Innovation skills are part of 21st century skills, a broad skillset that supports healthcare professionals to better sustain, or future-proof, a career in the modern workplace. Educational programs and services in healthcare need to prepare students to innovate in order to address complex needs of aging and changing demographics in global populations. Early career healthcare professionals will benefit from skills and adaptability to tackle challenges and innovate their practices. Engagement in innovation that involves technology cultivates such new skill sets, fosters leadership, and positions these healthcare professionals as critical players in shaping the future of their professions. In this article, we describe examples of integrating 21st century skills into three categories: curriculum and instruction, professional development, and learning environments, based on a partnership framework for 21st century learning. Our shared examples offer an international perspective on the topic of innovation, describing efforts within occupational therapy, nursing, and social work programs in Canada, The Netherlands, and the USA. In the area of curriculum and instruction, we include initiatives to build innovation skills both within a single course and integrated opportunities throughout the curricula. From the professional development perspective, new professional roles and programs have emerged with a focus on technology. Finally, educational support systems have fostered innovative learning environments for interdisciplinary education with a focus on collaboration, innovation, and creativity. In all examples, interprofessional collaboration between education and practice was a leading strategy to prepare healthcare professionals across the globe with necessary 21st century leadership skills for innovative practice.
Key Words: skills, innovation, technology, professionals, healthcare, social work, occupational therapy, human centered design, design thinking, 21st century skills
Educational programs, healthcare, and social work services need to continuously innovate their practices to address the ageing and changing demographics in global populations (World Health Organization [WHO], 2015). Increasing numbers of people with chronic diseases and co-morbidities, along with increased disparities and digitization of our societies, impact healthcare and social work services (WHO, 2015) Healthcare and welfare organizations seek a balance between providing high standards of (social) care versus economic viability and efficiency due to staff shortages (Czuba et al, 2023; Endalamaw et al., 2024).
Educational programs, healthcare, and social work services need to continuously innovate their practices to address the ageing and changing demographics in global populations
Use of emerging technology can help with these challenges (WHO, 2015). For instance, technologies can bridge the gap between the increasing demand for care in times of staff shortages (Endalamaw et al. 2024). However, to reach this potential, application and use of such technologies need to be incorporated into educational programs to future-proof healthcare and social work professionals and occupational therapists (hereafter: healthcare professionals) (Groeneveld et al., 2024) and prepare these leaders to successfully integrate technologies into practice (Snow, 2019). Rapid development of new technologies, such as artificial intelligence (AI), also challenges educators to prepare future healthcare professionals to critically examine the potential of such tools to disempower and depersonalize patients or reduce the transparency of outcomes from AI and human contact (Groeneveld et al., 2024).
...early career healthcare professionals need innovation skills and adaptability to tackle these real-world practice challenges...
In this evolving landscape, early career healthcare professionals need innovation skills and adaptability to tackle these real-world practice challenges and innovate their practices (Amankawaa et al., 2022). The practice-based challenges healthcare providers face are diverse, medical, technical, or non-technical in nature. They require innovations of equipment, clinical processes, technologies, and services for the purpose of efficiency, effectiveness, user-satisfaction, and/or costs. Innovative solutions should not be ascribed to engineering professions only; these may be developed by anyone, including nurses, occupational therapists and social workers.
Healthcare professionals bring perspectives and expertise grounded in patient and client experiences, ethical considerations, real-world challenges, and can ensure that innovations are human-centered, culturally sensitive and ethically grounded (White et al., 2016). These contextual perspectives and innovative ideas can position healthcare professionals on a spectrum from users to co-developers. This transition is necessary as current developments may not align with the needs of healthcare professionals. Though professionals have numerous valid ideas to address pain points (i.e., frustrations or difficult problems that could benefit from innovation), they find that they are challenged to innovate their practices, as, for example, the curriculum is often rather fixed by national and professional guidelines. Also, healthcare faculty are commonly not trained and experienced in developing innovative projects.
Innovative solutions should not be ascribed to engineering professions only; these may be developed by anyone...
