Collaboration between academic centers and healthcare systems/practices has demonstrated improved outcomes, fostered innovation, and increased nursing research. Although evidence for their importance has been established, all too often these academic-practice partnerships (APP) encounter hurdles that limit success. Lack of time, poor communication, and unclear leadership endorsement are often barriers to effective APPs. Utilizing the challenges of the COVID-19 pandemic, a successful APP was developed based on the Interprofessional Education Collaborative (IPEC) competencies. The IPEC framework addressed needs related to the COVID-19 pandemic and became the foundation for many future endeavors between a large children’s healthcare system and a university school of nursing. This APP demonstrated the appropriate capacity and organizational structure to provide simultaneous benefits to multiple parties while improving systemwide healthcare outcomes. This article outlines the development and implementation processes, subsequent evaluation, and implications for practice related to this highly successful partnership.
Key Words: Academic Practice Partnership, Interprofessional Education Collaborative Core Competencies, call center, advanced practice nurses, nursing education, practice readiness
Collaboration between academic centers and healthcare systems/practices have demonstrated improved outcomes for both student education and practice outcomes. It is well recognized that academic-practice partnerships (APPs) can create mutually beneficial collaborations that may result in improved patient outcomes, improved practice innovations, and increased research capacities (Baptiste et al., 2020; Roach & Hooke, 2018). However, the healthcare systems and academic institutions struggle to effectively create mutually beneficial partnerships. Lack of time, frail communication structures, and vague leadership endorsement contribute to the failure of APPs (Baptiste et al., 2021; Paton et al., 2020). This article outlines the development and implementation processes, subsequent evaluation, and implications for practice related to this highly successful partnership.
...healthcare systems and academic institutions struggle to effectively create mutually beneficial partnerships
Literature Review
The COVID-19 pandemic was not just a crisis in the healthcare of individuals within our population, it also impacted healthcare systems, providers, and health professional education (Office of Health Policy, 2022). Innovative approaches were needed to address patient care, while also addressing provider shortage and a lack of educational opportunities for nurses and providers (Costa & Friese, 2022).
Impact of COVID-19 on Children
Initially, it was thought that children and adolescents had escaped the impact of the COVID-19 pandemic. However, in late fall 2021, the Omicron variant emerged with a propensity for affecting children (Fleming-Dutra, 2022). This was due to rescinding stay-at-home orders and the return of face-to-face education. There was an “off season” surge in illness such as respiratory virus, parainfluenza, and rhinovirus that typically peak in the winter months (Cohen et al., 2021). In the last week of December 2021, the Omicron virus spurred a 35 percent increase in COVID-19 related pediatric hospitalizations (Hand, 2021; Centers for Disease Control and Prevention [CDC], 2023). The first week of January 2022 set a record high for pediatric COVID-19 hospitalizations (Jenco, 2022).
Initially, it was thought that children and adolescents had escaped the impact of the COVID-19 pandemic.
With this influx of illness, parents had many questions regarding COVID-19, and schools were refusing to allow students to return if they had been exposed. Parents sought information about COVID-19 symptoms, exposure, testing, results, and quarantine concerns. Additionally, as COVID-19 vaccines became more available, parents wanted to discuss pros and cons of the vaccine, locations to receive the vaccine, and vaccine reactions. The complexity of the patient conditions and everchanging guidelines were overwhelming to healthcare systems nationwide (Carey, 2021).
Challenges and Solutions for Pediatric Providers
At the same time, pediatric healthcare sites were facing record-high staffing shortages due to illness, quarantining of staff or family members, and a nationwide trend referred to as the “Great Resignation” (Parker & Horowitz, 2022). Pew research reported that the “Great Resignation” was fueled by worker dissatisfaction with pay, lack of opportunities for advancement, feeling disrespected at work, and childcare issues (Parker & Horowitz, 2022). The American Academy of Pediatrics (2021) issued a statement affirming that the COVID-19 pandemic resulted in an extraordinarily prolonged surge with multiple waves of illness, and unprecedented stresses on healthcare workers and support structures.
The complexity of the patient conditions and everchanging guidelines were overwhelming to healthcare systems nationwide.
To decrease the burden on the healthcare system, call centers were initiated to answer parent questions and address clinical issues. The goal was to decrease the number of patients coming to primary care practices, urgent care centers, and emergency room, and address the overwhelming call volume (Huss et al., 2021). Call centers protected employees from further disease spread while providing professional, early intervention to those in need (Cooling et al., 2021). Some call centers were used by hospitals to answer staff concerns regarding exposure, positive tests, and return to work, while other health systems opened call centers to answer community questions and serve as a resource for concerned parents of established patients.
