Negative health impacts exist for individuals who identify as lesbian, gay, bisexual, transgender, or something other than heterosexual are critical. Nurses are on the front lines of delivering holistic patient care to everyone, and their potential biases regarding this vulnerable population may negatively affect care. The study used scores from two tests designed to measure implicit bias in individuals towards sexual and gender minorities (SGM). A retrospective design with secondary data from Project Implicit was conducted using the Transgender (2020) and Sexuality (2006 to 2020) Implicit Association Tests (IATs). We compared mean Transgender IAT scores of nurses to other health-related professions (n = 53,586) and investigated differences between nurses’ Transgender IAT scores and self-identified explicit attitudes (n = 1558). A time-series of nurses’ Sexuality IAT scores was also explored (N = 25,791). Our study findings demonstrated that nurses held the strongest implicit preference for cisgender people compared to other occupational groups. No significant difference was found between nurses’ implicit and explicit preferences. Nurses’ implicit attitudes about sexual orientation have trended toward less biased scores. Comprehensive nursing education and implementation of nursing practices that promote health and well-being for sexual and gender minority patients are needed to reduce biases and continue this trend.
Key Words: implicit bias, bias, unconscious bias, implicit attitudes, IAT, implicit association to describe test, sexual and gender minorities, SGM, transgender, trans, lesbian, gay, LGBTQ, LGBTQ+, LGBT, nursing, nurses
According to Gallup, as of February 2022, the proportion of Americans who identify as lesbian, gay, bisexual, transgender, or something other than heterosexual is 7.1% (Jones, 2022). The term “sexual and gender minorities” (SGM) is currently the preferred inclusive term to describe the diverse population of individuals who are not exclusively heterosexual, do not identify with their sex assigned at birth, or otherwise do not conform to traditional binary gender roles (e.g., people who identify as lesbian, gay, bisexual, transgender, queer/questioning, LGBTQ, or other variations of this acronym) (National Institutes of Health, 2015). The SGM community includes, but is not limited to, sexual minorities, generally individuals with same-sex attraction who identify as lesbian, gay, and bisexual; and gender minorities, typically transgender and gender non-conforming/non-binary individuals (Ayhan et al., 2020).
Stigmatization, fear, hatred, homophobia, transphobia, and bias of providers are among the reasons believed to contribute to inequities in healthcare for SGM individuals.Negative health impacts for SGM individuals are well-documented, including vulnerability to addiction and mental health disorders (Meyer, 2003; Parent et al., 2019; Sinha, 2008). Stigmatization, fear, hatred, homophobia, transphobia, and bias of providers are among the reasons believed to contribute to inequities in healthcare for SGM individuals (Ayhan et al., 2020; Divan et al., 2016). Sexual and gender minority individuals may be reluctant to seek healthcare or may postpone treatment because of fear of discriminatory practices (Institute of Medicine, 2011). Thirty-three percent (33%) of the 2015 United States (U.S.) Transgender Survey respondents reported at least one negative interaction with a healthcare provider, such as verbal abuse or outright refusal to provide care, and 23% did not seek care during the year prior to completing the survey due to the fear of being mistreated (James et al., 2016).
Sexual and gender minority individuals may be reluctant to seek healthcare or may postpone treatment because of fear of discriminatory practices.
Nurses are on the front lines of delivering holistic SGM patient care. However, nurses’ biases regarding this vulnerable population may negatively affect care, contributing to less time spent with patients and inadequate assessment, treatment, and follow-up (Narayan, 2019). Explicit biases or attitudes are outwardly acknowledged stereotypes, beliefs, and perceptions that can be reported (Manns-James, 2015). Biases can also be implicit, which are outside of conscious awareness and often conflict with explicitly stated beliefs (Chapman et al., 2013). Implicit bias shapes a person’s behaviors and attitudes through automatic, rapid assimilation of patterns, helping people act instinctively in unfamiliar or unsafe situations (Edgoose et al., 2019). However, it may also increase the possibility of adverse treatment and discrimination (Edgoose et al., 2019).
Studies that have considered nurses’ implicit attitudes regarding the SGM population are lacking. Little is known specifically about nurses’ implicit biases and subsequent effects on patient care in these populations (Manns-James, 2015). In our literature review, we identified only one relevant published study. Sabin et al. (2015) compared healthcare workers’ Implicit Association Test (IAT) results from the Sexuality IAT globally available through Project Implicit. The Sexuality IAT collects information related to participant views on heterosexuals compared to lesbian and gay individuals. Groups included medical doctors, other diagnostic and treating providers, nurses, mental health providers, and non-providers. Of the four provider groups, nurses had the strongest implicit preferences for heterosexuals versus lesbian and gay individuals. The study, however, did not address providers’ attitudes related to bisexual and transgender individuals and was not focused specifically on U.S. participants.
Of the four provider groups, nurses had the strongest implicit preferences for heterosexuals versus lesbian and gay individuals.
Given the lack of studies that specifically focus on nurses and the primary emphasis on nurses’ explicit attitudes, we sought to further investigate nurses’ implicit attitudes using two separate IAT tests: the Transgender (bias towards transgender individuals) and the Sexuality (bias towards gay and lesbian individuals) IATs. Using data from the Transgender IAT as well as the Sexuality IAT, we formulated three questions:
Q1: Is there a difference between U.S. nurses’ Transgender IAT scores and those of other health related occupational groups?
Q2: Does a significant difference exist between nurses’ Transgender IAT scores and their self-reported explicit attitudes?
Q3: Have nurses’ scores on the Sexuality IAT changed over time?
Methods
We evaluated retrospective secondary data from Project Implicit, a non-profit organization that collects data on implicit biases (Project Implicit, 2011a). Datasets were retrieved in September 2021. Globally, individuals access Project Implicit online to complete one of 14 different IATs on social attitude topics, such as age, race, weight, religion, transgender (i.e., gender identity), and sexuality (i.e., sexual orientation) (Project Implicit, 2011c). In addition to completing the IAT, respondents can voluntarily answer questions related to personal demographics and explicit attitudes about the selected subject, which generally have Likert-scale response options.