Engagement in innovation that involves various technologies cultivates new skill sets. For example, innovators learn to adapt to change and stay flexible. Innovation fosters leadership, and positions healthcare professionals as critical drivers in shaping the future of their fields (i.e., “future-proof” professionals bolstered by these skill sets in an evolving environment). But how are students currently prepared to take on this role? While much is known about the needed core skills and tasks of professionals to become licensed providers working in healthcare and social work (Oskarsson & Vik, 2024; Roller-Wirnsberget et al., 2020), less is known about the way we educate new healthcare professionals to play a role in this constantly changing workspace (Aykan et al., 2022).
Innovation fosters leadership, and positions healthcare professionals as critical drivers in shaping the future of their fields...
Hence, both the need for systematic and integrated innovation education and a practice environment with trial programs are needed. In this article, we explore approaches in education that can instruct, future-proof, and prepare today’s healthcare professionals. We describe various programs in three countries and their progress to bring innovation skill sets that to health professionals. We will share examples of global collaboration on successful education programs that may lead the way towards innovations developed by health professionals to address practice gaps.
Best Practices in Canada, The Netherlands, and the USA
Future-proof education is synonymous with "future skills" and "21st century skills" or more general terminologies such as "skills" and "competencies" (Blouin, 2023). The United Nations Educational, Scientific and Cultural Organization (UNESCO) International Centre for Technical and Vocational Education and Training defines the term 21st century skills as a broad range of skills supporting a professional to better navigate a career in the modern workplace. The Partnership for 21st Century Learning (P21) framework (Network for BattelleforKids, 2019) divides the 21st century skills into three categories (see Figure 1). The first category is Learning and Innovation Skills, which include creativity, innovation, critical thinking, problems solving, communication and collaboration. The second category is Information, Media, and Technology Skills, which include information literacy, media literacy and ICT literacy. The last category is Life and Career Skills, which include flexibility, adaptability, initiative and self-direction, social and cross-cultural skills, productivity and accountability, leadership and responsibility.
Future-proof education is synonymous with "future skills" and "21st century skills"...
Figure 1. Partnership for 21st Century Learning Framework
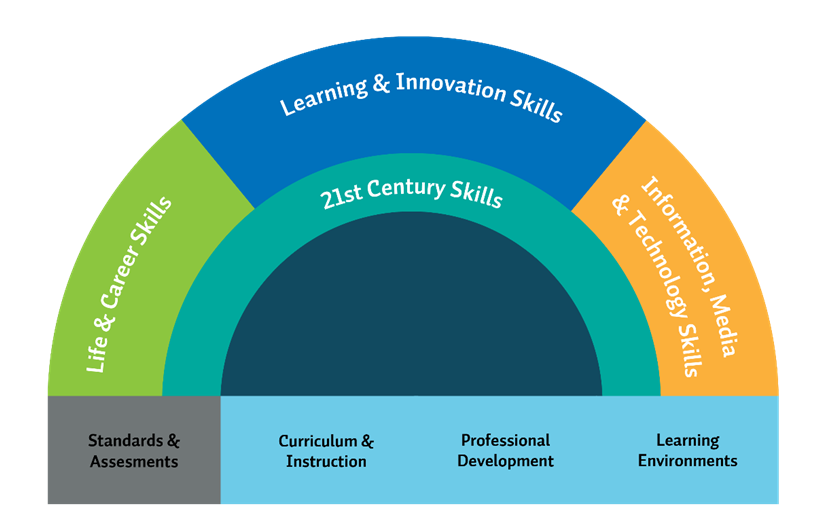
(Figure adapted from Network of BattelleforKids, 2019).
The foundation of the Partnership for 21st Cenrury Learning Framework, or P21 framework,P21 framework includes curriculum and instruction, professional development, and learning environments to integrate the 21st century skills in education to prepare students for their future professions and lifelong learning. In this article, we explore examples on a global level for integrating 21st century skills into curriculum and instruction, professional development, and learning environments, based on this P21 framework, with a focus on occupational therapy, nursing, and social work programs in Canada, The Netherlands, and the United States of America (US).
Integration of 21st Century Skills in Curriculum and Instruction
The first educational support system is integration in the curriculum and instruction area. This focus is on opportunities in the curricula to apply 21st century skills and a competency-based approach to learning beyond physical school walls. Integration of 21st century skills, and more specifically learning and innovation skills, is not new. For example, in Canada in the 1990s, occupational therapy students collaborated with industrial design students on capstone projects focused on design strategies to address challenges of aging (Liu et al., 2001; Liu & Lederer, 2009). The program was also the first in Canada to work with industry to offer “tele-rehabilitation” (Liu, 2018). This initiative was motivated by a need for faculty to remotely supervise students during clinical placement in rural areas where there were no therapists. The 21st century curricula would provide students with opportunities to anticipate the rapid evolution of interprofessional roles, expertise and tools as technologies evolve and become more accessible.