Call centers protected employees from further disease spread while providing professional, early intervention to those in need
New and innovative approaches, such as APPs, were being considered to address the crisis. The goal of the APP was to pair healthcare systems with academic systems to provide students with competency-based education while improving healthcare outcomes system-wide (American Association of Colleges of Nursing [AACN], 2019). APPs provide collaboration through regular engagement and interaction in both clinical and academic settings utilizing joint committees, continuing education, and research forums (AACN, 2015). Key components must include mutual respect and trust, shared knowledge, and commitment to nurse-led collaborative models (AACN, 2012). APPs are further enhanced with a shared vision, buy-in, and transparent communication (Paton, 2022).
APPs provide collaboration through regular engagement and interaction in both clinical and academic settings...
Local Problem: Setting the Stage for an APP
Our local children’s hospital, like many other systems across the country, faced overwhelming issues resulting from the COVID-19 pandemic’s sudden impact on children. The children’s hospital system consisted of 266-hospital beds, three pediatric urgent care centers, 20-primary care clinics, and 6-specialty clinics. Providers in this system were responsible for not only patient care, but also for responding to questions and concerns within the community. Due to a shortage of staff, confusing messaging, and the overabundance of questions, the hospital system was having difficulty meeting the needs of concerned parents related to COVID-19.
...the hospital system was having difficulty meeting the needs of concerned parents related to COVID-19.
In cases where a child or family member had symptoms of illness or potential exposures, the child’s school required a provider clearance before the return to school. Despite the hospital staff’s best efforts to effectively communicate, primary care practice triage and staffing models were not able to easily manage and stay current with changing federal, state, and regional guidelines. The situation was further complicated by inconsistent regional school requirements and varied information regarding COVID-19 vaccination clinics. These culminating, and everchanging factors created a system-wide problem for this children’s health system.
At the same time, local school of nursing (SON) faculty, like so many schools across the country, were having difficulty finding clinical placements for students. Our SON programs included BSN, RN-BSN, MSN (family nurse practitioner, pediatric nurse practitioner, psychiatric nurse practitioner, clinical nurse specialists), and post-masters Doctor of Nursing Practice (DNP). These students were faced with clinical sites unable to precept them due to the increased risk of exposure to COVID-19, a shortage in staff, overwhelmed providers, and/or the closure of clinics. Even though the SON had utilized the children’s hospital for years for undergraduate clinical placements, there were no formal or routine relationships in place for advance practice nursing students.
These students were faced with clinical sites unable to precept them...
Due to the impact of the COVID-19 pandemic on both the hospital and the academic health center/SON, new strategies that would benefit both sites were needed. Though APPs had been explored for the purpose of providing educational sites for students, very little data indicated how APPs could be used to address a crisis that neither the hospital nor academic center could address alone. In addition, very little was known about how to best develop and implement an APP, especially during a pandemic. Our goal was to explore the possibility of developing and implementing an APP to meet this gap.
Purpose
The principal purpose of this project was to develop, implement, and evaluate an APP between a SON and a children’s hospital to provide a high-level COVID-19 Call Center (CCC). The overall goal was to understand factors that optimized the success and sustainability of the APP while accomplishing the following specific aims:
- Improve patient care and outcomes by providing a reliable repository for answering COVID-19 questions for parents.
- Decrease the burden on the healthcare system by alleviating the heavy telephone triage and unnecessary visits for primary care practices.
- Provide a robust practicum experience for graduate nursing students.
Developing the APP: Interprofessional Education Collaborative (IPEC)
It was expected that interprofessional teams would be able to successfully implement programs if all four competencies were addressed.
Since attempts at APPs had failed previously, a framework was sought to guide the development of the Academic Practice Partnership-COVID Call Center (APP-CCC). We determined that the Interprofessional Education Collaborative (IPEC) framework would best serve to guide the development of the APP-CCC. The IPEC core competencies are structured around four areas (see Figure 1): teams and teamwork; values and ethics; roles and responsibilities; and communication (IPEC, 2016). The Teams and Teamwork competency applies to relationship development based on the values and principles of team dynamics used to plan, deliver, and evaluate patient centered programs that are safe, timely, efficient, and equitable. The Values and Ethics competency suggests that individuals from other professions maintain a climate of mutual respect and shared values. The Roles and Responsibilities competency indicates that team members should have knowledge of their own role and those of the other professions they are working with. Finally, the Interprofessional Communication competency focuses on the team’s ability to communicate with patients, families, communities, and professions in a responsive and responsible manner that supports the team’s approach to maximizing health outcomes (IPEC, 2016). It was expected that interprofessional teams would be able to successfully implement programs if all four competencies were addressed.