Measures
Measure of Implicit Attitudes. The IAT has been widely used for over two decades to collect information on implicit biases (Project Implicit, 2011a). Designed to help measure attitudes and beliefs that people may be unwilling or unable to report, the test measures the strength of relative associations between concepts (e.g., lesbian/gay or heterosexual) and evaluations or stereotypes (such as good or bad) (Greenwald et al., 2015; Project Implicit, 2011b). For example, in the Transgender IAT, participants watch a brief tutorial of the photos used in the test to identify who is transgender and who is cisgender. Then participants are shown a series of photos and asked to differentiate between cisgender and transgender celebrities. Further into the test, participants are asked to make associations. They are asked to press “E” when a photo of a transgender person or a good word (i.e., “friend”) appears, and to press “I” when a photo of a cisgender person or a bad word (i.e., “dirty”) appears. Then the test switches the associations (i.e., transgender with bad words and cisgender with good words). Figure 1 offers an example screenshot. The Sexuality IAT operates similarly and requires participants to distinguish between words and symbols representing lesbian/gay and heterosexual people (See screenshot example in Figure 2).
Figure 1. Example Screenshot: Transgender IAT
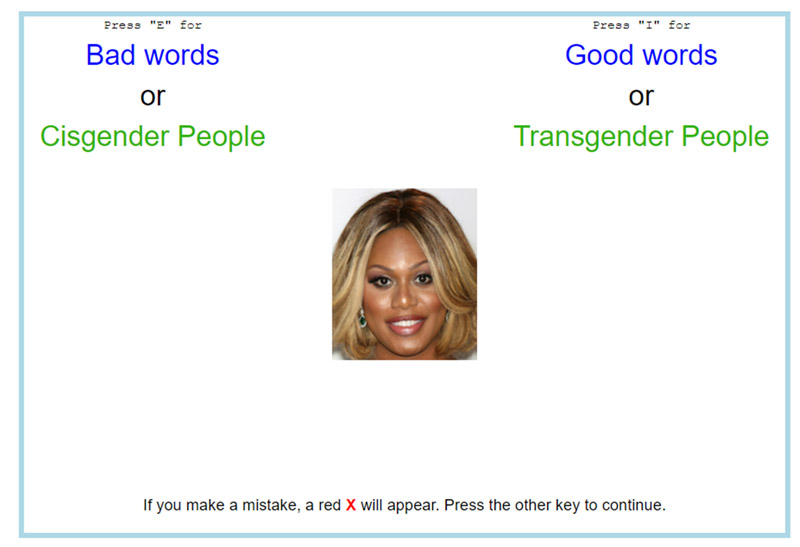
Note: Screenshot reprinted with permission from Project Implicit.
Figure 2. Example Screenshot: Sexuality IAT
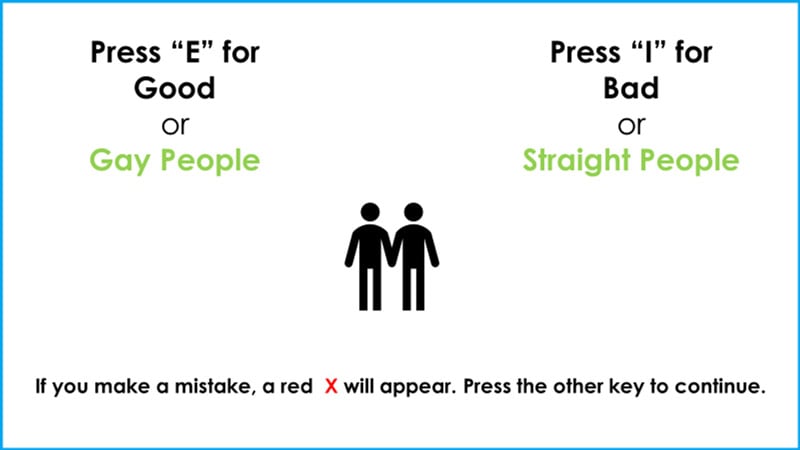
Note: Screenshot reprinted with permission from Project Implicit.
IAT scores are computed using respondents’ performance speeds for two classification tasks (Greenwald et al., 2003) and are based on the premise that choosing responses is easier when closely related items share the same response key (Project Implicit, 2011b). Participants who respond more quickly to a pair of associations (e.g., “heterosexual + good” or “gay + bad”) are considered to have stronger implicit attitudes toward that group (Project Implicit, 2011b). Results are reported as overall IAT D scores between -2 and 2 (Greenwald et al., 2003). Interpretation of the scores is based on ranges (Epifania et al., 2020). For example, Transgender IAT scores between -0.15 and 0.15 are interpreted as no preference for either transgender or cisgender. Scores between -0.65 and -2 are interpreted as a strong preference for cisgender individuals (see Table 1).
Table 1. Implicit Bias Ranges and Recoding of Nurses’ Explicit Bias
|
|
|
Nurses’ Explicit Bias |
||
|---|---|---|---|---|
|
Interpretation |
IAT Range |
Explicit Self Evaluation |
Recoded Self Evaluation* |
n(%) |
|
Strongly Prefer Transgender over cisgender |
-2 to -0.65 |
1 |
-1.325 |
8 (0.5%) |
|
Moderately Prefer Transgender over cisgender |
>-0.65 to ≤-0.35 |
2 |
-0.5 |
13 (0.8%) |
|
Slightly Prefer Transgender over cisgender |
>-0.35 to ≤-0.15 |
3 |
-0.25 |
36 (2.3%) |
|
No Preference between transgender and cisgender |
>-0.15 to <0.15 |
4 |
0 |
961 (61.7%) |
|
Slightly Prefer Cisgender over Transgender |
≥0.15 to <0.35 |
5 |
0.25 |
285 (18.3%) |
|
Moderately Prefer Cisgender over Transgender |
≥0.35 to <0.65 |
6 |
0.5 |
148 (9.5%) |
|
Strongly Prefer Cisgender over Transgender |
≥0.65 to 2 |
7 |
1.325 |
107 (6.9%) |
*Recoded values are the midpoint of the IAT range.