...initiatives focus both on a single course and on integration of 21st century skills and technology throughout the curriculum.
Current developments in education show that initiatives focus both on a single course and on integration of 21st century skills and technology throughout the curriculum. These two brief examples describe innovation in an educational setting that focused on a single course or event.
Hackathon. An example of a single course focussed learning and innovation skills is participation in a hackathon with participants from Canada, Netherlands, and the USA. In the hackathon, students of nursing, social work, and occupational therapy professions work together on solutions for real-world problems. In a relatively short period of time students must deliver a prototype solutions for real-world problems. In a relatively short period of time students must deliver a prototype solution and pitch their solution or concept to representatives of healthcare organizations. While hackathons can be a single course, they have also been implanted as electives between courses in different disciplines, or events that leverage conferences and scientific meetings.
Innovative & Design Thinking Module. Another example with the focus on critical thinking and creativity is a nursing quality and safety course in the United States that was modified to include a module about innovating nursing practice. Graduate nursing students study concepts and skills to lead, implement, and evaluate quality and safety projects. Students also participate in an Innovation & Design Thinking (I&DT) module. The I&DT module used the U.S. National Science Foundation (NSF) (n.d.) I-Corps 4-week program to structure module. Leary & Burger (2022) clarified the phases of design thinking and its natural alignment with the nursing process, as follows:
"The design thinking process is human-centered and has five main stages: Empathy, Define, Ideate, Prototype, and Test. These five stages tie in closely with the five stages of the nursing process, Assess, Diagnose, Plan, Implement, and Evaluate. This process is also human-centered, so we are already trained to be thinking [sic] this way" (para. 4).
Small groups of nursing students were assigned to innovate a stubborn nursing problem (e.g., patient-facing technology, falls, multi-disciplinary communication). Doctor of Nursing Practice (DNP) and Master of Nursing (MN) students participated in four 1-hour synchronous online sessions learning about human-centered design/design-thinking focusing on a nursing problem. Small student teams conducted interviews to understand (i.e., empathize) the issue from the patient or user perspective, define the underlying problem from that perspective, and brainstorm (ideate) solutions. A user-focused prototype was then presented as a storyboard on a slide and shared in class. Many solutions focused on efficiency, effectiveness, safety; better durable medical equipment, and technology use (Talsma et al., 2025).
On the other hand, educating future-proof professionals also demands the integration of 21st century skills throughout the curriculum. The following example describes the efforts of an occupational therapy program in Canada to improve technology literacy and skills.
Integration of Technology Literacy. Leaders in the Occupational Therapy Program of the University of Alberta, in Canada recognized the need to enhance the technology literacy of occupational therapists. Liu (2018) emphasized that to lead in the era of the Fourth Industrial Revolution, occupational therapists must overcome their fears and embrace the opportunities that technology presents. Bier et al. (2022) noted that a new form of interdisciplinary collaboration is emerging, particularly between occupational therapy practitioners and experts in artificial intelligence. However, the rapid pace of technological progress presents challenges. For example, research findings have suggested that occupational therapists still lack the necessary knowledge and skills to effectively address tech-related occupations. This underscores the urgent need to develop and implement educational programs focusing on digital competencies (Segal & Doyle, 2023).
From this vision the program now integrates technology awareness and digital literacy skills in its curriculum.
From this vision the program now integrates technology awareness and digital literacy skills in its curriculum. Beginning in orientation week, students are introduced to the role of technology in shaping occupational participation and building a foundation of awareness. In the first year, students explore the connection between technology and occupation through a range of courses, gaining both theoretical knowledge and hands-on experience. In the second year, they undertake a dedicated course focused on advanced technologies such as AI, robotics, extended reality (XR), smart home systems, and Brain Computer Interface, featuring hands-on activities that teach the use of these innovations in clinical practice.