Figure 1. IPEC Model with Call Center
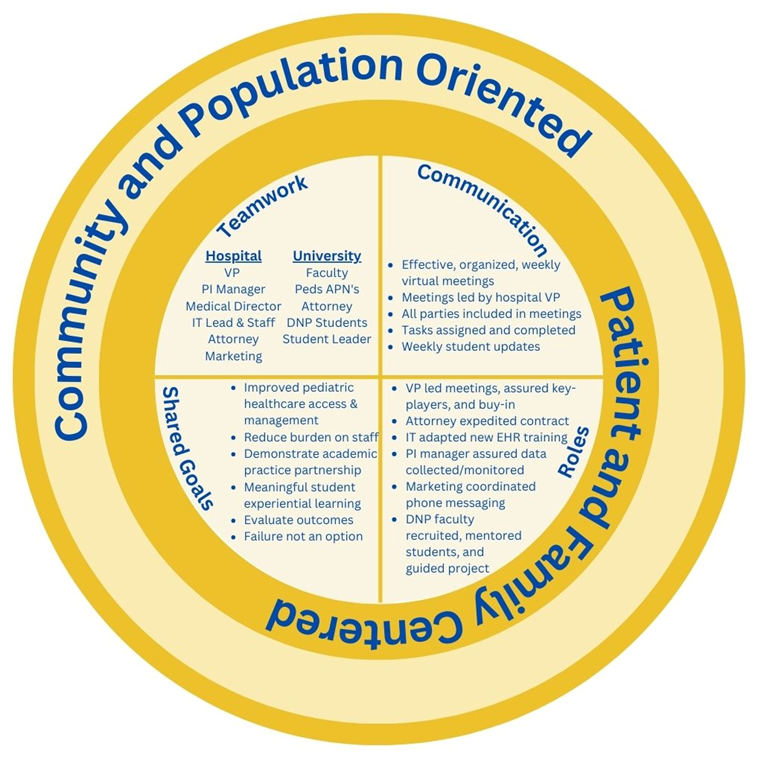
Teams and Teamwork
Creating the APP-CCC required a team of individuals who possessed the expertise and authority required to develop and implement the CCC within the hospital system and the SON academic structure. As such, leaders invested in the APP-CCC project who represented the children’s hospital and the SON formed a team to create a “win-win” solution to the impact of COVID-19 on the hospital system while addressing the SON need for student placement. Members from the children’s hospital consisted of 1) the Vice President of Physician Creating the APP-CCC required a team of individuals who possessed the expertise and authority required to develop and implement the CCC... Practice Management (VP-PPM), 2) the Performance Improvement Manager, 3) the Director for Information Services (IS), 4) Legal counsel, and 5) Director of Marketing and Public Relations. Members from the School of Nursing included 1) nursing faculty, specifically a pediatric nurse practitioner (PNP) and pediatric clinical nurse specialist (CNS) who also had clinical practices at the children’s hospital, 2) the university attorney, 3) two administrative university faculty, and 4) a DNP student. The CNS faculty member served as the leader from the SON, while the VP-PPM served as the lead from the hospital.
Values/Ethics and Shared Values
The APP-CCC team was established based on shared values related to patient care, healthcare workforce, and student education. The APP-CCC team was established based on shared values related to patient care, healthcare workforce, and student education. These shared values were used to connect those involved with the APP-CCC program under a common mission/vision. Specifically, the team members valued the importance of placing the interests of the patient and/or population at the center of the APP-CCC program. Each team member respected the values, roles/responsibilities, and expertise of those on the team.
The team hoped to decrease cost and burden to the healthcare system, while meeting the students’ need for real world experiential opportunities that would meet the new AACN Essentials (AACN, 2021). Both the university and healthcare system realized that families were not able to access quick and reliable information. As a result, children were inappropriately receiving care in primary care practices and urgent care centers, while others were requiring rapid admissions to the intensive care unit due to limited access to primary care services.
Both the university and healthcare system realized that families were not able to access quick and reliable information.
Roles/Responsibilities
To quickly accomplish the development and implementation of the CCC, there was a need to establish a team that possessed the expertise and leverage to accomplish needed tasks. There was an immediate need to break down barriers within organizations that were often slow to change. As the process proceeded, the APP-CCC team members added additional professionals with expertise to complement the existing team members while addressing gaps in the roles of the current team members.
The professionals involved in the team were responsible for:
- developing the APP-CCC,
- implementing the technology,
- assuring legal and regulatory issues were addressed,
- determining workflow,
- training students,
- scheduling student experiences, and
- assuring that changing guidelines were being met.
There was an immediate need to break down barriers within organizations that were often slow to change.
The CNS leader from the SON and the VP PPM were responsible to assemble the APP-CCC and ensure that it comprised the expertise needed to move the project forward. As such, members of the team moved in and out of meetings based on skills and responsibilities. Legal representatives from both the university and the healthcare system were assembled to ensure a Memorandum of Understanding (MOU) was developed. They also ensured that state rules and regulations and the emergency waivers for healthcare were followed.