This research supported and validated that the IAT assesses personal attitudes rather than cultural or group attitudes.
Following the creation of the IAT in 1998, Greenwald and Nosek (2001) reported good reliability. Greenwald et al. (2009) again found moderate predictive validity of the test (r = .274), which was subsequently verified six years later (Greenwald et al., 2015). Greater IAT predictive validity versus self-reported measures has been substantiated (Manns-James, 2015). Manns-James (2015) described construct validity testing using known group comparisons, factor analysis, hypothesis testing, and multi-trait multi-method strategies. This research supported and validated that the IAT assesses personal attitudes rather than cultural or group attitudes (Manns-James, 2015). Consistently high Cronbach’s alpha scores were also reported, averaging 0.8 with an overall range of 0.7 – 0.9 (Manns-James, 2015).
Measure of Explicit Attitudes Towards Transgender Individuals. In addition to evaluating implicit biases, Project Implicit also askedparticipants to self-describe their preferences regarding transgender individuals on a Likert scale from one to seven, with one indicating a strong preference for transgender individuals and seven indicating a strong preference for cisgender individuals. A score of four indicated no preference. We sought to determine the level of self-awareness that nurses have by comparing these explicit bias self-evaluations with their implicit transgender IAT score evaluations. To make a valid comparison, the explicit scores were recoded to align with IAT scores by using the midpoint of the IAT interpretation range corresponding to that choice. For example, if participants selected 1, indicating “a strong preference for transgender people over cisgender people,” their selection was recoded in our process using the implicit IAT scores interpreted as a strong preference for transgender people (namely, scores between -0.65 and -2). The choice of 1 was thus recoded as 1.325, the midpoint of this range. See Table 1 for recoding details.
Inclusion/Exclusion Criteria. Inclusion criteria consisted of U.S. residents who had a completed overall IAT D score from either the Transgender IAT test in 2020 or from the Sexuality IAT test between the years of 2006 to 2020, and who indicated their general occupational area from a list provided by Project Implicit. We also followed the methods of Sabin et al. (2015) by excluding respondents if their IAT scores were incomplete or if they met either of the following criteria: (1) went too fast (less than 300 milliseconds) on more than 10% of the total test trials or (2) made more than 30% erroneous responses across critical blocks of the IAT. This helped to eliminate participants who were not engaging with the tasks of the IAT in a way that was likely to accurately measure implicit bias.
We used data from the Transgender IAT to compare nurses’ attitudes towards transgender individuals with other occupational groups.
We used data from the Transgender IAT (2020) to compare nurses’ attitudes towards transgender individuals with other occupational groups. Occupational groups in this study were largely categorized in a similar manner to those in Sabin et al. (2015). This categorization uses both the general occupational area of the participant and their stated level of education to determine their likely role in healthcare. For example, respondents who specifically self-identified their occupational status as “Healthcare – Nurses and Home Health Assistants” and who identified their education level as an associate degree or higher were classified as nurses. We created an additional occupational group of Healthcare Support Workers to account for those who listed a healthcare occupational area but reported lower educational attainment. See Table 2 for full details on how the occupational groups were defined.
Table 2. Occupational Group Designations
|
Description of Participant’s Occupational Area |
Education Level |
Group Designation |
|---|---|---|
|
Healthcare - Diagnosing and Treating Practitioners (MD, Dentist, etc.) |
MD |
MD |
|
Bachelor’s degree or Higher |
Other Diagnostic and Treating Providers |
|
|
Less than a Bachelor’s |
Healthcare support workers |
|
|
Healthcare - Nursing and Home Health Assistants |
Associate degree or Higher |
Nurses |
|
Less than an Associate’s degree |
Healthcare support workers |
|
|
Social Service - Counselors, Social Workers, Community specialists |
Bachelor’s degree or Higher |
Mental Health Providers |
|
Less than a Bachelor’s |
Healthcare support workers |
|
|
Healthcare - Technologists and Technicians |
Any |
Healthcare support workers |
|
Healthcare - Occupational and Physical Therapist Assistants |
Any |
Healthcare support workers |
|
Healthcare - Other healthcare support |
Any |
Healthcare support workers |
|
All Others |
Any |
Non-Providers |
To compare nurses' implicit and explicit attitudes towards transgender individuals, we further excluded those respondents who did not answer the question on explicit bias. Finally, to look at trends in nurses’ attitudes towards lesbian and gay individuals, we started with the Sexuality IAT data from 2006 to 2020 and used the same criteria as above to identify nurses.
Data Collection/Preparation
Data Access and Ethical Approval. We downloaded the de-identified Transgender and Sexuality IAT datasets from the Open Science Framework (OSF) (2023a; 2023b) website, a data repository that houses publicly available databases. Due to the de-identified, retrospective nature of the project, no risks or benefits to human subjects existed. Given that the project was a retrospective study, it did not require the current engagement of the identified population, and informed consent was not required. Verification of exempt status was secured through the university’s Institutional Review Board (IRB).
Statistical Analyses. Statistical analyses of quantitative data were performed using IBM SPSS Statistics software version 28. Implicit bias between occupational groups were compared using a one-way analysis of variance (ANOVA). The normality requirement was deemed sufficiently met due to an overall skew value of 0.011 and an excess kurtosis value of 0.021. Skew and excess kurtosis values of 0 indicate normality (Kellar & Kelvin, 2013). Further, the largest skew value for individual occupational groups was 0.092, while the largest magnitude of the excess kurtosis values was 0.184. The assumption of equal variances was deemed sufficiently met using the Hartley test, as the largest standard deviation ratio was 1.06. A value of 1 indicates equal variances (Kellar & Kelvin, 2013).