This progressive, integrated approach ensures that students are proficient in the use of these tools and capable of guiding patients to adopt technologies that enhance their participation in daily activities. In this course, instructors from non-traditional disciplines, including engineering, computer science, and design, collaborate with occupational therapy, offering students valuable opportunities for interdisciplinary learning and fostering a broader educational perspective.
Integration 21st Century Skills in Professional Development
The second educational support system is professional development. This perspective highlights how programs and faculty or instructors can integrate 21 century skills into tools, teaching strategies, and new professions and programs. At the national level in the United States, the importance of innovation for the nursing profession has been noted (Leary et al, 2022). For example, the National Academies of Sciences, Engineering, and Medicine (NASEM, formerly Institute of Medicine) report, The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity (2021), includes the need to innovate nursing practice. Hagle et al. (2020) positions innovation as a pillar of knowledge alongside inquiry and improvements in nursing. Furthermore, recent publications of the American Association of Colleges of Nursing (2021) include specific competencies about innovation, , such as focus on empathy (2.1a) and optimization of system effectiveness through application of innovation and evidence-based practice (7.3). Academics and healthcare systems are applying the tenets of a Learning Healthcare System concept, where learning through trial and error is central to improving patient outcomes (NASEM, 2007).
As competencies related to nursing innovation are established, incorporating learning experiences about innovation becomes the next step. In addition to tools and teaching strategies, new professions and programs emerge. In this section we will describe several examples of incorporating innovative thinking in skills for professional development.
Health and Technology Coursework. In the Netherlands, Saxion University of Applied Sciences, had already anticipated and initiated preparations for the growing impact of technology in the profession of nursing. In addition to the regular nursing program, a study route “Health and Technology” was developed to educate bridge builders between healthcare and technology. This study route was developed in close collaboration with healthcare organizations whose leaders had indicated an interest in certified nurses with added interest and skills in the field of innovation and technology.
Front-Runners. While learning to work with technology is currently standard practice of nursing education in the Netherlands (Bouwes et al., 2023), there is a demand for nurses who act as a front-runners in their teams and organization in this field. Front-runners can support their nursing colleagues when working with technology, provide input for the design of (new) technologies, can effectively communicate with technically educated workers, and are able to oversee ethical issues that may arise when using technology. Part of the study route is a semester long innovation internship. For 20 weeks students specifically do not focus on traditional core nursing skills, but rather on the innovative skills needed to act as a nursing front-runner on innovation and technology. To date, over 500 students graduated from this study route.
Cross-Domain Collaboration. Another example is the Master of Health Care & Social Work program in The Netherlands, which focuses on cross-domain collaboration. Students with a background in health or social work background (e.g., nursing, physiotherapy, social work) learn to integrate research and innovation into their practice and foster innovation of their domain. They develop a critical perspective to formulate policies that support and promote technological innovation. All students study part time and they combine their master's education with working in practice. Students are encouraged to perform their assignment in their own organization and thereby contributing to innovation at that organization. In addition, the use of technology is always part of the assignment and students have to appraise whether technology is, or is not, of added value to solving the problems.
...students have to appraise whether technology is, or is not, of added value to solving the problems.
Integration 21st Century Skills in Learning Environments
The third educational support system is learning environments and learning practices, human support, and physical environments that will support the teaching and learning of 21st century skills. Here we describe an example of interdisciplinary education that has created an innovative learning environment for several thousand students.
Interdisciplinary Education. The Smart Solutions Semester at Saxion University of Applied Sciences fosters an innovative learning environment by interdisciplinary education. The Smart Solutions Semester provides an infrastructure that can be utilized each semester. This innovation involves students from different degree programs working together to resolve complex issues faced by our research groups and the professional field. These are problems that cannot be resolved by one discipline on its own. This is why students work in interdisciplinary teams that focus on collaboration, innovation and creativity. Project teams consist of six to eight students from different degree programs.
These are problems that cannot be resolved by one discipline on its own.
Each team has a unique mix of experience, skills and talents. In total, students enrolled in programs for nursing, civil engineering, and economics are participants. They spend five months working on the Smart Solutions Semester. Teachers collaborate with the project teams, focusing on personal development, teamwork, and quality of the product. In addition to working on their own project, students also participate in workshops to learn new skills. Design Thinking is one of the commonly used research methods in the Smart Solutions Semester because of its focus on research and innovation/development. Annually, approximately 2,000 students from 24 programs participate in the semester. They form about 285 project teams, each tackling a unique, authentic issue from professional practice or research groups.