The Director for Information Services (IS) was instrumental in determining how to meet the technology needs of the program as well as implementing the needed platforms (i.e., the tele-communication system and the third-party triage system) and ensuring privacy and confidentiality. IS also provided students with access to electronic health records (EHR) from their homes. The Director of Marketing developed the APP-CCC messaging and branding for the practices and community. The Performance Improvement Manager maintained the call volume and was able to assist the team to predictstaffing needs for the APP-CCC.
...members of the team moved in and out of meetings based on skills and responsibilities.
Nursing school faculty members provided student oversight, guided their training, and provided support for student leaders and students who manned the APP-CCC. In addition, SON faculty provided the pediatric expertise and supervision necessary to accomplish the task. The lead DNP student served as liaison between the meetings and the students, aided in student training, and scheduled students to provide the APP-CCC services.
Interprofessional Communication
The APP-CCC team did not have a previous history of working together or an established communication pattern. For effective communication, the APP-CCC team needed to establish a mechanism to communicate with each other and with patients at a distance, a schedule/system for meetings, and equipment to support communication needs.
The APP-CCC team did not have a previous history of working together or an established communication pattern.
As a result of COVID-19 restrictions and the physical distance between all team members, meetings were held virtually. Meetings were held weekly and ad hoc at the start of the day (7 am) with respect to each team member’s responsibilities. The ongoing work of each team member was reviewed at the start of each meeting; assignments were given at the end trusting that participants would complete their assigned work prior to the next meeting. Meetings were led by the VP-PPM as this member had working relationships with team members from both the hospital system and the SON.
To establish a mechanism for communication with patients and EHR documentation, the Director of IS provided access and training to the two main communication platforms utilized by the healthcare system (Cisco Jabber® and EHR). The third communication platform utilized was a third-party triage system for standardized triage documentation (TriageLogic®). Students and faculty received additional training in this system.
The team of students and faculty was updated weekly on changes in procedural processes or changes in care guidelines. They were updated via an emailed newsletter composed by the lead DNP student with input from the SON and the hospital team members. The lead DNP student, SON and hospital team members met virtually at least weekly to discuss progress, concerns, and to review team resources. Resources were updated regularly to maintain current recommendations and practice given frequently changing COVID-19 protocols. To ensure ease of access, all documents were maintained on a Cloud-based platform made available to all team members.
Resources were updated regularly to maintain current recommendations and practice given frequently changing COVID-19 protocols
Implementation of APP-CCC
Students
Twenty-six graduate nursing students, including six pediatric nurse practitioner (PNP) students, twenty DNP students, and four university faculty were involved in developing, implementing, and evaluating the APP-CCC. The call center was initially envisioned as a potential opportunity for undergraduate, prelicensure students. As the project planning began, and COVID-19 progressed, it was deemed that the call center would be more appropriate for nurse practitioner or post-master’s DNP students for several reasons: the higher acuity of patients, higher stress level of parents, and continually evolving changes with the COVID-19 protocols. As some DNP students who were licensed nurse practitioners (NP) were located out of state, and the APP-CCC occurred during the COVID-19 waivers, the Commonwealth of Virginia permitted practitioners with an active license issued by another state to provide telehealth services in Virginia.
The program was organized allowing students to achieve needed practicum experiences related to their academic track.
The program was organized allowing students to achieve needed practicum experiences related to their academic track. They also benefited from experiences that included mentoring by DNP leadership, participating in agency administrative meetings, and communicating with interprofessional teams for a common goal. These students served as active team members in developing, implementing, and evaluating the APP-CCC program.
Students in the PNP program benefitted from opportunities to interact with families while applying their advanced practice knowledge and skills for this high-level telephone triage. Students were able to synthesize and then apply changing concepts in the fields of epidemiology and infectious disease. Additionally, this APP-CCC provided several opportunities to utilize counseling skills needed to de-escalate the anxiety of parents. The design of the APP-CCC allowed budding NP students to learn, adapt, and gain confidence in these skills.
Students were able to synthesize and then apply changing concepts in the fields of epidemiology and infectious disease.
All students involved in the program learned about the development and implementation of a call center and how it felt to provide the APP-CCC services. Furthermore, they learned the importance of evaluating outcomes and using this data to refine the program. An even greater outcome was that the SON and the hospital system learned to work collaboratively to benefit both organizations, as well as the targeted patient population.
Training of Students
Students required training in 1) responding to potential questions raised by the parents, 2) utilizing the tele-communication system (Jabber®) to converse with parents, 3) using the third-party triage system (TriageLogic®), and 4) documenting the visit through the EHR. A major obstacle was that the hospital system historically only completed training using a face-to-face format. Given the COVID-19 pandemic and the fact that the students were providing services from all over the country, it was necessary for the hospital agency to In addition to formal training, students received weekly COVID-19 content specific training and systems updates. pivot to provide virtual training and utilize an electronic interactive training platform to accommodate the needs of students and faculty. Remaining areas of training were completed by synchronous, recorded, teleconference meetings, and the creation of shared drives for all resource documents and recorded sessions. Agency contact leads for each system, along with a DNP student and faculty lead, were regularly available during APP-CCC hours for troubleshooting.
