Stethoscope hygiene is rarely performed despite evidence that they are a potential source of nosocomial infections. Aseptic touch-free disposable stethoscope diaphragm barriers (touch-free barriers) provide a bacteriologically impervious surface; however, little is known about perceptions of touch-free barriers. The purpose of this study was to determine patients’ and healthcare professionals’ perceptions of stethoscope hygiene habits, cleanliness, and patient safety, after respondents viewed videos of stethoscope hygiene with alcohol versus a touch-free barrier, or no hygiene/no barrier. We conducted a cross-sectional study using survey methodology and convenience sampling. Participants viewed three short videos that showed a provider using each of three stethoscope hygiene techniques (barrier, alcohol, or none), followed by completion of a brief survey. Pearson’s chi-square, Fisher’s exact, Wilcoxon rank sum or Kruskal-Wallis tests were used as appropriate. Bonferroni correction was used to control error rate at 0.05 for each question. The sample size of 240 participants included 119 patients and 121 healthcare professionals. Patients rarely witnessed healthcare professionals cleaning stethoscopes, rated clean stethoscopes as important, and were more likely to choose touch-free barrier as easiest for providers. Healthcare professionals rated stethoscope hygiene as important, reported frequent stethoscope hygiene, and felt that touch-free barrier would improve workflow. Touch-free barriers were viewed positively by respondents. Hospitals should consider touch-free barriers as an important strategy to reduce nosocomial infections.
Key Words: stethoscope, aseptic, hospital-acquired infections, patient safety
Background
...stethoscope hygiene is rarely performed despite the fact that stethoscopes carry a similar bacterial load compared to hands.The United States Centers for Disease Control and Prevention ([CDC], 2021) reported 687,000 healthcare-associated infections (HAI) in 2015 and estimated that at least 300,000 people in long term care facilities died as a result in 2017 (Centers for Medicare and Medicaid Services, 2017). Thus, prevention of HAI is of paramount importance. Handwashing has been the accepted practice for preventing HAI for over a century (Tyagi & Barwal, 2020); however, stethoscope hygiene is rarely performed despite the fact that stethoscopes carry a similar bacterial load compared to hands (Longtin et al., 2014; Boulée et al., 2019).
...researchers have consistently reported low observed stethoscope disinfection rates...Some of the most recurrent pathogens found on stethoscope diaphragms included Pseudomonas; vancomycin-resistant Enterococci; Clostridioides difficile (c-diff) (O'Flaherty & Fenelon, 2015); Staphylococcus aureus; Acinetobacter spp; and Klebsiella pneumoniae (Bansal et al., 2019; Datta et al., 2018; Queiroz Júnior et al., 2021). Even so, researchers have consistently reported low observed stethoscope disinfection rates, in the range of 5-18% (Boulée et al., 2019; Holleck et al., 2020; Jenkins et al., 2015; Rao et al., 2017). Self-reported rates of hygiene commonly exceed 85% (Alali et al., 2020). In a recent report of contamination rates among nursing students’ stethoscopes, researchers found 29.9% of stethoscope diaphragms were contaminated with bacteria, 5.1% of which was c-diff and e-coli (Gaisser et al., 2021). Further, it has been shown that stethoscope hygiene does not kill all pathogens, as c-diff is particularly resistant to alcohol (Alali et al., 2020; Jabbar et al., 2010). Aseptic touch-free applied disposable stethoscope diaphragm barriers provide a bacteriologically impervious surface and a possible reduction in stethoscope-to-patient, and patient-to-patient, spread of c-diff and other pathogens (Peacock et al., 2021).
Overall, avoiding contaminated surfaces appears important to patients.More research is needed to identify stethoscope hygiene methods that healthcare professionals perceive as acceptable. Prior to the current study, little was known about patients’ and healthcare professionals’ perceptions of aseptic, touch-free applied, disposable stethoscope diaphragm barriers (hereafter referred to as stethoscope diaphragm barriers) for the purpose of reducing pathogen spread from contaminated stethoscopes. Overall, avoiding contaminated surfaces appears important to patients. In a 2021 narrative review, researchers reported that cleanliness of the hospital environment was an important factor related to patient satisfaction (Guerra-Martín & González-Fernández, 2021).
Aseptic touch-free applied disposable stethoscope diaphragm barriers provide a bacteriologically impervious surface...There is a lack of research addressing patient perceptions about the importance of stethoscope cleanliness. In addition, there is still much to learn about healthcare professionals’ perceptions of the stethoscope as a pathogen harboring instrument, and its role in patient safety. The purpose of this study was to survey patients and healthcare professionals after they viewed videos of stethoscope hygiene performed with 70% isopropyl alcohol (alcohol) versus a stethoscope diaphragm barrier, or no hygiene/no barrier. We sought to determine their perceptions of stethoscope hygiene habits, cleanliness and patient safety related to stethoscope hygiene, ease of use, and hygiene compliance,
Research Methods
Design
We conducted a single center cross-sectional study using standard survey methodology and convenience sampling of patients and healthcare professionals. The study received approval from the hospital institutional review board (IRB), the Chief Nursing Officer and the Vice Chair of Research, and the departments of internal medicine and geriatrics to survey nurses and physicians. This study took place at the main campus of a large quaternary care center in the Midwest United States. Sampling occurred in the outpatient surgical waiting area (for patients, family members, and visitors); various inpatient and outpatient nursing units (for nurses and mid-level practitioners); and in outpatient internal medicine offices (for physicians). A waiver of informed consent was granted by the IRB.