An ANOVA is robust to minor violations of the assumptions of normality and equal variance (Kellar & Kelvin, 2013). Post-hoc tests were used to compare individual groups and were adjusted using the Bonferroni method. A paired t-test was calculated to understand if a significant difference existed between IAT scores and self-reported explicit attitudes in the nurses group. The parametric test was chosen as this test is robust to violations of normality when the number of pairs is larger than 30 (Kellar & Kelvin, 2013). To evaluate nurses’ attitudes towards lesbian and gay individuals over time, the mean IAT score for each year was calculated from the Sexuality IAT file for 2006 to 2020 and graphed using a line chart.
Results
There were 179,353 respondents who completed the Transgender IAT in 2020. After applying inclusion and exclusion criteria, the total sample size was 53,586. Participants were divided into healthcare and non-provider groups, resulting in 20.8% healthcare (n = 11,163) and 79.2% non-providers (n = 42,423). The healthcare group (n = 11,163) was further divided based on occupation: 14.2% nurses (n = 1584), 6.3% physicians (MDs) (n = 705), 8.6% other diagnostic and treating professionals (n = 965), 28.8% mental health providers (n = 3210), and 42.1% healthcare support workers (n = 4699).
Participants were divided into healthcare and non-provider groups...
Participants’ reported gender identities were then calculated based on available choices, which included “male,” “female,” “trans male/trans man,” “trans female/trans woman,” “genderqueer/gender nonconforming,” and “a different identity.” Respondents who selected more than one gender identity were classified as “other.” Interestingly, in each identified group, gender identity was predominantly female (see Table 3). Additionally, we described the demographic characteristics of the nurses who completed the Transgender IAT. Most of the nurses identified as female (89.5%), White (73%), not Hispanic or Latino (86.1%), with a mean age of 34.44 years (SD=13.26). A complete table of nurse demographics is provided (see Table 4).
Table 3. Reported Gender Identity
|
|
MD |
Other Diagnostic and Treating Professionals |
Nurses |
Mental Health Providers |
Health Support |
Nonproviders |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
|
Male |
245 |
34.9 |
231 |
24.0 |
124 |
7.8 |
364 |
11.4 |
789 |
16.8 |
12059 |
28.5 |
|
Female |
447 |
63.7 |
704 |
73.0 |
1418 |
89.6 |
2619 |
81.8 |
3657 |
78.0 |
27311 |
64.5 |
|
Trans-male |
1 |
0.1 |
1 |
0.1 |
5 |
0.3 |
29 |
0.9 |
34 |
0.7 |
327 |
0.8 |
|
Trans-female |
0 |
0.0 |
3 |
0.3 |
3 |
0.2 |
11 |
0.3 |
21 |
0.4 |
248 |
0.6 |
|
Genderqueer/ Gender Nonconforming |
5 |
0.7 |
16 |
1.5 |
16 |
1.0 |
113 |
3.5 |
122 |
2.6 |
1260 |
3.0 |
|
A Different Identity |
0 |
0.0 |
0 |
0.0 |
4 |
0.3 |
15 |
0.5 |
8 |
0.2 |
194 |
0.5 |
|
Other* |
4 |
0.6 |
11 |
1.1 |
13 |
0.8 |
52 |
1.6 |
59 |
1.3 |
934 |
2.2 |
|
Total |
702 |
100 |
964 |
100 |
1583 |
100 |
3203 |
100 |
4690 |
100 |
53475 |
100 |
*Other: Respondents selected two or more gender identities.
Note: Percentages indicate the percent of the occupational group.
Table 4. Nurse Demographics
|
|
Transgender IAT 2020 |
|
|---|---|---|
|
Category |
n |
% |
|
Age |
|
|
|
Less Than 20 |
8 |
0.5 |
|
20 to 29 |
520 |
32.8 |
|
30 to 39 |
410 |
25.9 |
|
40 to 49 |
300 |
18.9 |
|
50 to 59 |
201 |
12.7 |
|
60 to 69 |
93 |
5.9 |
|
70 and above |
1 |
0.1 |
|
No response |
44 |
2.8 |
|
Race |
|
|
|
American Indian/Alaska Native |
8 |
0.5 |
|
Black or African American |
122 |
7.7 |
|
East Asian |
36 |
2.3 |
|
Multiracial |
68 |
4.3 |
|
Native Hawaiian or Other Pacific Islander |
13 |
0.8 |
|
South Asian |
24 |
1.5 |
|
White |
1157 |
73.0 |
|
Other or Unknown |
45 |
2.8 |
|
No response |
111 |
7.0 |
|
Ethnicity |
|
|
|
Hispanic or Latino |
135 |
8.5 |
|
Not Hispanic or Latino |
1364 |
86.1 |
|
Unknown |
85 |
5.4 |
Results of the computed one-way ANOVA and post hoc Bonferroni tests provided evidence of differences between some of the groups (F(5, 53580) = 19.55, p <.001). Based on mean overall IAT D scores and score range interpretations by Greenwald et al. (2003), nurses showed a “slight preference” for cisgender people (M = 0.19, SD = 0.43), while other groups had “little preference” or “no preference” (see Table 5). Differences were identified between nurses and mental health providers, healthcare support workers, and non-providers (p < .001), and between nurses and other diagnostic and treating providers (p = .035). However, no significant difference was identified between nurses and physicians (p = .548). The most significant difference was found between nurses and mental health providers (M1 – M2 = 0.12, p < .001, Cohen’s d = 0.27).
Table 5. ANOVA Results of IAT Scores by Occupation
|
Category |
M |
SD |
F-value |
p-value |
η2 |
|---|---|---|---|---|---|
|
MDs |
0.15 |
0.43 |
19.55 |
<.001 |
.002 |
|
Other diagnostic and treating providers |
0.14 |
0.45 |
|
|
|
|
Nurses |
0.19 |
0.43 |
|
|
|
|
Mental health providers |
0.07 |
0.45 |
|
|
|
|
Healthcare support workers |
0.12 |
0.44 |
|
|
|
|
Non-providers |
0.10 |
0.45 |
|
|
|
|
Total |
0.11 |
0.45 |
|
|
|
Note: Bonferroni Post-hoc comparisons indicate significant differences (p <.001) between nurses and the categories of mental health providers, healthcare support workers, and nonproviders. There was also a significant difference (p = .035) between Nurses and Other diagnostic and treating providers. Significant differences (p < .01) were also noted between Mental-Health Providers and all other occupational groups.
