity when moving into the SPR environment. The variability in patient census and acuity in any NICU can influence data alarm numbers, but it cannot be controlled or predicted.
The NICU continues to participate in The Vermont Oxford Network to establish safe pulse oximeter alarms for our patients.
Internal limitations were evident during the project due to a change in the clinical systems analyst’s position. Our initial data were not reviewed based on 1,000 patient days which is the unit’s preferred incident rate measurement. The data were recalculated from the prior datasets and patient census for consistent measurement analysis. The committee did not remeasure the decibel level after the alarm reduction and environmental interventions were implemented. This measurement would have provided further data to support the impact of the interventions on the work environment.
Nurse use of the Alarm Decision Tree algorithm was not measured but would have been beneficial to determine the impact of the Alarm Decision Tree education. The clinical systems nurse analyst can print a call activation summary, which reports specific types of alarms and action taken via the room monitor in any given time frame providing information on use of the Alarm Decision Tree. It records the length of the alarm, details of the response, time of the suspension, when it was acknowledged, and how often it occurred for the same instance. This data would have provided pre and post data on the effectiveness of the educational intervention.
Conclusion
This nurse driven quality improvement project, along with the support of a dynamic UBC, reduced non-actionable alarms in the local work environment by over 40% within four months. The project provides evidence that bedside nurses can identify problems and implement changes to improve patient care, safety, and nurse satisfaction. Reduced alarm fatigue and a safer work environment resulted from interdisciplinary teamwork through the UBC. Alarm management is driven by understanding the local environment and the use of technology. Education on the utilization of modern technology in the work environment is an essential intervention. In addition, the technology must be compatible with the local work environment and patient population.
Alarm management is driven by understanding the local environment and the use of technology.
Attention to alarm factory default settings and adjusting to appropriate patient parameters will help decrease alarm fatigue. Continued inquiry into safe alarm parameters for neonatal patients is recommended. Call activation summaries can be beneficial to examine trends of staff response to alarms. Ongoing monitoring of environmental noise is important for patient and staff homeostasis.
The presence of a structured and progressive UBC provides the environment for nurses to impact patient safety and staff satisfaction by channeling knowledge and expertise into quality improvement projects. The shared governance It is the observations and experiences of nurses at the bedside that lead to successful quality improvement. elements of partnership, equity, accountability, and ownership at the point of service are essential. It is the observations and experiences of nurses at the bedside that lead to successful quality improvement.
Acknowledgements:
The authors declare there are no financial conflicts of interest to disclose.
The authors wish to acknowledge the Akron Children’s Neonatal Intensive Care nursing staff and Unit Based Council for their initiative on this project, continued contributions to data collection, and
dedication to patient safety with special thanks to Evelyn Sell, BSN, RN, Lillian Kay Esker, BSN, RN, and Jamie August, MSN, RN.
We gratefully acknowledge the Akron Children’s leadership team, Maggie Arbaugh MSN, Christine Young DNP, MBA, RN, NEA-BC, Connie Teal DNP, RNC-NIC, APRN-CNS, WCC, Lela Bartley MSN, Denise Saraniti MSN, RNC-NIC, Monica Smith MSN, RNC-NIC, Anand Kantak M, F.A.A.P., and Jennifer Grow MD, F.A.A.P., along with the contributions of Tammy Troyer MSN, RN, and Vickie L. Webb MSN, RN-BC, CPN for data aggregation and analysis. The authors also wish to recognize Akron Children’s Hospital and so many who offered support during this project.
Authors
Colette V. Benincasa, MSN, RN, C-NPT
Email: cbenincasa@akronchildrens.org
Colette V. Benincasa, MSN, RNC-NPT, Akron Children’s Hospital has been a NICU staff and transport nurse for almost 39 years. Colette has served as Co-chair of the Unit Based Council, member of the House Wide and Transport Quality Improvement Councils and recently stepped down as Chair of the NICU Unit Based Council. Colette develops quality initiatives for the NICU, the transport team, and is a NRP and S.T.A.B.L.E lead instructor. She participated in the Vermont Oxford Collaborative and served as Principal Investigator on Safe Sleep Transitioning in the NICU. She has presented on leadership, QI projects and NICU alarm fatigue at the local, state, and national level and is a member of Sigma Theta Tau and NANN.
Kathleen A. Bailey, BSN, RN
Email: kbailey55@neo.rr.com
Kathleen A. Bailey, BSN, RN worked as a NICU nurse for 43 years, serving as NICU Head Nurse, Nurse Program Coordinator of NICU Follow-up Clinic, and Principal Investigator on music therapy use in NICU. Kathleen served as first chair of NICU’s Shared Governance Council and developed the council’s structure and credibility in its infancy. She led initiatives concerning staff satisfaction and quality improvement. Kathleen coauthored and published two chapters on NICU related topics. Kathleen has presented at local, state, and national levels on the continuum of care for NICU patients. She championed nurse engagement, and has presented at the local, state, and national levels about alarm fatigue in the NICU.