Sample
This study included two sample populations. Patients who had been treated in a clinic or doctor’s office within the last six months were the first cohort, and this included adult patients, their family members, and their visitors. Recruitment and data collection took place in outpatient clinics and the outpatient surgery waiting area on the hospital main campus. Participants needed to be able see (for video viewing) and to read and understand English to complete the surveys. There were no other exclusion criteria for this sample.
The second cohort was healthcare professionals in both outpatient and inpatient settings at the hospital’s main campus who regularly used a stethoscope in practice. This included licensed practical nurses, registered nurses, and advanced practice registered nurses (APRNs) employed throughout the main campus. Additionally, physicians acting as resident preceptors and resident physicians in the outpatient internal medicine clinic, and physician’s assistants, were included. No exclusions applied and no incentive was provided for either cohort for participation.
Sample size calculations were based on detecting a 20% difference between groups based on a binary question, and medium effect sizes. A sample size of 200 patients and healthcare professionals (100 per cohort) allowed for 80% power to detect effect sizes of 0.4 (10 point or larger differences on a continuous visual analogue scale [VAS]), and 20% or greater differences on binary questions. An additional 20% (240 total participants) were included to account for missing data. Sample size calculations assumed two-sided Chi-square tests for categorical variables and two-sided two-sample t-tests for continuous measures, with significance defined as p<0.05.
Data Collection
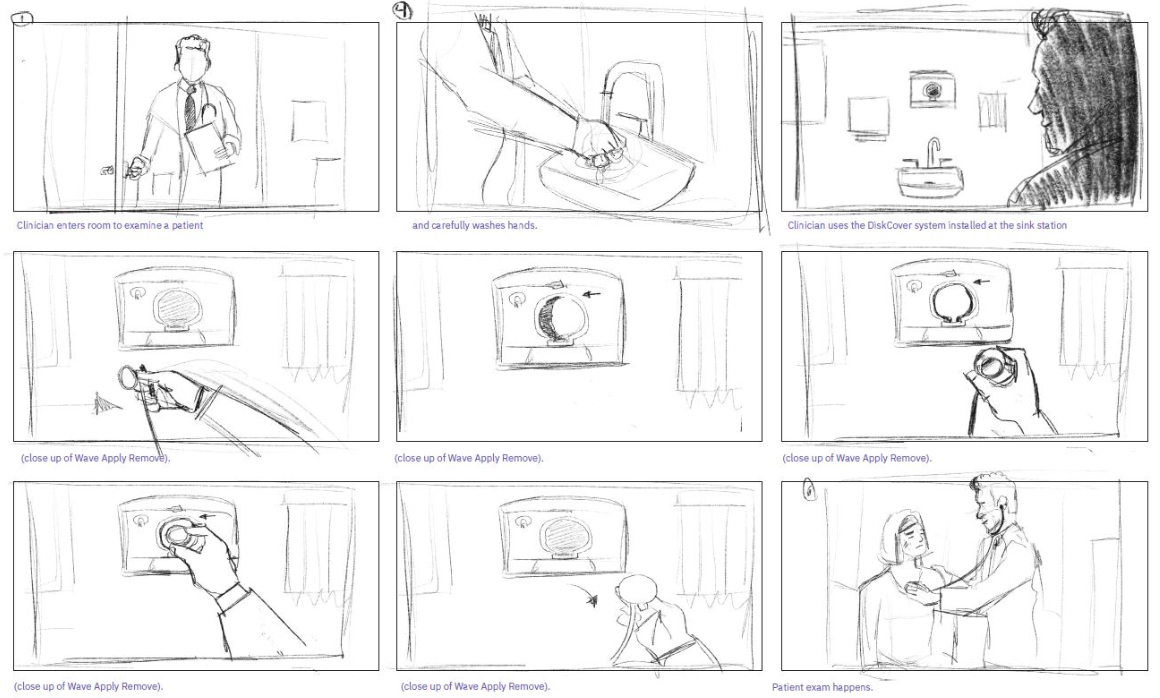
Instrumentation. Two investigator-created surveys (one for patients and one for healthcare professionals) were used to assess perceptions of stethoscope hygiene habits, patient safety, ease of use, and compliance of stethoscope hygiene. The comparison was alcohol to a touch-free barrier (Aseptiscope, Inc, San Diego, CA – DiskCover System, n.d.) (see Figure 1), and control (no cleaning or barrier). Prior to the surveys, participants viewed three short videos showing a healthcare provider using each of the three techniques. No conversation was used in the videos; there was background music. Videos were viewed in random order; both cohort participants viewed the same videos. These videos were created for the purpose of this research and specifically included all three hygiene techniques. Each video was developed from the same story board; these were identical except for the stethoscope hygiene technique. Figure 2 illustrates a rough drawing used in the video planning in which the provider used the touch-free barrier. Videos were provided in person; a data collector was present to ensure that all were viewed and presented in random order, followed by the survey completion.
Figure 1. Touch-free Barriers

(DiskCover System, n.d.; Aseptiscope, Inc, San Diego, CA).
Figure 2. Story Board Used for Videos
Procedures. For the patient cohort, data collectors approached eligible family members and visitors in hospital waiting areas throughout the main campus of the hospital. Data collectors waited near the outpatient surgery check-in desk and offered an information flyer about the study. They then approached family members and visitors in the surgical waiting area who were previously given an information flyer, confirmed that they were not a surgical patient, and that they had a visit with a provider in the last six months. No patients were approached in the surgical waiting area. Patients were approached in outpatient clinic areas throughout the main campus near the registration desk and given an information flyer. Data collectors then followed-up after patients had completed their appointments with their providers, and asked the patients if they would be interested in participating.