To compare nurses’ implicit and explicit transgender bias, we examined data from 1,558 nurses who answered the question on explicit bias. A total of 61.7% of these nurses reported no preference between transgender and cisgender people, while 34.7% reported they had some level of preference for cisgender people (see Table 1). A paired t-test was conducted comparing the mean overall IAT D scores (M = 0.19, SD = 0.43) to the mean recoded explicit scores (M = 0.17, SD = 0.37), which found no significant difference between implicit and explicit scores (Md = 0.02, SD = 0.49, t(1557) = 1.948, p = .052) (see Table 6).
Table 6. Paired t-test Comparing IAT Scores with Explicit Self-Evaluation
|
Group |
M |
SD |
n |
t |
p |
|---|---|---|---|---|---|
|
Mean IAT Scores |
0.19 |
0.43 |
1558 |
1.948 |
.052 |
|
Mean Recoded Explicit Scores |
0.17 |
0.37 |
|
|
|
Nurses’ implicit attitudes about sexual orientation were found to be trending toward less biased scores.
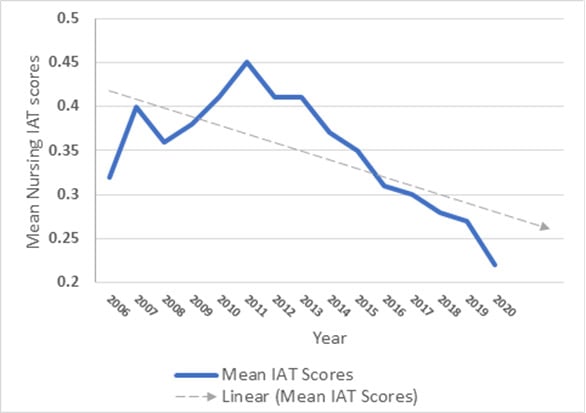
To evaluate nurses' attitudes towards lesbian and gay individuals over time, we started with the 4,263,187 respondents who took the Sexuality IAT between 2006 and 2020. After applying inclusion and exclusion criteria, the total sample was 25,791. Mean overall IAT D scores were calculated for each year between 2006 and 2020. Nurses’ implicit attitudes about sexual orientation were found to be trending toward less biased scores. From 2007 to 2011, the mean overall IAT D score rose from 0.40 to 0.45, which indicated a moderate preference for heterosexuals. The year 2011 showed the highest overall IAT D score mean (M = 0.45, SD = 0.43). Between 2012 and 2020, the mean decreased from 0.41 to 0.22, indicating a shift from a moderate to a slight preference for heterosexuals (see Figure 3).
Figure 3. Mean IAT Scores (Implicit Bias Towards Gay and Lesbian) 2006 – 2020
Discussion
Differences between Nurses’ Transgender IAT Scores and Other Groups
Our initial aim for this part of the study was to identify whether a difference existed between U.S. nurses’ Transgender IAT scores and other groups. The study is thought to be one of the first of its kind to describe the differences in nurses’ implicit attitudes about transgender people compared to other occupations. Of all categorized groups, nurses held the strongest implicit preference for cisgender people, and significant differences were found between nurses and other diagnostic and treating providers, mental health providers, healthcare support workers, and non-providers. Only the physician (MDs) group did not show a significant difference compared to nurses. Based on overall Transgender IAT D scores, the nurses group only slightly preferred cisgender individuals, while mental health providers and all other groups had little to no preference. These findings are consistent with the general trend toward SGM acceptance (National Academy of Sciences, 2020), but may reflect response bias as it seems plausible that those professionals who choose to take the Transgender IAT test may skew towards individuals with more acceptance.
The gender identity makeup of these professions may also play a role.
The gender identity makeup of these professions may also play a role. Mental health providers, non-providers, and healthcare support workers had the largest number of participants who identified as genderqueer/gender nonconforming (3.5%, 3%, and 2.6% respectively), the highest total number of participants) who chose a category other than “male” or “female” (6.8%, 7.1%, and 5.2% respectively), and the largest numbers of participants who identified as transgender (1.2%, 1.4%, and 1.1%, respectively) (see Table 3). These three groups also had the lowest overall Transgender IAT scores (M = 0.07, M = 0.10, and M = 0.12, respectively), which may signify the need for additional SGM representation within the healthcare workforce to reduce the level of implicit bias toward transgender people.
Differences between Nurses’ Transgender IAT Scores and Explicit Attitudes
Based on the frequency of responses, most nurses reported no preference between transgender and cisgender individuals (n = 61.7%). Despite this finding, the mean recoded explicit scores calculation indicated a slight preference for cisgender individuals (M = 0.17, SD = 0.37) although that difference was not statistically significant (M = 0.19, SD = 0.43). Implicit biases have been commonly considered unknown and vastly different from explicit attitudes (Chapman et al., 2013). However, we found that both nurses’ implicit and explicit attitudes identified a slight preference for cisgender people, which indicates that the nurses may have a general awareness of their own transgender biases.
Implicit biases have been commonly considered unknown and vastly different from explicit attitudes.
Despite awareness, nurses may not have the appropriate resources to effectively change their attitudes, which is evident based on the lack of professional training and unfamiliarity with SGM patient care (Carabez et al., 2015; Collins, 2020; Eickhoff, 2021; James et al., 2016; Paradiso & Lally, 2018; Sirota, 2013). Nurses are likely more confident in their skills in familiar settings; nurses who are inexperienced with transgender patient care may have reservations about caring for these patients stemming from confusion about appropriate care methods, lack of knowledge related to terminology, and lack of experience with actual transgender patients (Carabez et al., 2016). Campinha-Bacote (2003) described this type of behavior as “conscious incompetence,” one of four stages of competence. Implicit and explicit attitudes align with this model, which begins with unconscious incompetence where the nurse does not know that cultural knowledge is lacking (similar to implicit attitudes where the nurse is not aware of existing or underlying bias), followed by conscious incompetence where awareness exists without the knowledge of how to correct it (i.e., explicit attitudes).