In addition to formal training, students received weekly COVID-19 content specific training and systems updates. These sessions were led by the medical director and telehealth director for the outpatient practices at the health system, and then assigned to DNP students as lead internal “champions.” Additional DNP lead students were assigned as the “champion” and served as a resource for any EHR related questions.
ACC-CCC Program Delivery
The APP-CCC technical infrastructure and fiscal resources were supported by the hospital system. The APP-CCC was initially operated five days a week from 8am to 4pm. After the soft launch, and within a week of the full launch, a need arose for the APP-CCC to assist with the inundated pediatric urgent care centers also associated with the hospital system. It was at this time that the APP-CCC was then extended to seven days a week.
The APP-CCC technical infrastructure and fiscal resources were supported by the hospital system.
Calls to the APP-CCC were initiated by patients/families who contacted either the urgent care or primary care offices affiliated with the children’s hospital. For urgent care locations, staff forwarded calls to the APP-CCC, while at the primary care offices, families were self-directed via an automated prompt for all COVID-19 related information. The APP-CCC then received the call and triage was completed utilizing a combination of resources that included triage software (Barton-Schmidt), local department of health guidelines, CDC guidelines, and health system guidelines.
Students were able to provide testing and vaccine locations or test results (completed either at primary care practice or urgent care center). Additionally, students provided advice regarding COVID-19 symptoms, vaccine related symptoms, and exposure questions (e.g., isolation, quarantine). During the calls, it was sometimes determined that patient would need to be seen. If the need was acute, the family was referred to an appropriate facility (e.g., urgent care center or emergency room). If non-acute, the family was transferred to the PCP practice with a warm handoff to office staff to schedule the appointment. All documentation of the interaction was placed in the patient EHR and the primary care provider on record received a copy of the call.
Impact of APP-CCC
It was important to obtain data on the program while it was occurring to address issues and refine its implementation. Data were collected on the overall impact of the APP-CCC program to leverage future APPs.
Patient/Family Member
To determine the success of the APP-CCC and refine the program, patient and family data were gathered by the hospital system via the EHR and patient logs. Data points such as insurance type, and originating pediatric practice were monitored. The health system also examined call types which were sorted into seven categories described below with frequencies.
It was important to obtain data on the program while it was occurring to address issues and refine its implementation.
There were 868 calls received during the 9-week period of the APP-CCC. Data showed that patients with Tricare insurance represented 14%; patients with Medicaid insurance represented 38%; and patients with commercial insurance represented 48%. This distribution resembled the demographics represented in the primary care practices being serviced. Frequencies for calls reflected the seven created categories: COVID-19-diagnosed or suspected (n = 203); test results (n = 192); vaccine information (n = 167); exposure questions (n = 142); testing questions (n = 79); immunization reactions (n = 12); and not applicable to call center and rerouted to office (n = 23).
Clinical/Program
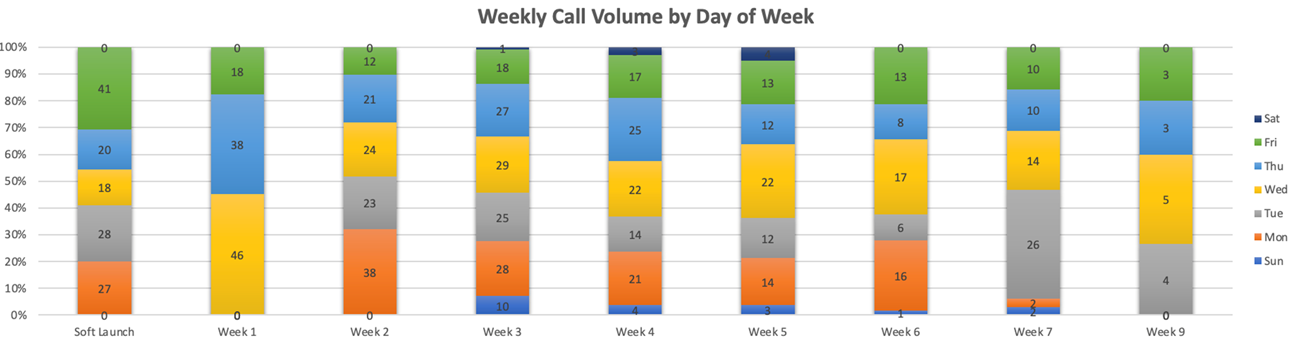
Data on the call center utilization were tracked by week, day, and hour. Primary care providers were surveyed regarding overall satisfaction with the CCC and perceived impact on the practice call volume. A focus group with primary care providers and the call center team leaders was conducted to gather narrative based data.