For candidates who agreed to participate, to ensure privacy we provided a quiet place in the waiting area, or in a clinic office/room as needed. The participant then viewed the videos in random order via an iPad. Each video took 1 ½ -2 ¼ minutes to watch (total time was approximately five minutes). Participants then completed the patient survey, also via an iPad.
For the healthcare professional cohort, data collectors approached these employees to ask if they would be interested in watching a brief video and taking a short survey. They were invited to participate, either via email or in person. If needed, we arranged a convenient time to view the videos and complete the survey. The video viewing and survey completion process was similar to the patient cohort.
Statistical Analyses
Categorical variables were described using frequencies and percentages and presented with 95% confidence intervals (95% CI). Comparisons were analyzed using Pearson’s chi-square or Fisher’s exact tests for unordered factors, and Wilcoxon rank sum tests or Kruskal-Wallis tests were used for ordered variables. Continuous variables were described using medians and quartiles; comparisons used Wilcoxon rank sum tests or Kruskal-Wallis tests. Pairwise comparisons, using a Bonferroni correction, were performed whenever 3-group comparisons were significant overall. Comparisons of levels within questions were performed among all responders using binomial tests to determine if the frequency of responses was equal between levels. Wilcoxon signed rank tests were used to assess whether scale responses differed from the midpoint of 50 on a 0-100 scale. These analyses used a Bonferroni correction to control the overall error rate at 0.05 for each question. Analyses used SAS® Software (version 9.4; Cary, NC).
Results
There were 240 total records in the dataset. Of these, 119 were from the patient cohort and the remaining 121 were provided by healthcare professionals.
Patient Cohort
The patient cohort was categorized as patients (n = 44) and others (n = 75). Patients were more likely to indicate that they currently had a chronic condition that affected their immune system or had an open wound or burn above the waist, compared to others (p<0.001). Of the group, over a third [n (%)] of the cohort were immune compromised or had open wounds or burns [39 (33.1)].
Witnessed stethoscope hygiene practices were rare.Witnessed stethoscope hygiene practices were rare. Overall, only 5% (95% CI = 1.9 to 10.6%) of respondents reported seeing the provider clean their stethoscope before every contact, with the most common answer to the question of “how often had they witnessed stethoscope hygiene” being “unsure” (reported in 37.8%; 95% CI = 29.1 to 47.2%). Stethoscope hygiene was witnessed as only “sometimes” or “always” in a minority of cases (42%, 95% CI = 33.0 to 51.0%), which was similar to the most common report of “unsure”, “never”, or “rarely” (total = 58%; 95% CI= 48.6 to 67.0%). Ultimately, considering that some respondents indicated they were “unsure” if the stethoscope was clean, thus representing contaminated diaphragms, the odds of an unclean stethoscope contact would be more likely than not.
When stratified by the “patient only” subset, patients were more likely to say that they saw their healthcare provider clean their diaphragm than others (p = 0.025). Only 9.1% of the patient group reported witnessing stethoscope hygiene every time, while 47.7% indicated that they saw it “sometimes”, with the remainder (43.3%) seeing stethoscope hygiene unsure/never/rarely (see Table 1).
Table 1. Patients and Others (Family and Visitors) Comparisons on Survey Questions
|
Overall |
Other |
Patient |
|||||
|---|---|---|---|---|---|---|---|
|
Factor |
N |
Statistics |
N |
Statistics |
N |
Statistics |
P-value |
|
Before a healthcare professional touches my body with their stethoscope, I observe them cleaning the diaphragm (the part that touches your skin) with alcohol, n (%) |
119 |
75 |
44 |
0.025b |
|||
|
Unsure |
45 (37.8) |
32 (42.7) |
13 (29.5) |
||||
|
Never |
16 (13.4) |
12 (16.0) |
4 (9.1) |
||||
|
Rarely |
8 (6.7) |
6 (8.0) |
2 (4.5) |
||||
|
Sometimes |
44 (37.0) |
23 (30.7) |
21 (47.7) |
||||
|
Every time |
6 (5.0) |
2 (2.7) |
4 (9.1) |
||||
|
On a scale of 0-100 (0 = not important at all, 100 = critically important), the need for healthcare professionals to clean the diaphragm of the stethoscope before it touches my skin is, median [Q1, Q3] |
118 |
92.5 [50.0, 100.0] |
75 |
80.0 [50.0, 100.0] |
43 |
100.0 [50.0, 100.0] |
0.40b |
|
Of the 2 stethoscope hygiene approaches (alcohol swab cleaning or touch free barrier) that I watched, the following would be easiest for my healthcare professional to use, n (%) |
119 |
75 |
44 |
0.78b |
|||
|
1. Touch Free Barrier |
98 (82.4) |
62 (82.7) |
36 (81.8) |
||||
|
2. Neither |
5 (4.2) |
5 (6.7) |
0 (0.00) |
||||
|
3. Alcohol Swab Cleaning for 60-seconds |
16 (13.4) |
8 (10.7) |
8 (18.2) |
||||
|
Provides me with visual evidence of a clean stethoscope, n (%) |