Implications for Practice
In the dynamic landscape of population health and demographics, pertinent healthcare and social work skills and adaptability of (future) healthcare professionals are of utmost importance for innovation in healthcare and social work practices. In this article we briefly explored select innovative approaches in education that can educate and train future-proof healthcare professionals who are ready for rapidly evolving health systems. We considered innovative teaching approaches from Canada, Netherlands, and the US that focused on how 21st century skills are integrated into the curriculum and education programs; professional development; and learning environments. Our examples showed that complex societal challenges (i.e., wicked or stubborn problems) were the starting point for both educational modules and programs and for innovation in practice.
Future-proof professionals need to develop skills in the integration of diverse perspectives and expertise for comprehensive and effective solutions. Hence, we see the transition from monodisciplinary to multidisciplinary and interdisciplinary collaboration to reshape education and learning environments. Educational institutions play a critical role in this healthcare and technology transformation, preparing students for emerging professions and equipping them with the necessary competencies (Endalamaw et al., 2024). The study route “Health & Technology” program within a nursing program in the Netherlands illustrated how education can lead the way to reshape emerging professions.
A fundamental aspect of fostering innovation is the acceptance of “not knowing” and even failure as an integral part of the process.
A fundamental aspect of fostering innovation is the acceptance of “not knowing” and even failure as an integral part of the process. However, educators may not be trained or prepared to move from a didactic teaching model to a more exploratory and learning model. They may need additional training and practice to try (and fail) to become comfortable with the ambiguity of innovation and explorations. Embracing failure allows students and teachers to experiment, learn, and ultimately achieve successful innovations and practice improvements.
Innovation in healthcare requires a multi-level and interdisciplinary approach, involving national agencies, state ambitions, and collaboration with educational institutions and healthcare organizations (Endalamaw et al., 2024). Integrating innovation into educational programs is crucial to prepare future professionals for the evolving demands of the healthcare sector, including population and demographic changes, and evolving technologies. Educators, both teachers and professionals, are key players in this transition. They must be innovative, tech-savvy, and ready to embrace uncertainty. Their role is to prepare students for their future professions by equipping them with the necessary skills and knowledge to adapt to new technologies and methodologies (den Ouden & Groeneveld, 2023; Frith, 2020).
A critical discussion is needed about the future role of innovation and emerging technologies within healthcare.
A critical discussion is needed about the future role of innovation and emerging technologies within healthcare. It is essential to define the complementary aspects of professional practice and technology (Groeneveld et al., 2024). An understanding of this relationship will help in designing educational programs that prepare professionals to work alongside technology effectively.
As one of the 21st century skills, leadership plays a crucial role in the innovation and implementation of technology in healthcare and social work (European Centre for Development, 2012). Technology is perceived as one of the solutions for challenges regarding the aging population, with a higher number of chronic diseases, and staff shortages. However, distinguishing between technology that is seen as mere gadgets versus technology as a meaningful care intervention is important (Groeneveld et al., 2024). Part of the solution is to engage end-users (both professionals and patients/clients) in the development of technologies. Engaging end-users in the design and development process is essential to create effective and user-friendly solutions (Leary et al., 2022). Otherwise, missing this important input can lead to the creation of technologies that are difficult to use or do not meet the actual needs of users.
...distinguishing between technology that is seen as mere gadgets versus technology as a meaningful care intervention is important
Future-proof professionals must learn to critically evaluate new technologies for their user-population to ensure that they genuinely enhance (social) care rather than simply adding complexity or additional costs to the care process. This distinction is vital to avoid adopting technologies that do not contribute to improved health outcomes. Leaders are pivotal in the transformation process, guiding the selection and implementation of technologies and innovations (Atkinson & Singer, 2021; Oskarsson & Vik, 2024). Their role includes fostering a culture of innovation, encouraging colleagues to embrace new technologies, and ensuring that these technologies are used effectively and ethically.