Aris Beoglos Eliades, PhD, RN, CRN-BC
Email: ariseliades@gmail.com
ORCID ID: 0000-0002-3864-6128
Dr. Eliades has extensive clinical, faculty and research experience having worked as a nurse, nurse scientist, and certified clinical research nurse in NICUs and as Director of Nursing Research. A published author, reviewer, and national and international presenter whose research interests include pain location assessment, thermometry devices, mentoring, nursing workforce and neonatal and pediatric nursing practice topics. Dr. Eliades is a member of ANA, Society of Pediatric Nurses, MNRS, past-President of Delta Omega Chapter of Sigma Theta Tau International and President of the International Association of Clinical Research Nurses.
References
Akron Children’s Hospital. (2021). Management of clinical alarms. #10457. Unpublished internal company document
Almadhoob, A., & Ohlsson, A. (2020). Sound reduction management in the neonatal intensive care unit for preterm or very low birth weight infants. The Cochrane Database of Systematic Reviews, 1, CD010333. https://doi.org/10.1002/14651858.CD010333.pub2
Assi, M.J., & Freeman, A. (2018). Developing a strategic connection between nursing excellence and workforce engagement [Webinar]. Press Ganey. Retrieved from https://www.njha.com/media/569363/2018Press-GaneyNursingSpecialReport.pdf
Aylward, P.D. (2006). Betty Neuman: The Neuman systems model and global applications. In M.E. Parker (Ed.) Nursing theories and nursing practice (2nd ed., pp. 281-294). Davis.
Bergstedt K, Wei H. (2020). Leadership strategies to promote frontline nursing staff engagement. Nursing Management, 51(2), 48–53. https://doi.org/10.1097/01.NUMA.0000651204.39553.79
Bleich M. R. (2018). Shared governance-shared leadership: Opportunities for development. Journal of Continuing Education in Nursing, 49(9), 394–396. https://doi.org/10.3928/00220124-20180813-03
Bonafide, C., Lin, R., Zander, M., Graham, BA., Paine, C., Rock, W., Rich, A., Roberts, K., Fortino, M., Nadkarni, V., Localio, R., & Keren, R. (2015). Association between exposure to nonactionable physiologic monitor alarms and response time in a Children’s Hospital. Journal of Hospital Medicine, 10(6). 345-351. https://doi.org/10.1002/jhm.2331
Brennan, D. & Wendt, L. (2021). Increasing quality and patient outcomes with staff engagement and shared governance. OJIN: The Online Journal of Issues in Nursing, 26(2). https://doi.org/10.3912/OJIN.Vol26No02PPT23
Cvach, M., Rothwell, K. J., Cullen, A. M., Nayden, M. G., Cvach, N., Pham, J. C. (2015). Effect of altering alarm settings: A randomized controlled study. Biomedical Instrumentation &Technology, 49(3), 214-222. https://doi.org/10.2345/0899-8205-49.3.214
Edwards, E. M., Ehret, D. E. Y., Soll, R. F., & Horbar, J. D. (2019). Vermont Oxford Network: a worldwide learning community. Translational pediatrics, 8(3), 182–192. Retrieved from https://tp.amegroups.org/article/view/27334/24533
French-Bravo, M., & Crow, G. (2015). Shared governance: The role of buy-in bringing about change. OJIN: The Online Journal of Issues in Nursing, 20(2). https://doi.org/10.3912/OJIN.Vol20No02PPT02
Fujita, L. Y., & Choi, S. Y. (2020). Customizing physiologic alarms in the emergency department: A regression discontinuity, quality improvement study. Journal of Emergency Nursing, 46(2), 188–198.e2. https://doi.org/10.1016/j.jen.2019.10.017
Horkan, A. M. (2014). Alarm fatigue and patient safety. Nephrology Nursing Journal, 41(1), 83-85. Retrieved from https://pubmed.ncbi.nlm.nih.gov/24689269/#:~:text=doi%3A%2010.1097/NCI.0b013e3182a903f9
Hravnak, M., Pellathy, T., Chen, L., Dubrawski, A., Wertz, A., Clermont, G., & Pinsky, M. R. (2018). A call to alarms: Current state and future directions in the battle against alarm fatigue. Journal of Electrocardiology, 51(6S), S44–S48. https://doi.org/10.1016/j.jelectrocard.2018.07.024
Johnson, K. R., Hagadorn, J. I., Sink, D. W. (2017). Reducing alarm fatigue in two neonatal intensive care units through a quality improvement collaboration. Am Journal Perinatol, 35(13), 1311-1318. https://doi.org/10.1055/s-0038-1653945