119 |
75 |
44 |
0.15d |
|||
|
Touch Free Barrier ONLY |
23 (19.3) |
18 (24.0) |
5 (11.4) |
||||
|
Alcohol Swab Cleaning for 60-seconds ONLY |
29 (24.4) |
14 (18.7) |
15 (34.1) |
||||
|
Neither |
3 (2.5) |
2 (2.7) |
1 (2.3) |
||||
|
Both ALCOHOL AND TOUCH FREE |
64 (53.8) |
41 (54.7) |
23 (52.3) |
||||
|
Increases my comfort in having the healthcare professional use a stethoscope on my skin, n (%) |
119 |
75 |
44 |
0.48c |
|||
|
Touch Free Barrier |
20 (16.8) |
15 (20.0) |
5 (11.4) |
||||
|
Alcohol Swab Cleaning for 60-seconds |
31 (26.1) |
19 (25.3) |
12 (27.3) |
||||
|
Both |
68 (57.1) |
41 (54.7) |
27 (61.4) |
||||
|
Most positively affects MY SAFETY, n (%) |
116 |
72 |
44 |
0.10b |
|||
|
1. Touch Free Barrier application |
28 (24.1) |
18 (25.0) |
10 (22.7) |
||||
|
2. Stethoscope hygiene does not maintain patient safety |
18 (15.5) |
16 (22.2) |
2 (4.5) |
||||
|
3. Alcohol Swab Cleaning for 60 seconds |
70 (60.3) |
38 (52.8) |
32 (72.7) |
||||
|
Is the best way to show me that the stethoscope was cleaned before use, n (%) |
119 |
75 |
44 |
0.43d |
|||
|
Touch Free Barrier |
20 (16.8) |
14 (18.7) |
6 (13.6) |
||||
|
Alcohol Swab Cleaning for 60-seconds |
49 (41.2) |
27 (36.0) |
22 (50.0) |
||||
|
Neither |
2 (1.7) |
2 (2.7) |
0 (0.00) |
||||
|
Both |
48 (40.3) |
32 (42.7) |
16 (36.4) |
||||
|
Statistics presented as Median [P25, P75], N (column %). |
|||||||
...the patient cohort perceived the importance of a clean stethoscope as more important than not...When rated on a scale of 0-100 (0 = not important at all, 100 = critically important), the patient cohort perceived the importance of a clean stethoscope as more important than not (when testing response difference from 50; midpoint of the range) (p<0.001). For visual evidence of a clean stethoscope, they were more likely to answer “both” touch free barrier and witnessed alcohol cleaning over any single method of touch free barrier or alcohol (p<0.001) and were least likely to answer neither (p<0.001). When asked which method “increased comfort” when healthcare professionals used a stethoscope on their skin, respondents were more likely to answer “both” (i.e., either touch free barrier or alcohol) rather than one method or the other (p<0.001). There was no significant difference between touch free barrier and alcohol related to increased comfort. Respondents were more likely to choose alcohol cleaning over touch free barrier for which most positively affects their safety (p<0.001).
There was no significant difference between touch free barrier and alcohol related to increased comfort.Of the 2 stethoscope hygiene approaches (alcohol cleaning or touch free barrier), the patient cohort was more likely to choose the touch free barrier rather than the option of neither or alcohol cleaning (p<0.001) as easier for their provider to use. They were also more likely to choose alcohol cleaning compared to neither (p<0.016).
Healthcare Professionals Cohort
Healthcare professionals were categorized as nurses (n = 89), mid-level practitioners (Physicians Assistants and APRNs) (n = 24), and physicians (n = 8) for a total sample of 121. There were no significant differences between groups on any of the questions (see Table 2).
Table 2. Healthcare Professionals Group Comparisons on Survey Questions
|
Overall |
RN, LPN |
PA, APRN |
Physician |
||||||
|---|---|---|---|---|---|---|---|---|---|
|
Factor |
N |
Statistics |
N |
Statistics |
N |
Statistics |
N |
Statistics |
P-value |
|
How often do you clean your stethoscope diaphragm with alcohol for 60 seconds? , n (%) |
121 |
89 |
24 |
8 |
0.37b |
||||
|
Never |
7 (5.8) |
4 (4.5) |
2 (8.3) |
1 (12.5) |
|||||
|
Weekly |
6 (5.0) |
3 (3.4) |
2 (8.3) |
1 (12.5) |
|||||
|
Daily |
21 (17.4) |
19 (21.3) |
1 (4.2) |
1 (12.5) |
|||||
|
Between every few patients |
36 (29.8) |
29 (32.6) |
5 (20.8) |
2 (25.0) |
|||||
|
Between every patient |
51 (42.1) |
34 (38.2) |
14 (58.3) |
3 (37.5) |
|||||
|
Which approach would be the easiest for your work flow? , n (%) |
121 |
89 |
24 |
8 |
0.11b |
||||
|
1. Touch Free Barrier |
89 (73.6) |
68 (76.4) |
14 (58.3) |
7 (87.5) |
|||||
|
2. Neither |
7 (5.8) |
6 (6.7) |
1 (4.2) |
0 (0.00) |
|||||
|
3. Alcohol Swab Cleaning for 60 seconds |
25 (20.7) |
15 (16.9) |
9 (37.5) |
1 (12.5) |
|||||
|
If a touch free barrier was available, would your stethoscope hygiene compliance change? , n (%) |
121 |
89 |
24 |
8 |
0.11b |
||||
|
Significantly worsen compliance |
1 (0.83) |
1 (1.1) |
0 (0.00) |
0 (0.00) |
|||||
|
Slightly worsen compliance |
3 (2.5) |
1 (1.1) |
2 (8.3) |
0 (0.00) |
|||||
|
No impact |
39 (32.2) |
28 (31.5) |
10 (41.7) |
1 (12.5) |
|||||
|
Slightly improve compliance |
45 (37.2) |
33 (37.1) |
8 (33.3) |
4 (50.0) |
|||||
|
Significantly improve compliance |
33 (27.3) |
26 (29.2) |
4 (16.7) |
3 (37.5) |
|||||
|
Which stethoscope hygiene strategy would most positively affect patient safety? , n (%) |
119 |
87 |
24 |
8 |
0.80b |
||||
|
1. Touch Free Barrier application |
38 (31.9) |
30 (34.5) |
5 (20.8) |
3 (37.5) |
|||||
|