Data on the call center utilization were tracked by week, day, and hour.
The call volume was heaviest during the middle of the week, with Wednesdays, Tuesdays, and Thursdays having a total volume of 197, 188, and 164 respectively (Figure 2). Fairly even volumes were on Mondays (n = 146) and Fridays (n = 145). Saturday and Sundays were much lighter with volumes of 8 and 20, respectively. The heaviest weekly call volume of 138 calls was experienced during the third week. These data points were reviewed weekly by the DNP lead and utilized to ensure proper staffing of the CCC.
Figure 2. Weekly Call Volume
Seventy-one percent of the providers noticed a decrease in triage call volume at their practices. Of note during the focus group, some providers not initially included in the launch of the call center program requested to be included. Ultimately, the CCC allowed clinic staff to maintain daily operations, ensuring care to their current patients, without being overwhelmed or pulled from the floor to answer patient calls.
Students
Student data were collected and maintained by the lead faculty and lead DNP student. Demographic information, along with student type (e.g., PNP, PCNS, DNP) and licensure state was collected. As the semester progressed, students were also surveyed about their call center experience and how they felt they met specific outcomes, framed around the AACN (2021) Essentials.
A total of 26 students participated in the ccc, 20 were doctoral students of which 18 had advanced practice licensure. The remainder of the students were DNP nurse executive students or PNP students, all of whom were licensed RNs. Of the students that participated in the call center, 20 of the students completed the post-CCC survey. Those completing the survey were all female, with a mean age of 39.15 (SD=8.17), and 50% were non-white. Students were asked how the experience improved their abilities and how the experienced prepared them for various situations and settings, framed around the Essentials (AACN, 2021). The overall rating of these questions regarding the call center experience was x = 4.25 (SD = 1.07) on a five-point Likert scale, with strongly disagree = 1 and strongly agree = 5.
Students were asked how the experience improved their abilities and how the experienced prepared them for various situations and settings...
From this APP-CCC model, two DNP projects were developed. The first project assessed patient and family satisfaction and cost savings. The second project expanded the impact of the APP by assessing the asthma outcomes (via chart review) of children seen in the hospital clinics to identify gaps. The results of this project were used to launch a program where care was provided to children with asthma by APRN students from the SON mobile health clinic. The students connected with specialists at the children’s hospital via telehealth to co-manage the care of these students.
Discussion
There had been no APP between the healthcare system and the academic institution prior to the implementation of the APP-CCC. As such, one primary goal for both organizations was to establish an APP that would be self-sustaining and utilized for other future needs identified by both organizations. It was important to collect data on the impact of the program to leverage further collaborative programs. Distribution of data from APPs formalizes the recognition of completed initiatives as significant contributions to organizational business and nursing service lines and demonstrates the value of the APPs (Diegel-Vaceka & Yonkaitis, 2023).
It was important to collect data on the impact of the program to leverage further collaborative programs.
The primary concern at the onset of theCOVID-19 pandemic was the overall health of our population. However, throughout the pandemic, it became apparent that there were other significant crises surrounding COVID-19 including the inadequate infrastructure of healthcare systems, the multifaceted burden of the pandemic on healthcare providers, and the strain on the clinical education of future healthcare providers. Through the activation of an APP between a children’s hospital and SON, solutions were implemented, and problems mitigated during a crisis that allowed for success in both organizations.
The APP was able to provide resources and a solution to the COVID-19 crisis that many primary care practices faced regarding staffing shortages. By applying the IPEC competencies of open communication; common values for our populations and families served; and understanding of each other’s roles; along with teamwork, the APP-CCC team was able to strategize a solution to alleviate the burden on the primary care practices. We were able to decrease call volume burden for the practices and to triage the sometimes-complicated questions of COVID-19 with experienced RNs and NPs. The higher level of telephone triage also alleviated further burden on providers to follow up with in-office triage. Furthermore, the goal of the APP was to provide students with competency-based education within clinical sites. This was achieved through this APP-CCC program.
Implications for Practice/Conclusion
It is important to emphasize the key components in this APP that was nurse-led. Strategic relationships, interprofessional understanding, and trust were fundamental factors to the successful launching of this call center. Additionally, key strategies, such as weekly meetings with assigned task(s) at the end, a soft launch opening, and identification of champion leaders with the ability to mobilize individuals were also vital to the overall success. Transparent buy-in from healthcare leadership was also a vital component.