In sum, there is a need to strengthen innovative work across various professions such as nursing, social work, and occupational therapy. This effort includes fostering a culture of innovation, providing resources and support for innovative projects that may need to go through multiple iterations (“fail fast”), and encouraging collaboration among different disciplines. Our examination of the features of innovation success in different countries and professions has provided valuable insights. Identifying shareable and adoptable features and skills between innovation initiatives can help to create more effective and scalable solutions.
...it is essential to focus on collaboration, leverage local resources, and engage/work together with the community and region.
Our examples showed that these initiatives for innovation cannot be unique to one discipline; the role of academic institutions, government, and the surrounding ecosystem (e.g., healthcare organizations) is crucial in fostering innovation. These entities must work together to create an environment that supports and encourages innovation in healthcare. The described best practice Smart Solutions Semester showed the added value of real-life assignments for students and their added value/thinking power to come up with innovative solutions for health and welfare organizations and companies. For aspiring innovators, it is essential to focus on collaboration, leverage local resources, and engage/work together with the community and region.
Conclusion
Future-proof healthcare professionals must critically evaluate technologies to ensure that they enhance care. These professionals need to build skills in the integration of diverse perspectives and expertise to develop comprehensive and effective solutions. Collaboration between educational institutions and practice environments does and will play a critical role in preparing students for integration of emerging technologies within their professions to equip them with the necessary 21st century leadership skills. Hence, integration of the Partnership for 21st Century Learning framework (Network for BattelleforKids, 2019) categories of curriculum and instruction, professional development, and learning environments can provide a rich, sustainable, and challenging pathway to innovation for healthcare educators and their students.
Authors
Marjolein E.M. den Ouden, PhD
Email: m.e.m.denouden@saxion.nl
ORCID ID: 0000-0001-7821-1578
M.E.M. den Ouden (Marjolein) is professor Technology, Health & Care at Saxion University of Applied Sciences and the Regional Community College Twente. She has a background in epidemiology (MSc, PhD) and human movement sciences (MSc). She is an expert in human centered technology development, the acceptance and implementation of technology and the technology competences of (future) professionals. As a PI/work package leader she contributes to various (inter)national research projects and contributes as an expert to the Dutch Mission Driven Innovation and Research Agenda of The Netherlands.
Sjors Groeneveld, MSc
Email: s.w.m.groeneveld@saxion.nl
ORCID ID: 0000-0003-3942-9691
S.W.M. Groeneveld (Sjors) is a senior lecturer Living Technology at Saxion University of Applied Sciences and PhD candidate AI in long term care at the University of Twente. Sjors is involved in various Dutch national initiatives focused on the role of technology in healthcare education, is an educational author and speaks and publishes about the influence of technology on the competences of (future) healthcare professionals.
Monique M.J. Engelbertink, PhD
Email: m.m.j.engelbertink@saxion.nl
ORCID ID: 0000-0003-2246-436X
M.M.J. Engelbertink (Monique) is an associate lector at Saxion University of Applied Sciences. Her research line focuses on preventing and supporting psychosocial stress and mental complaints within the social work domain. She teaches at the master's program Health Care and Social Work.
AkkeNeel Talsma, PhD, RN, FAAN
Email: Talsma@uwm.edu
ORCID ID: 0000-0001-6110-926X
AkkeNeel Talsma is an Associate Professor of Nursing and a Kellner Entrepreneurship Fellow at the University of Wisconsin Milwaukee (UWM) College of Health Sciences and Professions, School of Nursing. Dr. Talsma has extensive experience developing and evaluating quality and safety interventions. Her work includes the introduction of innovation into the nursing curriculum and has developed her own healthcare technology related innovations benefiting maternal health and surgical outcomes. Dr. Talsma is further supporting innovation as an NSF-I-Corps mentor.
Adriana Ríos Rincón, PhD, OT (Reg. AB)
Email: aros@ualberta.ca
ORCID ID: 0000-0002-9018-9761
A.M. Ríos Rincón (Adriana) is an Assistant Professor in the Department of Occupational Therapy at the University of Alberta. Her research focuses on using advanced technologies to support aging in place and facilitate transitions across the continuum of care for older adults. She also investigates how technology can assess and enhance cognitive skills, promoting engagement in cognitive activities for older adults, including those living with dementia. Additionally, Dr. Rios Rincón leads the implementation of strategies to develop digital skills in occupational therapy students, ensuring they are prepared for the future of healthcare technology.