2. Stethoscope hygiene does not maintain patient safety |
23 (19.3) |
15 (17.2) |
7 (29.2) |
1 (12.5) |
|||||
|
3. Alcohol Swab Cleaning for 60 seconds |
58 (48.7) |
42 (48.3) |
12 (50.0) |
4 (50.0) |
|||||
|
On a scale of 1-100, rate importance of stethoscope hygiene?, median [Q1, Q3] |
118 |
80.0 [50.0, 95.0] |
88 |
80.0 [50.0, 97.5] |
22 |
75.0 [50.0, 90.0] |
8 |
90.0 [75.0, 95.0] |
0.36b |
|
Do you think a stethoscope hygiene strategy could improve patient satisfaction? , n (%) |
120 |
88 |
24 |
8 |
0.12b |
||||
|
0. No |
37 (30.8) |
27 (30.7) |
9 (37.5) |
1 (12.5) |
|||||
|
1. Unsure |
39 (32.5) |
27 (30.7) |
10 (41.7) |
2 (25.0) |
|||||
|
2. Yes |
44 (36.7) |
34 (38.6) |
5 (20.8) |
5 (62.5) |
|||||
|
Which hygiene strategy would provide the greatest improvement in patient satisfaction? , n (%) |
44 |
34 |
5 |
5 |
0.41b |
||||
|
1. Touch Free Barrier Application |
16 (36.4) |
11 (32.4) |
3 (60.0) |
2 (40.0) |
|||||
|
2. Both, equally |
25 (56.8) |
20 (58.8) |
2 (40.0) |
3 (60.0) |
|||||
|
3. Alcohol Swab Cleaning for 60 seconds |
3 (6.8) |
3 (8.8) |
0 (0.00) |
0 (0.00) |
|||||
|
Statistics presented as Median [P25, P75], N (column %). PA=Physicians Assistant APRN=Advanced Practice Registered Nurse |
|||||||||
On a scale of 1-100 (1 = not important at all, 100 = critically important), respondents rated the need for healthcare professionals to perform some type of stethoscope hygiene as more important than not (test of whether the response differed from 50; midpoint of the range) (p<0.001). When asked how often they cleaned their stethoscope diaphragm with alcohol for 60 seconds as recommended by the CDC, respondents were more likely to choose “between every patient or between every few patients” compared to other options (p<0.001), and daily compared to weekly (p=0.004). When compared to no stethoscope hygiene, respondents perceived that alcohol would positively affect patient safety (p<0.001). Overall, respondents chose touch free barrier and alcohol cleaning for 60 seconds at similar rates for impact on patient safety (p=0.041).
In response to which of the two stethoscope hygiene approaches (i.e., alcohol swab for 60 seconds or touch free barrier) would be easier for their workflow, respondents were markedly more likely to choose the touch free barrier over alcohol swabbing (73.6 versus 20.7%, p<0.001, respectively). Respondents were more likely to choose “slightly or significantly improve” (82%; 95% CI = 74.3 to 88.7%) when asked if the touch free barrier would improve their stethoscope hygiene compliance if it were readily available over the other options of no impact, slightly or significantly worsen (36.1%; 95% CI = 27.5 to 45.4%). Finally, although the impression of stethoscope hygiene affecting patient satisfaction was similar (30.8% and 32.5% for “no effect” and “unsure,” respectively), the majority (36.7%) felt that stethoscope hygiene would improve patient satisfaction.
Discussion
The results of our surveys revealed opportunities to improve stethoscope hygiene practices in hospitals, and a need to identify novel solutions to eliminate pathogen spread via stethoscopes. In the current study, the patient and the healthcare professional cohorts both reported that they felt a clean stethoscope was important, indicating that they may have recognized that it can harbor pathogens. Nevertheless, patients witnessed healthcare professionals cleaning their stethoscope only “sometimes” or “never,” and many patients were not sure if the stethoscope had been cleaned at all.
...the patient and the healthcare professional cohorts both reported that they felt a clean stethoscope was important...When asked how frequently they cleaned their stethoscopes for at least 60 seconds, healthcare professionals in our study were most likely to choose “between every patient” or “between every few patients.” This is of questionable accuracy, as no recent observational study has ever reported CDC compliant rates of stethoscope cleaning to exceed a rate of 10% of patient contacts (Boulée et al., 2019; Vasudevan et al., 2019). In fact, the failure of stethoscope cleaning despite a claim of compliance has been well documented in ambush studies. In ambush studies, stethoscope diaphragm cultures are obtained immediately after the user reports their frequency of cleaning. These have shown rates of positive cultures to exceed 90% (Alali et al., 2020). The only conclusions that can be drawn from the summary of this data are that either stethoscope cleaning does not work, or that self-reports of adequate stethoscope hygiene are extremely unreliable.
Ultimately in our study, patients rarely reported witnessing stethoscope hygiene, despite that the healthcare professionals stated they did so frequently. It is possible that patients simply did not notice them cleaning their stethoscopes. Due to the low rates of stethoscope hygiene reported in the literature, it is more likely many patients did not see the healthcare professionals clean their stethoscope because it was not done.