Overall, an APP has the capacity and organization to provide simultaneous benefits to multiple parties while improving healthcare outcomes system wide. This APP demonstrated improved patient care access and decreased burden on healthcare systems. In addition to this achievement, new opportunities for DNP student research, hospital system quality improvement projects, and multiple faculty research opportunities have also resulted from this partnership. A nurse-led interprofessional APP, framed around the IPEC model, was able to successfully mitigate a crisis in healthcare. Furthermore, this APP supported a project that positioned a deliverable, ready to use framework to inform the next public health crisis.
Authors
Tina Gustin DNP, CNS, RN
Email: tgustin@odu.edu
Tina Gustin has over 35-years of advanced practice nursing experience. She received an undergraduate degree from the Medical College of Virginia, which is now Virginia Commonwealth University. She received a master’s degree as a Pediatric Clinical Nurse Specialist from the University of Virginia, and a Doctor of Nursing Practice degree from Old Dominion University. She is currently an Associate Professor at Old Dominion University School of Nursing where she teaches in the Doctor of Nursing Practice Program. Dr. Gustin is the director of the university Center for Telehealth Innovation, Education, and Research (C-TIER). The center serves as a national telehealth learning hub and research center. In practice, Dr. Gustin is the clinical manager for the Pediatric Telehealth program at Children’s Hospital of the King’s Daughters (CHKD) in Norfolk Virginia. She has been responsible for the development of the telehealth program and assuring clinical competence of the telehealth providers. Additionally, Dr. Gustin is the Virginia state telehealth coordinator for the Virginia Mental Health Access Program and serves on the Center for Telehealth and eHealth Law (CTeL) Advisory Board, where she chairs the Telehealth Education Task for CTeL.
Jessica Parrott, DNP, CPNP, CNE
Email: jmparrot@odu.edu
Jessica Parrott received bachelor’s in nursing, master’s in nursing and doctorate in nursing practice degrees from Old Dominion University (ODU). Dr. Parrott completed a master’s in nursing with a focus on the pediatric nurse practitioner role and additionally earned a postgraduate certificate in nursing education. She is dually certified as a primary care pediatric nurse practitioner and nurse educator. Dr. Parrott has been a nurse practitioner for 20 years in pediatric primary care and pediatric urgent care settings, and a nurse educator for over 10 years in both undergraduate and graduate nursing. Dr. Parrott is currently an Assistant Professor at ODU School of Nursing and practices clinically with Children's Hospital of the King's Daughters (CHKD) Division of Urgent Care where she is a member of the interprofessional Quality Improvement Committee. Additionally, she is adjunct faculty for Eastern Virginia Medical School (EVMS). Dr. Parrott currently serves on the National Association of Pediatric Nurse Practitioners Professional Issues Committee.
Jalana McCasland, BA, MPA, MA, Ed, FACHE
Email: jalanmccasland@gmail.com
Jalana McCasland is Vice President of Physician Practice Management at Children’s Hospital of the King’s Daughter’s (CHKD) and over sees operations for Children's Medical Group (CMG), Children's Surgical Specialty Group (CSSG) and Children's Specialty Group (CSG) practice management. McCasland earned a Bachelor of Arts in Politics and Government from the University of Texas at Dallas, a Master of Public Administration from the University of Texas at Tyler, and a Master of Organizational Leadership and Learning from George Washington University. McCasland has over 20 years of healthcare experience with the majority of it in the ambulatory setting, including practice management, call centers, telemedicine, managed care contracting and physician and regional outreach. McCasland is the Chair of the Virginia Beach Social Services Advisory Board and is a fellow in the American College of Healthcare Executives.
Carolyn Rutledge, PhD, FNP-BC, FAAN
Email: crutledg@odu.edu
Carolyn Rutledge is an Eminent Scholar at Old Dominion University (ODU) where she founded the Doctor of Nursing Practice program. She has published over 70 articles and served as investigator on 33 grants totaling over $27 million focusing on methods to care for underserved populations. She led development of the National Organization of Nurse Practitioner Faculty (NONPF) position paper on educating nurse practitioners in telehealth and published the book, “Telehealth Essentials for Advanced Practice Nursing.” She is Co-Director of the Center for Telehealth Innovation, Education, and Research (C-TIER). Dr. Rutledge received the 2014 SCHEV Outstanding Faculty Award, the highest honor provided to faculty in Virginia.