Trends on Nurses’ Attitudes about Sexual Orientation
Finally, we determined that nurses’ attitudes about sexual orientation were trending toward less biased scores. Although Sabin et al. (2015) found that nurses had the strongest implicit preferences for heterosexuals, our findings suggest that nurses’ attitudes have become more accepting of lesbian and gay individuals. As societal attitudes shift toward the affirmation of diversity, equity, and inclusion of the SGM population, more nurses are likely to follow suit. However, without adequate preparation and training on SGM healthcare needs, the potential for bias and errors in judgment may still exist.
...our findings suggest that nurses’ attitudes have become more accepting of lesbian and gay individuals.
Nursing Implications and Future Directions for Practice
Considering these results, nursing programs and healthcare facilities should deliberately consider the impact of implicit bias on patient care and the lack of SGM health education. Comprehensive education that supports nurses’ understanding of SGM patient care could help nurses avoid errors and constructively care for patients using a holistic, individualized approach. Inclusion of this content may also improve nurses’ attitudes and willingness to care for these individuals (Eickhoff, 2021).
Building on the American Association of Colleges of Nursing (AACN) (2021) Essentials domain #2 regarding person-centered care, nurses must promote holistic, individualized, respectful, coordinated, evidence-based experiences for every patient. Person-centered care focuses on a respect for diversity and differences and requires nurses to have intentional presence as they seek to understand an individual’s lived experiences. The AACN stressed the importance of person-centered care as a foundational element to nursing education across all practice areas (AACN, 2021).
Structuring programs that integrate SGM health education throughout the curricula may help promote person-centered care and better prepare nurses in alignment with the AACN (2021) standards. Individuals that identify within the SGM community are seen in a variety of healthcare settings and contexts. Care of these patients spans every specialty area, including but not limited to pediatrics, obstetrics and gynecology, medical-surgical, cardiology, and emergency departments. Providing objective information throughout the entire program of nursing education might help close knowledge gaps about caring for SGM patients within different types of settings, thus increasing the number of nurses who feel prepared to care for SGM patients and potentially reducing associated biases and varied levels of incompetence. However, more guidance on curricula and SGM content is needed (Eickhoff, 2021).
...more guidance on curricula and SGM content is needed.
Nurses themselves can promote health and well-being for SGM patients by incorporating practices that include identifying and using the patient’s preferred name, gender, and pronouns; understanding SGM terminology; and integrating techniques that mitigate bias. Using a patient’s preferred name, gender, and pronouns validates that patient’s choices and is critical to the health of transgender and gender diverse individuals (Sevelius et al., 2020). Misgendering a patient, using incorrect pronouns, or calling a patient by the wrong name can communicate disrespect and may even cause harm or perpetrate an unsafe environment (Sevelius et al., 2020).
Nurses’ confusion related to terminology suggests that understanding SGM definitions may help nurses more effectively treat patients (Carabez et al., 2016). For example, gender identity and sexual orientation are two very different terms but whereas gender identity speaks to how a person identifies (e.g., male, female, nonbinary, two-spirit), sexual orientation describes to whom a person is attracted (e.g., heterosexual, lesbian, gay, asexual, pansexual). Carabez et al. (2016) noted the importance of nurses in understanding the continuum of gender outside of the gender binary status quo.
Nurses’ confusion related to terminology suggests that understanding SGM definitions may help nurses more effectively treat patients.
Future directions for nursing practice should also support practices that help nurses mitigate biases, such as mindfulness. Rooted in the ethical concepts of empathy and compassion, mindfulness has been used to reduce stress and improve communication patterns (Narayan, 2019). Burgess et al. (2017) described how mindfulness practices could help reduce implicit bias activation, as well as enhance awareness and control over triggered biases. Removing distractions and focusing on the present moment can help nurses recognize their biases and be more deliberate in their actions (Narayan, 2019).
Another bias reduction method is habit replacement, which requires nurses to consider their implicit attitudes as “bad habits” that can be broken and replaced with more desirable habits that involve acceptance, caring, and nonbiased thinking (Devine et al., 2012). Replacing a bad habit takes practice and a stepwise approach, such as recognizing the habit, planning for change, and practicing the new habit consciously and persistently (Narayan, 2019). Several additional methods to counteract bias have been referenced in the literature, including allyship, emotional regulation, individuation, partnership building, and perspective taking (Narayan, 2019; Wu et al., 2019). Regardless of the tools chosen, all these strategies involve a level of self-awareness, self-regulation, and a commitment to care for all.
Replacing a bad habit takes practice and a stepwise approach...
Additional studies may consider the impact of demographics, such as age, race, religion, political affiliation, and geographic location, and how these data influence implicit and explicit preferences. The effects of implicit preferences on actual patient outcomes need further review. How these preferences influence health disparities within the SGM population, and methods to reduce these inequalities, both also require more research.
The effects of implicit preferences on actual patient outcomes need further review.
Strengths and Limitations
This study offers additional insight into nurses’ perspectives of vulnerable populations and awareness of the potential negative impact of these attitudes on SGM patient care. Although the samples are not representative of definable populations, the available datasets and the large sample numbers enhance the generalizability of findings. In addition, the IAT has repeatedly shown statistical reliability, validity, and internal consistency (Greenwald & Nosek, 2001; Greenwald et al., 2009; Greenwald et al., 2015; Manns-James, 2015). One potential limitation includes recoding explicit scores to align with IAT scores, which may have affected the reported outcomes. Also, those individuals who identify as female are over-represented within the sample populations.
Conclusion
Nurses are not immune to implicit bias and its potentially negative influence on patient care. While our findings indicated that nurses had a slight implicit and explicit preference for cisgender people, nurses’ attitudes regarding sexual orientation have trended toward less biased scores over the past ten years. Although discrimination and stigma still exist, overall attitudes about the SGM population appear to be gradually moving toward inclusion and acceptance.