Kretzschmer, S., Walker, M., Myers, J., Vogt, K., Massouda, J., Gottbrath, D., Pritchett, M., Stikes, R., & Logsdon, C. (2017). Nursing empowerment, workplace environment, and job satisfaction in nurses employed in an academic health science center. Journal for Nurses in Professional Development: 33(4) 196-202. https://doi.org/10.1097/NND.0000000000000363
Kutney-Lee, A., Germack, H., Hatfield, L., Kelly, S., Maguire, P., Dierkes, A., Del Geidice, M., & Aiken, L. (2016). Nurse engagement in shared governance and nurse outcomes. J Nurs Adm. 46(11), 605–612. Retrieved from https://www.jstor.org/stable/26813763
Lewandowska, K., Weisbrot, M., Cieloszyk, A., Mędrzycka-Dąbrowska, W., Krupa, S., & Ozga, D. (2020). Impact of alarm fatigue on the work of nurses in an intensive care environment-A systematic review. International Journal of Environmental Research and Public Health, 17(22), 8409. https://doi.org/10.3390/ijerph17228409
Mayhew, K. J., Lawrence, S. L., Squires, J. E., & Harrison, D. (2022). Elevated sound levels in the neonatal intensive care unit: What Is Causing the Problem? Advances in neonatal care: official journal of the National Association of Neonatal Nurses, 22(6), E207–E216. https://doi.org/10.1097/ANC.0000000000000996
Martin, B., Kaminski-Ozturk, N., O'Hara, C., & Smiley, R. (2023). Examining the impact of the COVID-19 pandemic on burnout and stress among U.S. nurses. Journal of Nursing Regulation, 14(1), 4–12. https://doi.org/10.1016/S2155-8256(23)00063-7
Montalvo, I., (2007) The National Database of Nursing Quality IndicatorsTM (NDNQI®) OJIN: The Online Journal of Issues in Nursing. 12 (3). Retrieved from https://ojin.nursingworld.org/table-of-contents/volume-12-2007/number-3-september-2007/nursing-quality-indicators/
Neuman, B. (1996). The neuman systems model in research and practice. Nursing Science Quarterly, 9(2), 67-70–70. Retrieved from https://doi-org.proxy.library.kent.edu/10.1177/08943184960090
Olender L, Capitulo, K., & Nelson, J. (2020). The impact of interprofessional shared governance and a caring professional practice model on staff's self-report of caring, workplace engagement, and workplace empowerment over time. J Nurse Adm. 50(1):52-58. https://doi.org/10.1097/nna.0000000000000839
“Optimizing the Nursing Workforce: Key Drivers of Intent to Stay for Newly Licensed and Experienced Nurses.” 2018 Nursing Special Report, Press Ganey Associates, Inc.
Porter-O'Grady, T. (2023). Council accountabilities. [Editorial]. Nurse Leader, 127. https://doi.org/10.1016/j.mnl.2023.01.003
Porter-O'Grady, T., & Malloch, K. (2011). Quantum leadership: Advancing information, transforming health care. (3rd ed). Jones & Bartlett.
Sendelbach, S., & Funk, M. (2013). Alarm fatigue: A patient safety concern. American Association of Critical-Care Nurses, 24(4), 378-386. https://doi.org/10.1097/NCI.0b013e3182a903f9
Simpson, K. R., & Lyndon, A. (2019). False alarms and overmonitoring: Major factors in alarm fatigue among labor nurses. Journal of Nursing Care Quality, 34(1), 66-72. https://doi.org/10.1097/NCQ.0000000000000335
Sowan, A. K., & Reed, C. C. (2017). A complex phenomenon in complex adaptive health care systems-alarm fatigue. JAMA Pediatrics, 171(6), 515–516. https://doi.org/10.1001/jamapediatrics.2016.5137
The Joint Commission (2015). Joint Commission national safety goals. Retrieved from https://www.masimo.com/siteassets/us/documents/pdf/2015_npsg_hap.pdf
Van Bogaert, P., Peremans, L., Diltour., N., Van heusden, D., Dilles, T., Van Rompaey, B., & Havens, D. (2016). Staff nurses’ perceptions and experiences about structural empowerment: A qualitative phenomenological study. PLOS ONE 11(4). https://doi.org/10.1371/journal.pone.0152654
van Pul, C., Mortel, H.P.M.E. v.d., Bogaart, J.J.L. v.d., Mohns, T., & Andriessen, P. (2015). Safe patient monitoring is challenging but still feasible in a neonatal intensive care unit with single family rooms. Acta Paediatrica 104(6), e247-e254. https://doi.org/10.1111/apa.12907
Walsh, M., Powers, D., & Fanaroff, J. (2015). The potential for harm from alarm fatigue in single-Room NICUs. [Editorial]. Foundation Acta Paediatrica 104(5), 436-437. https://doi.org/10.1111/apa.12953