...it is possible that healthcare professionals are not disinfecting their stethoscopes as often as they think.Given the overwhelming evidence that stethoscope hygiene rates are quite low despite perceptions of its importance, it is possible that healthcare professionals are not disinfecting their stethoscopes as often as they think (Datta et al., 2018; Ghumman et al., 2013; Jenkins et al., 2015; Rao et al, 2017). In a 2019 observational study, researchers found that providers did not disinfect their stethoscopes at all in 82% of encounters, including cases of open chest and abdominal wounds (Boulée et al., 2019). This is concerning in that a contaminated stethoscope could easily infect the patient with non-intact skin (Boulée et al., 2019). In the current sample, over a third of the patient cohort had a chronic disease affecting their immune system or had an open wound or burn above the waist, demonstrating the vulnerability of many patients who have their skin touched with a contaminated stethoscope.
In a recent report, researchers showed that physician awareness of potential stethoscope contamination is higher since the onset of the COVID-19 pandemic compared to pre-pandemic, yet only a little over half actually performed optimal stethoscope hygiene (Vasudevan et al., 2022). Previous work reports that healthcare professionals were aware of the importance of stethoscope hygiene (100%), but 30% admit to never disinfecting their stethoscopes (Datta et al., 2018). This is in marked contrast to the current sample in which over 94% reported that they cleaned their stethoscope at least weekly, and only 5.8% reported never cleaning their stethoscope. In a recent systematic review, observations revealed infrequent disinfection, and a stethoscope diaphragm contamination rate of over 50% (Queiroz Júnior et al., 2021). Thus, the high rate of reported stethoscope disinfection in our sample of healthcare professionals is in contrast to prior research. Nevertheless, as we did not culture stethoscopes, we cannot provide data on pathogens they may have been harboring.
...previous reports have shown that patients’ perceptions of hospital cleanliness in general can have an impact on patient satisfaction.Results of the current study revealed that patients perceived both alcohol and touch free barrier as positive visual evidence of a clean stethoscope, and both methods increased their comfort when a stethoscope touched their skin. Given that the touch free barrier was likely unfamiliar to patients in our sample, these results offer the possibility that the touch free barrier is acceptable to most patients. We found no previous research on patients’ perceptions of visual evidence of a clean stethoscope or comfort when it touched their skin. However, previous reports have shown that patients’ perceptions of hospital cleanliness in general can have an impact on patient satisfaction (Jabbar et al., 2010); it is not known if stethoscope cleanliness might also be related to patient satisfaction. In addition, healthcare professionals in our study did not report a preference for one method of stethoscope hygiene over another for patient safety or satisfaction.
Regarding patient safety, our results showed that healthcare professionals felt cleaning with alcohol was superior to no cleaning at all; however, there was no difference when alcohol and touch free barrier were compared. Despite these perceptions, touch free barriers have been shown to protect against pathogens. Researchers demonstrated that c-diff colony counts were zero on stethoscope diaphragm barrier surfaces after touch free barriers had been applied to contaminated stethoscopes and incubated for 48 hours (Peacock et al., 2021), thus providing an aseptic surface for patient contact. It is also important to note that c-diff is increasingly resistant to 70% isopropyl alcohol (Jabbar et al., 2010).
[Both] cohorts reported that the touch free barrier would likely be easier compared to cleaning with alcohol.Both the patient and healthcare professional cohorts reported that the touch free barrier would likely be easier compared to cleaning with alcohol. Patients felt the touch free barrier would be easier for providers to use, and healthcare professionals reported it would be easier for their workflow. In light of these findings, the impact of stethoscope hygiene on daily workflow should be considered. It has been reported (Ghumman et al., 2013) that 76% of providers used their stethoscope frequently throughout the day and implied that cleaning a stethoscope for the recommended 60 seconds with every use is simply not feasible in busy clinics (Jain et al., 2013). In light of prior research that showed touch free barriers provided protection against pathogens (Peacock et al., 2021), it is possible that a touch free barrier is the optimal solution to reduction of HAI as it would have the potential to also improve workflow.
Hygiene of all kinds, though vital for patient safety, takes time, and can impact workflow. A 2017 observational study found that nurses spent approximately 8-10 minutes per shift washing their hands, resulting in 58-70 minutes of total time for the intensive care units if the nurses complied fully with hand hygiene protocol (Stahmeyer et al., 2017). Similarly, stethoscope hygiene would take another hour per day per nurse/provider if they saw 30 patients and disinfected with alcohol for 60 seconds before and after each one (Kalra et al., 2021a). It is not known if improvements in workflow would improve compliance; nevertheless, the healthcare professionals in our sample answered positively regarding the likelihood that a touch free barrier would improve stethoscope hygiene compliance.
Regardless of the effectiveness of the hygiene method, it will only protect patients if it is performed regularly.Compliance is an important component of patient safety that must be considered. Regardless of the effectiveness of the hygiene method, it will only protect patients if it is performed regularly. As a result, if compliance is poor, patients could be at higher risk of HAI. As stated previously, the healthcare professionals in our sample reported that the touch free barrier would likely improve their stethoscope hygiene compliance. This may be in part due to their reported perception that it would be easier to use and improve workflow. Since they also believed that alcohol would improve patient safety over touch free barriers, they may need additional education on the effectiveness of the barriers. Research showed that nurses were less likely to report receiving training on any kind of stethoscope hygiene as compared to physicians (Ghumman et al., 2018). All healthcare professionals would benefit from using the barriers in practice so they can experience first-hand their potential to reduce or eliminate stethoscope-mediated pathogen transmission while maintaining high quality sound transmission (Kalra et al., 2021b).
Future research is needed to explore exposing healthcare professionals to touch-free barriers in their daily patient care, including easy access to barriers on nursing units and in every patient room. Research is also needed to address gaps in the literature regarding patient perceptions of stethoscope cleanliness. It is possible that the more that patients see touch free barriers used in practice, the more they will see it as a viable stethoscope hygiene option. Finally, researchers should conduct larger scale studies to compare bacterial contamination rates between touch free barriers and other methods of stethoscope hygiene.