Nurses are not immune to implicit bias and its potentially negative influence on patient care.
Supporting nurses’ education and their awareness of the needs of SGM patients could further these efforts. Working together to promote an environment that defends diversity, inclusivity, and equity requires continuous effort and practice. Nurses must protect the rights of all patients regardless of gender identity or sexual orientation. Developing a therapeutic relationship requires genuine caring and understanding of a patient’s perspective, respect for differences, and partnership-building (Narayan, 2019). When mindful of these aspects of patient care and aware of their own biases, nurses may be able to deliver more effective SGM patient-centered care.
Implementing changes in current professional nursing programs and nursing education modalities could also help reduce the adverse effects of implicit bias.
Implementing changes in current professional nursing programs and nursing education modalities could also help reduce the adverse effects of implicit bias. Training to enhance implicit bias awareness, tools to counteract the consequences of bias, and education on the specific healthcare needs of the SGM population are needed. Nursing is highly regarded as a trustworthy profession. Addressing nurses’ implicit bias is critical to maintain trust, provide better nursing care, improve patient health outcomes, and reduce health disparities for all SGM individuals.
Author Note
We have no known conflict of interest to disclose. Correspondence concerning this article should be addressed to Carolyn M. Howard, 3255 New Hope Road, Hendersonville, TN 37075.
Phone: (615) 681-5805 or email below.
Authors
Carolyn M. Howard, DNP, MSN, RN, NE-BC, CNE
Email: carolyn.howard@belmont.edu
ORCID ID: 0009-0004-9779-4675
Dr. Howard is a Registered Nurse who has worked in healthcare for the past 29 years, primarily as a nurse leader for various healthcare organizations in the Nashville area, including Vanderbilt University Medical Center where she managed the outpatient Eskind Diabetes and Endocrinology Center and directed the Health IT Customer Care team. She is currently employed as full-time nursing faculty at Grand Canyon University located in Phoenix, Arizona, for the online Accelerated Bachelor of Nursing (ABSN) pre-licensure program and has taught for 11 years as an adjunct faculty in the undergraduate nursing program at Belmont University in Nashville, Tennessee. Dr. Howard graduated from Belmont with a Doctor of Nursing Practice degree in May 2022; her research focus was implicit bias in nursing and its effects related to patient care of the LGBTQ+ population. Her passion for this work stems from both her personal and professional experiences working with this vulnerable population and raising her transgender child. She has been certified as a Nurse Executive since 2014 through the American Nurses Credentialing Center and as a Certified Nurse Educator since 2021 from the National League for Nursing, of which she is also a member.
Linda G. Wofford, DNP, RN, CPNP
Email: linda.wofford@belmont.edu
ORCID ID: 0000-0001-9976-3865
Dr. Wofford is Professor and Assistant Dean of Nursing Evaluation & Assessment at Belmont University. With over 40 years of experience in nursing, Linda has a wide perspective about nursing in acute and community settings across the lifespan. She continues to seek effective strategies that can positively impact health outcomes for all people.
David Phillippi, PhD
Email: david.phillippi@belmont.edu
ORCID ID: 0000-0003-4723-8588
Dr. Phillippi earned a BS in Mathematics in 1997 and was inducted into Phi Beta Kappa. He earned an MS in Mathematics in 2003 and a PhD in Mathematics in 2007, both from the University of Tennessee. He has been teaching Statistics and Research Methods in the Belmont University School of Nursing since 2018. His interest in the topic stems in part from seeing his own child navigate the healthcare system as a member of the LGBTQ+ community.
References
American Association of Colleges of Nursing (AACN). (2021). The essentials: Core competencies for professional nursing education. https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf
Ayhan, C. H. B., Bilgin, H., Uluman, O. T., Sukut, O., Yilmaz, S., & Buzlu, S. (2020). A systematic review of the discrimination against sexual and gender minority in health care settings. International Journal of Social Determinants of Health and Health Services, 50(1), 44 – 61. https://doi.org/10.1177/0020731419885093
Burgess, D. J., Beach, M. C., & Saha, S. (2017). Mindfulness practice: A promising approach to reducing the effects of clinical implicit bias on patients. Patient Education and Counseling, 100(2), 372 – 376. https://doi.org/10.1016/j.pec.2016.09.005
Campinha-Bacote, J. (2003). Many faces: Addressing diversity in health care. Online Journal of Issues in Nursing, 8(1), manuscript 2. https://doi.org/10.3912/OJIN.Vol8No01Man02
Carabez, R., Pellegrini, M., Mankovitz, A., Eliason, M., Ciano, M., & Scott, M. (2015). “Never in all my years…”: Nurses’ education about LGBT health. Journal of Professional Nursing, 31(4), 323-329. https://doi.org/10.1016/j.profnurs.2015.01.003
Carabez, R., Eliason, M. J., & Martinson, M. (2016). Nurses’ knowledge about transgender patient care: A qualitative study. Advances in Nursing Science, 39(3), 257 – 271. https://doi.org/10.1097/ANS.0000000000000128
Chapman, E. N., Kaatz, A., & Carnes, M. (2013). Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. Journal of General Internal Medicine, 28(11), 1504 – 1510. https://doi.org/10.1007/s11606-013-2441-1
Collins, C. A. (2020). Pediatric nurse practitioners’ attitudes/beliefs and knowledge/perceived competence in caring for transgender and gender‐nonconforming youth. Journal for Specialists in Pediatric Nursing, 26(2). https://doi.org/10.1111/jspn.12321