Lili Liu, PhD, (OT Reg)
Email: lili.liu@uwaterloo.ca
ORCID ID: 0000-0001-7082-4898
Lili Liu is professor in the School of Public Health Sciences, and dean of the Faculty of Health at the University of Waterloo. Liu’s research program examines acceptance and adoption of technology innovations by older adults, their partners, health care professionals, and unlicensed care personnel. Her research informs policies that create safe environments for older adults living with dementia at risk of going missing.
References
Amankawaa, I., Boateng, D., Quansah, D. Y., Akuoko, C. P.., Desu, A. P. B., & Hales, C. (2022). Innovations in nursing education in response to the Covid-19 pandemic: A scoping review. Nursing Praxis Aotearoa New Zealand, 38(3), 1-16. https://doi.org/10.36951/001c.55768
American Association of Colleges of Nursing. (2021). The Essentials: Core competencies for professional nursing education. https://www.aacnnursing.org/Portals/0/PDFs/Publications/Essentials-2021.pdf
Atkinson, M. K., & Singer, S. J. (2021). Managing organizational constraints in innovation teams: A qualitative study across four health systems. Medical Care Research and Review, 78(5), 521-536. https://doi.org/10.1177/1077558720925993
Aykan, E. B., Fidanci, B. E., & Yildiz, D. (2022). Evaluation of entrepreneurship, individual innovation and obstacles to innovation in nursing students. International Journal of Caring Sciences, 15(3), 1792-1798. https://www.researchgate.net/publication/370214188_Evaluation_of_Entrepreneurship_Individual_Innovation_and_Obstacles_to_Innovation_in_Nursing_Students
BattelleforKids. (2019). Framework for 21st century learning definitions. https://static.battelleforkids.org/documents/p21/p21_framework_definitionsbfk.pdf
Bier, N., Auger, C., Bottari, C. & Demers, L. (2022). Promoting occupational participation through assistive technology. In: Egan & Restall. Promoting occupational Participation: Collaborative relationship-focused occupational therapy. CAOT/ACE.
Blouin, A. S. (2023). Innovations in nursing workforce management: integrating emerging technologies with proven strategies. JONA: The Journal of Nursing Administration, 53(11), 601-606. https://doi.org/10.1097/nna.0000000000001352
Bouwes, A., Broekman H., Dobber, J., Eisenberg, I., Den Hertog, R., & Rutgers, A. (2023). National Educational Profile Bachelor 2030, The Hague. https://www.loov-hbov.nl/wp-content/uploads/2023/11/2023-10-30-BN2030.pdf
Czuba, K. J., Vandal, A. C., Czuba, F. M., & Kayes N. M. (2023). The effectiveness of peer-led interventions to improve work-related psychosocial outcomes and reduce turnover of support workers in residential aged care: A systematic review and meta-analysis. International Journal of Nursing Studies Advances, 5, 100158. https://doi.org/10.1016/j.ijnsa.2023.100158
Den Ouden, M. E. M., & Groeneveld, S. (2023). V-Model shows technology competences of healthcare and social work professionals. ICT&Health. https://icthealth.nl/magazine/editie-02-2023/v-model-toont-competenties-zorg-en-welzijnsprofessionals-in-omgang-met-technologie
Endalamaw, A., Khatri, R. B., Erku, D., Zewdie, A., Wolka, E., Nigatu, F., & Assefa, Y. (2024). Barriers and strategies for primary health care workforce development: synthesis of evidence. BMC Primary Care, 25, 99. https://doi.org/10.1186/s12875-024-02336-1
European Centre for the Development of Vocational Training (Cedefop). (2012). Revised Edition 2013. Publications Office of the European Union. ISB978-92-896-1358-3.