Limitations
This study had several limitations. First, it was a cross-sectional design using survey methodology. Therefore, it is possible there was response bias wherefore those who participated felt strongly one way or the other. The study used self-report based on video scenarios. In prior research on stethoscope hygiene, self-reported rates were not consistent with stethoscope hygiene compliance (Alali et al., 2020; Boulée et al., 2019; Vasudevan et al., 2022). The sample size, while adequately powered, was still small and limited to a single hospital. Larger studies in more diverse populations may provide different results. In addition, causation cannot be inferred from the results of this nonexperimental study.
Conclusions
Overall, practitioners felt that a touch free barrier would improve workflow and stethoscope hygiene compliance...This research provides important information regarding patients’ and healthcare professionals’ perceptions of a novel aseptic touch free stethoscope barrier compared to the use of alcohol swabs for stethoscope hygiene. Respondents reported that they valued stethoscope hygiene, although patients rarely (only 5%) witnessed actual stethoscope hygiene. More than one third of respondents felt stethoscope hygiene would improve patient satisfaction. Overall, practitioners felt that a touch free barrier would improve workflow and stethoscope hygiene compliance, a feature that may support hospital consideration of implementing aseptic touch free stethoscope barriers as part of a strategy to reduce nosocomial infection rates.
Conflict of Interest Statement: One of the co-investigators holds stock in Aseptiscope Inc. The costs of this study were funded by Aseptiscope, Inc. None of the other authors have a conflict of interest with Aseptiscope or other corporate entities.
Funding source: The costs of this study were funded by Aseptiscope, Inc.
Commercial affiliations: One of the authors is Chief Medical Officer, Aseptiscope, Inc.
Authors
Lee Anne Siegmund, PhD, RN, ACSM-CEP, FAAN
Email: siegmul@ccf.org
ORCID ID: https://orcid.org/0000-0002-9606-306X
Lee Anne Siegmund is a Senior Nurse Scientist in Cleveland Clinic Office of Nursing Research and Innovation. As a research mentor, Dr. Siegmund has guided many nurses through their own research and she also conducts her own research on frailty, exercise to improve outcomes among older adults, and healthcare quality. Dr. Siegmund, whose work has been cited in 25 countries, recently published her middle range theory on frailty care and is currently testing the model.
Frank Peacock IV, MD, FACEP, FACC, FESC
Email: frankpeacock@gmail.com
ORCID ID: https://orcid.org/0000-0002-2730-6742
Frank Peacock is a Professor of Emergency Medicine and Vice Chair of Research in Emergency Medicine at Baylor College of Medicine, in Houston, Texas. With >800 peer reviewed publications, he is also the co-editor of several textbooks including Cardiac Emergencies, Short Stay Management of Heart Failure, and Short Stay Management of Chest Pain. Dr. Peacock is 3-time winner of the Best Research Paper Award from the American College of Emergency Physicians and the Ray Bahr Award from the American College of Cardiology.
James Bena, MS
Email: benaj@ccf.org
ORCID ID: https://orcid.org/0000-0002-7592-0480
James Bena is a biostatistician at the Cleveland Clinic. He has a broad background in statistics and public health research experience from his work at the National Institute for Occupational Safety and Health. He works with researchers from many basic and clinical science specialties on both observational and experimental studies and employs diverse statistical approaches to address research questions posed by collaborating investigators.
Shannon Morrison, MS
Email: morriss2@ccf.org
ORCID ID: https://orcid.org/0000-0002-9507-1762
Shannon Morrison is a statistical programmer at the Cleveland Clinic. Her specialties include data management and use of the SAS programming language. She has been with the Cleveland Clinic for 16 years.
References
Alali, S. A., Shrestha, E., Kansakar, A. R., Parekh, A., Dadkhah, S., & Peacock, W. F. (2020). Community hospital stethoscope cleaning practices and contamination rates. American Journal of Infection Control, 48(11), 1365-1369. https://doi.org/10.1016/j.ajic.2020.04.019
Bansal A., Bhan, B. D., Gupta, K., & Purwar, S. (2019). To assess the stethoscope cleaning practices, microbial load and efficacy of cleaning stethoscopes with alcohol-based disinfectant in a tertiary care hospital. Journal of Infection Prevention, 20(1), 46-50. https://doi.org/10.1177/1757177418802353
Boulée, D., Kalra, S., Haddock, A., Johnson, T. D., & Peacock, W. F. (2019). Contemporary stethoscope cleaning practices: What we haven't learned in 150 years. American Journal of Infection Control, 47(3), 238-242. https://doi.org/10.1016/j.ajic.2018.08.005
Centers for Disease Control and Prevention. (2021). Healthcare Associated Infections (HAI). https://www.cdc.gov/healthcare-associated-infections/index.html
Centers for Medicare & Medicaid Services. (2017). CMS Survey and Certification Group 2016/2017 Nursing Home Action Plan Action Plan for Further Improvement of Nursing Home Quality. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/Downloads/2016-2017-Nursing-Home-Action-Plan.pdf
Datta, P., Kaur, M., Rawat, S., Gupta, V., & Chander, J. (2018). Stethoscope, "the friendly foe" - A study to evaluate bacterial contamination of stethoscopes and disinfection practices. Journal of Infection in Developing Countries, 12(10), 887-893. https://doi.org/10.3855/jidc.10128
Disk Cover System. (n.d.). Home: Protect your patient.https://diskcover.com/
Gaisser, D. J., Lowey, S. E., & Barbel, P. (2021). An examination and comparison of stethoscope hygiene in nursing education programs. Journal of Nursing Education, 60(5), 277-280. https://doi.org/10.3928/01484834-20210420-07
Ghumman, G. W., Ahmad, N., Pop-Vicas, A. & Iftikhar, S. (2018). Stethoscope cleaning during patient care. Rhode Island Medical Journal, 101(4), 18-20.