Devine, P. G., Forscher, P. S., Austin, A. J., & Cox, W. T. L. (2012) Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of Experimental Social Psychology, 48(6), 1267 – 1278. https://doi.org/10.1016/j.jesp.2012.06.003
Divan, V., Cortez, C., Smelyanskaya, M., & Keatley, J. (2016). Transgender social inclusion and equality: A pivotal path to development. Journal of the International AIDS Society, 19(3). https://doi.org/10.7448/IAS.19.3.20803
Edgoose, J. Y. C., Quiogue, M., & Sidhar, K. (2019). How to identify, understand, and unlearn implicit bias in patient care. Family Practice Management, 26(4), 29 – 33. https://pubmed.ncbi.nlm.nih.gov/31287266/
Eickhoff, C. (2021). Identifying gaps in LGBTQ health education in baccalaureate undergraduate nursing programs. Journal of Nursing Education, 60(10), 552 – 558. https://doi.org/10.3928/01484834-20210729-01
Epifania, O. M., Anselmi, P., & Robusto, E. (2020). DscoreApp: A shiny web application for the computation of the implicit association test D-score. Frontiers in Psychology, 10, 2938. https://doi.org/10.3389/fpsyg.2019.02938
Greenwald, A. G., Banaji, M. R., & Nosek, B. A. (2015). Statistically small effects of the implicit association test can have societally large effects. Journal of Personality and Social Psychology, 108(4), 553 – 561. https://doi.org/10.1037/pspa0000016
Greenwald, A. G., & Nosek, B. A. (2001). Health of the Implicit Association Test at age 3. Zeitschrift für Experimentelle Psychologie, 48(2), 85 – 93. https://doi.org/10.1026//0949-3946.48.2.85
Greenwald, A. G., Nosek, B. A., & Banaji, M. R. (2003). Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85(2), 197–216. https://doi.org/10.1037/0022-3514.85.2.197
Greenwald, A. G., Poehlman, T., Uhlmann, E. L., & Banaji, M. R. (2009). Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. Journal of Personality and Social Psychology, 97(1), 17–41. https://doi.org/10.1037/a0015575
Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK64806/
James, S. E., Herman, J. L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The report of the 2015 US Transgender Survey. Washington, DC: National Center for Transgender Equality. https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf
Jones, J. (2022, February 17). LGBT identification ticks up to 7.1%. Gallup. https://news.gallup.com/poll/389792/lgbt-identification-ticks-up.aspx
Kellar, S., & Kelvin, E. (2013). Monro’s Statistical Methods for Health Care Research. Wolters Kluwer.
Manns-James, L. (2015). Finding what is hidden: A method to measure implicit attitudes for nursing and health-related behaviours. Journal of Advanced Nursing, 71(5), 1005 – 1018. https://doi.org/10.1111/jan.12626
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. https://doi.org/10.1037/0033-2909.129.5.674
Narayan, M. C. (2019). CE: Addressing implicit bias in nursing: A review. American Journal of Nursing, 119(7), 36 – 43. https://doi.org/10.1097/01.NAJ.0000569340.27659.5a
National Academy of Sciences. (2020). Demography and public attitudes of sexual and gender diverse populations. In White, J., Sepúlveda, M., Patterson, C. (Eds.) Understanding the well-being of LGBTQI+ populations. National Academies of Sciences, Engineering, and Medicine; Division of Behavioral and Social Sciences and Education; Committee on Population; Committee on Understanding the Well-Being of Sexual and Gender Diverse Populations. https://www.ncbi.nlm.nih.gov/books/NBK566077/
National Institutes of Health. (2015). NIH FY 2016-2020 Strategic plan to advance research on the health and well-being of sexual and gender minorities. National Institutes of Health Sexual and Gender Minority Research Coordinating Committee, National Institutes of Health. https://dpcpsi.nih.gov/sites/default/files/sgmStrategicPlan.pdf
Open Science Framework (OSF). (2023a). Project Implicit demo website datasets. Sexuality IAT 2004 – 2022. https://osf.io/ctqxo/
Open Science Framework (OSF). (2023b). Project Implicit demo website datasets. Transgender IAT 2020 – 2022. https://osf.io/fb29q/
Paradiso, C. & Lally, R. M. (2018). Nurse practitioner knowledge, attitudes, and beliefs when caring for transgender people. Transgender Health, 3(1), 48 – 56. https://doi.org/10.1089/trgh.2017.0048
Parent, M. C., Arriaga, A. S., Gobble, T., & Wille, L. (2019). Stress and substance use among sexual and gender minority individuals across the lifespan. Neurobiology of Stress, 10, 100146. https://doi.org/10.1016/j.ynstr.2018.100146
Project Implicit. (2011a). About us. About Us. https://implicit.harvard.edu/implicit/aboutus.html
Project Implicit. (2011b). Education: About the IAT. Learn More. https://implicit.harvard.edu/implicit/iatdetails.html
Project Implicit. (2011c). Preliminary information. Take a Test.https://implicit.harvard.edu/implicit/takeatest.html
Sabin, J. A., Riskind, R. G., & Nosek, B. A. (2015). Health care providers’ implicit and explicit attitudes toward lesbian women and gay men. American Journal of Public Health, 105(9), 1831 – 1841. https://doi.org/10.2105/AJPH.2015.302631
Sevelius, J. M., Chakravarty, D., Dilworth, S. E., Rebchook, G., & Neilands, T. B. (2020). Gender affirmation through correct pronoun usage: Development and validation of the transgender women’s importance of pronouns (TW-IP) scale. International Journal of Environmental Research and Public Health, 17(24), 9525. https://doi.org/10.3390/ijerph17249525
Sinha, R. (2008). Chronic stress, drug use, and vulnerability to addiction. Annals of the New York Academy of Sciences, 1141(1), 105–130. https://doi.org/10.1196/annals.1441.030
Sirota, T. (2013). Attitudes among nurse educators toward homosexuality. Journal of Nursing Education, 52(4), 219 – 227. https://doi.org/10.3928/01484834-20130320-01
Wu, D., Saint-Hilaire, L., Pineda, A., Hessler, D., Saba, G. W., Salazar, R., & Olayiwola, N. (2019). The efficacy of an antioppression curriculum for health professionals. Family Medicine, 51(1), 22-30. https://doi.org/10.22454/FamMed.2018.227415