Frith, K. H. (2020). Design thinking: An approach to innovative interprofessional education. Nurings Education Perspectives, 41(1), 69. https://doi.org/10.1097/01.Nep.0000000000000629
Groeneveld, S., Bin Noon, G., den Ouden, M. E. M., van Os-Medendorp, H., van Gemert-Pijnen, J. E. W. C., Verdaasdonk, R. M., & Morita, P. P. (2024). The cooperation between nurses and a new digital colleague "AI-Driven Lifestyle Monitoring" in long-term care for older adults: Viewpoint. JMIR Nursing, 7, e56474. https://doi.org/10.2196/56474
Hagle, M., Dwyer, D., Gettrust, L., Lusk, D., Peterson, K., & Tennies, S. (2020). Development and implementation of a model for research, evidence-based practice, quality improvement, and innovation. Journal of Nursing Care Quality, 35(2), 102-107. https://doi.org/10.1097/ncq.0000000000000422
Leary, M., Villarruel, A. M., & Richmond, T. S. (2022). Creating an innovation infrastructure in academic nursing. Journal of Professional Nursing, 38, 83-88. https://doi.org/10.1016/j.profnurs.2021.12.005
Leary, M., & Burger, A. (2022). Requiring design thinking in nursing curriculum. American Nurse. https://www.myamericannurse.com/my-nurse-influencers-requiring-design-thinking-in-nursing-curriculum/
Liu, L., Lederer, R., & Amell, T. (2001, September 12- 14). Improving the fit between products and an aging population. International Conference on Technology and Aging, Toronto, Ontario.
Liu, L., & Lederer, R. (2009). Aging and ergonomics. In S. Kumar (Ed.), Rehabilitation and Ergonomics (pp. 103-133). Routledge.
Liu, L. (2018). Muriel Driver Lecture (Keynote) – Occupational therapy in the fourth industrial revolution. Canadian Journal of Occupational Therapy, 85(4), 272-285. https://doi.org/10.1177/0008417418815179
National Academies of Sciences, Engineering, and Medicine. (2021). The future of nursing 2020-2030: Charting a path to achieve health equity. The National Academies Press. https://doi.org/10.17226/25982
National Academies of Sciences, Engineering, and Medicine. (2007). The learning healthcare system: Workshop summary. The National Academies Press. https://doi.org/10.17226/11903
Oskarsson, I. M. L., & Vik, E. (2024). Suggesting a holistic framework for understanding healthcare services leadership competence - A critical interpretive synthesis. Leadership in Health Services (Bradford, England), 37(5), 99–129. https://doi.org/10.1108/lhs-08-2023-0059
Roller-Wirnsberger, R., Lindner, S., Liew, A., O'Caoimh, R., Koula, M. L., Moody, D., Espinosa, J. M., van Durme, T., Dimitrov, P., Benjak, T., Nicolaidou, E., Hammar, T., Vanhecke, E., Junius-Walker, U., Csizmadia, P., Galluzzo, L., Macijauskienė, J., Salem, M., Rietman, L., … Rodriguez-Mañas, L. (2020). European Collaborative and Interprofessional Capability Framework for Prevention and Management of Frailty-A consensus process supported by the Joint Action for Frailty Prevention (ADVANTAGE) and the European Geriatric Medicine Society (EuGMS). Aging Clinical and Experimental Research, 32(4), 561–570. https://doi.org/10.1007/s40520-019-01455-5
Segal, A., & Doyle, N. W. (2024). Technology trends in practice: A survey of occupational therapy practitioners. Work, 79(3), 1069–1078. https://doi.org/10.3233/WOR-230654
Snow, F. (2019). Creativity and innovation: An essential competency for the nurse leader. Nursing Administration Quarterly, 43(4), 306-312. https://doi.org/10.1097/naq.0000000000000367
Talsma, A. N., Holt, J. M., Lloren, J. I., Klingbeil, C., Taani, M., & Avdeev, I. (2025). Evaluation of synchronous online “Innovation and Design Thinking Module” in graduate nursing. OJIN: The Online Journal of Issues in Nursing. https://doi.org/10.3912/OJIN.Vol30No01Man03
UNESCO-UNEVOC International Centre for Technical and Vocational Education and Training. (2022). Handbook for the UNEVOC Network. UNESCO. Bonn, Germany.
U. S. National Science Foundation. (n.d.). NSF’s innovation corps (I-Corps). Major Initiatives. https://new.nsf.gov/funding/initiatives/i-corps
White, K. R., Pillay, R., & Huang, X. (2016). Nurse leaders and the innovation competence gap. Nursing Outlook, 64(3), 255-261. https://doi.org/10.1016/j.outlook.2015.12.007
World Health Organization. (2015). World reporting on ageing and health. https://www.who.int/publications/i/item/9789241565042/