References
American Academy of Pediatrics (2021, September 27.) Caring for patients in inpatient and outpatient settings during episodes of surge. Retrieved from: https://www.aap.org/en/pages/2019-novel-coronovirus-covid-19-infections/clinical-guidance/caring-for-patients-in-outpatient-settings-during-episodes-of-surge
American Association of Colleges of Nursing (2021) The Essentials: Core competencies for professional nursing education. Retrieved from: https://www.aacnnursing.org./Portals/0/PDFs/Publications/Essentials-2021.pdf
American Association of Colleges of Nursing. (2019). AACN’s vision for academic nursing. Retrieved from: https://www.aacnnursing.org/Portals/42/News/White-Papers/Vision-Academic-Nursing.pdf
American Association of Colleges of Nursing (2015). Re-envisioning the clinical education of advanced practice registered nurses. Retrieved from: https://www.aacnnursing.org/Portals/42/News/White-Papers/APRNClinical-Education.pdf
American Association of Colleges of Nursing (2012). AACN-AONE task force on academic practice partnerships: Guiding principles. Retrieved from: https://www.aacnnursing.org/Academic-Practice-Partnerships/The-Guiding-Principles
Baptiste, D., Whalen, M. & Goodwin, M. (2021). Approaches for establishing and sustain clinical academic partnerships: A discussive review. Journal of Clinical Nursing, 31(3-4), 329-334. https://doi.org/10.1111/jocn.15830
Carey, J., (2021, September 14). Virginia doctor says pediatricians struggling to keep up with covid testing demand. NBC Washington. Retrieved from: https://www.nbcwashington.com/news/local/virginia-doctor-says-pediatricians-struggling-to-keep-up-with-covid-testing-demand/2801167/
Centers for Disease Control and Prevention. (2023, January 22). COVID data tracker. Atlanta, GA: US Department of Health and Human Services, CDC. Retrieved from: https://covid.cdc.gov/covid-data-tracker
Cohen, R., Ashman, M. Taha, M., Varon, E., Angoulvant, F., Levy, C., Rybak, A., Ouldali, N., Guiso, N. & Grimprel, E. (2021). Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infectious Diseases Now, 51(5), 418-423. https://doi.org/10.1016/j.idnow.2021.05.004.
Cooling, M. Klein, C., Pierce, L., Delinski, N., Lots, A., and Vozenilek, J. (2021), Access to care: end-to-end digital response for COVID-19 care delivery. The Journal of Nurse Practitioners, 18(2), 232–235. https://doi.org/10.1016/j.nurpra.2021.09.011
Costa, D., & Friese, C. (2022). Policy strategies for addressing current threats to the U.S. nursing workforce. The New England Journal of Medicine, 386(26), 2454-2456.
Diegel-Vaceka, L., & Yonkaitis, C. F. (2022). A novel approach to fostering academic-practice partnerships: The DNP project executive summary. Journal of Nursing Education, 61(3), 156–158. https://doi-org.proxy.lib.odu.edu/10.3928/01484834-20211128-03
Fleming-Dutra, K. (2022, June 17). COVID-19 epidemiology in children ages 6 months–4 years. National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention. Retrieved from: https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2022-06-17-18/02-covid-fleming-dutra-508.pdf
Hand, M. (2021, December 28). COVID hospitalizations among children up in VA as omicron spreads. The Patch. Retrieved from: https://patch.com/virginia/fallschurch/covid-hospitalizations-among-children-va-omicron-spreads
Huss, G., Magendie, C., Pettoello-Mantovani, M., & Jaeger-Roman, E. (2021). implications of the covid-19 pandemic for pediatric primary care practice in Europe. The Journal of Pediatrics, 233, 290–291.e2. https://doi.org/10.1016/j.jpeds.2021.03.004
Interprofessional Education Collaborative. (2016). Core competencies for interprofessional collaborative practice: 2016 update. Washington, D.C.: Interprofessional Education Collaborative.
Jenco, M. (2022, January 7). CDC releases updated school guidance; pediatric COVID hospitalizations hit record high. American Academy of Pediatrics News. Retrieved from: https://publications.aap.org/aapnews/news/19038
Office of Health Policy. (2022, May). Impact of the covid-19 pandemic on the hospital and outpatient clinician workforce. (HP-2022-13). Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Retrieved from: https://aspe.hhs.gov/sites/default/files/documents/9cc72124abd9ea25d58a22c7692dccb6/aspe-covid-workforce-report
Parker, K., & Horowitz, J., (2022, March 9). Majority of workers who quit a job in 2021 cite low pay, no opportunities for advancement, feeling disrespected. Pew Research Center. Retrieved from: https://www.pewresearch.org/fact-tank/2022/03/09/majority-of-workers-who-quit-a-job-in-2021-cite-low-pay-no-opportunities-for-advancement-feeling-disrespected/
Paton, E. A., Wicks, M., Rhodes, L. N., Key, C. T., Day, S. W., Webb, S., & Likes, W. (2022). Journey to a new era: An innovative academic-practice partnership. Journal of Professional Nursing, 40, 84–88. https://doi.org/10.1016/j.profnurs.2022.03.006
Roach, A., & Hooke, S. (2019). An academic-practice partnership: fostering collaboration and improving care across settings. Nurse Educator, 44(2), 98–101. https://doi.org/10.1097/NNE.0000000000000557