Guerra-Martín, M. D., & González-Fernández, P. (2021). Satisfaction of patients and family caregivers in adult intensive care units: Literature review. Enferm Intensiva (English Ed), 32(4), 207-219. https://doi.org/10.1016/j.enfie.2020.07.002
Holleck, J. L., Campbell, S., Alrawili, H., Frank, C., Merchant, M., Rodwin B., Perez, M., Gupta, S., Federman, D., Chang, J., Vientos, W., & Dembry, L. (2020). Stethoscope hygiene: Using cultures and real-time feedback with bioluminescence-based adenosine triphosphate technology to change behavior. American Journal of Infection Control, 48(4), 380-385. https://doi.org/10.1016/j.ajic.2019.10.005
Jabbar, U., Leischner, J., Kasper, D., Gerber, R., Sambol, S., Parada, J., Johnson, S., & Gerding, D. (2010). Effectiveness of alcohol-based hand rubs for removal of clostridium difficile spores from hands. Infection Control and Hospital Epidemiology, 31(6), 565-570. https://doi.org/10.1086/652772
Jain, A., Shah, H., Jain, A., & Sharma, M. (2013). Disinfection of stethoscopes: Gap between knowledge and practice in an Indian tertiary care hospital. Annals of Tropical Medicine and Public Health, 6, 236-9. https://doi.org/10.4103/1755-6783.116503
Jenkins, I. H., Monash, B., Wu, J., & Alpesh, A. (2015). The third hand: Low rates of stethoscope hygiene on general medical services. Journal of Hospital Medicine, 10(7), 457-458. https://doi.org/10.1002/jhm.2359
Kalra, S., Amin, A., Albert, N., Cadwell, C., Edmonson, C., Gaynes, R., Hand, M., Marinella, M., Morley, C., Sieck, S., & Vasudevan, R. (2021a). Stethoscope hygiene: A call to action. Recommendations to update the CDC guidelines. Infection Control and Hospital Epidemiology, 42(6), 740-742. https://doi.org/10.1017/ice.2021.115
Kalra, S., Garri, R. F., & Shewale, J. B. (2021b). Aseptic disposable stethoscope barrier: Acoustically invisible and superior to disposable stethoscopes. Mayo Clinic Procedures, 96(1), 263-264. https://doi.org/10.1016/j.mayocp.2020.10.029
Longtin, Y., Schneider, A., Tschopp, C., Renzi, G., Gayet-Ageron, A., Schrenzel, J., & Pittet, D. (2014). Contamination of stethoscopes and physicians' hands after a physical examination. Mayo Clinic Proceedings, 89(3), 291-299. https://doi.org/10.1016/j.mayocp.2013.11.016
O'Flaherty, N., & Fenelon, L. (2015). The stethoscope and healthcare-associated infection: A snake in the grass or innocent bystander? Journal of Hospital Infection, 91(1), 1-7. https://doi.org/10.1016/j.jhin.2015.04.010
Peacock, W. F., Kalra, S., Vasudevan, R. S., & Torriani, F. (2021). Aseptic stethoscope barriers prevent c difficile transmission in vitro. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 5(1), 103-108. https://doi.org/10.1016/j.mayocpiqo.2020.10.002
Queiroz Júnior, J. R. A., Melo, I. O., Calado, G. H. D. S., Cavalcanti, L. R. C., Cavalcanti, L. R. C., & Sobrinho, C. R. W. (2021). Identification and resistance profile of bacteria isolated on stethoscopes by health care professionals: Systematic review. American Journal of Infection Control, 49(2), 229-237. https://doi.org/10.1016/j.ajic.2020.07.007
Rao, D. A., Aman, A., Muhammad Mubeen, S., & Shah, A. (2017). Bacterial contamination and stethoscope disinfection practices: A cross-sectional survey of healthcare workers in Karachi, Pakistan. Tropical Doctor, 47(3), 226-230. https://doi.org/10.1177/0049475516686543
Stahmeyer, J. T., Lutze, B., von Lengerke, T., Chaberny, I. F., & Krauth, C. (2017). Hand hygiene in intensive care units: A matter of time? Journal of Hospital Infection, 95(4), 338-343. https://doi.org/10.1016/j.jhin.2017.01.011
Tyagi, U., & Barwal, K. C. (2020). Ignac Semmelweis-Father of Hand Hygiene. Indian Journal of Surgery, 82(3), 276-277. https://doi.org/10.1007/s12262-020-02386-6
Vasudevan, R. S., Mojaver, S., Chang, K. W., Maisel, A. S., Peacock, W. F., & Chowdhury, P. (2019). Observation of stethoscope sanitation practices in an emergency department setting. American Journal of Infection Control, 47(3), 234-237. https://doi.org/10.1016/j.ajic.2018.08.028
Vasudevan, R. S, Nedjat-Haiem, M. A., Mahadevan, A., Herbert, M. S., Lander, L., Warsi, T., Shaikh, U., Harding, C., & Savoia, M. C. (2022). Assessing changes in stethoscope hygiene during COVID-19: A multi-centre cross-sectional study. Journal of Hospital Infection 127, 1-6. https://doi.org/10.1016/j.jhin.2022.05.019


