Healthcare organizations are embracing the sciences of safety, improvement, human factors, and complexity to transform their culture into a culture of safety and high reliability. Nurses are the front lines of healthcare delivery, and as such, the front lines of safety and quality processes and outcomes. Nurses are required to both understand and develop the skills needed to improve care processes and to own the work of improvement as a professional responsibility. These changes demand that nurses understand both the complex demands of providing harm-free care and the system dynamics needed to create the conditions for improved outcomes, organizational, and system performance, and intraprofessional development and teamwork. The author presents the challenge of maintaining a safe patient care environment and describes a model that can detect and mitigate the migration of safe nursing care into at-risk and unsafe nursing care. She emphasizes the importance of healthcare organizations performing as high reliability organizations and outlines ‘planned practices’ steps to introduce new technology and innovation, and concludes by considering the interaction between individual practice and system performance.
Key words: High reliability organizations (HROs), borderline tolerable conditions for use (BTCU), dynamic system model, health care safety, failure mode and effects analysis (FMEA), human factors, safety science, improvement science
Exceptional leadership in nursing is more essential than ever before. Exceptional leadership in nursing is more essential than ever before. The increasing emphasis on safety and quality in care delivery demands new knowledge and skills. Today's healthcare professionals acquire and practice the skills to improve care processes, and own the work of improvement as a professional responsibility. Basic health sciences curricula now include content in the sciences of safety, improvement, human factors, and complexity. The foundation of a transparent healthcare setting, defined by Leape et al. (2009) as an environment in which defects are made visible and learnings are shared freely and without inhibition, is being recognized and embraced for the purpose of advancing safety and improvement. Organizations are creating environments characterized by psychologically safe spaces in which open communication is expected and rewarded, and errors can be examined without fear (Morath & Leary, 2004). Nursing professionals on the front lines of care and in healthcare management positions need to expand their portfolio of skills in order to provide the clinical leadership needed to achieve a culture of safety. It is important to see each nurse as a caregiver and healer, and also a system improver, prepared to improve the systems of care rather than to become a victim of a faulty and error-prone system.
The Challenge
The work of Zimmerman, a professor and researcher in organizational science and complexity, provides a helpful context for the following discussion addressing safe patient care. Glouberman and Zimmerman (2004) have identified the nature of three categories of problems: simple, complicated, and complex. The following Table summarizes the characteristics of these categories of problems.
Table. Distinctions Between Categories of Problems
|
|
Categories of Problems |
||
|
|
Simple |
Complicated |
Complex |
|
Characteristics
|
Known elements
|
Elements are knowable
|
Elements may be partially known and may change
|
|
|
Predictable outcomes
|
Largely predictable
|
Unpredictable
|
|
|
Checklists and protocols
|
Algorithms
|
Relationships/correlations
|
|
|
Low autonomy
|
Low autonomy
|
High autonomy
|
|
Aim
|
Reliability
|
Reliability
|
Resilience
|
Adapted with permission from Glouberman, S. & Zimmerman, B. (2004). Complicated and complex systems: What would successful reform look like? In Forest, P., Marchildon, G., & McIntosh, T. (Eds.), Romanow Papers: Changing health care in Canada, Vol. 2 (p.22). Toronto, Ontario. Copyright (Table) 2004 by Brenda Zimmerman.
Each diagnosis, individual patient, care delivery model, and social context has simple, complicated, and complex problems. Healthcare delivery is often approached as if the problems encountered are all simple or complicated problems, and many of them are. However, this is not the case in dealing with patient safety and the transformations required to make healthcare safer. Sir Cyril Chantler, Chairman of the Great Ormond Street Hospital for Children National Health Service Trust (GOSH), captured the dilemma of contemporary healthcare when he stated: “Health care used to be simple, ineffective, and relatively safe. Now it is complex, effective, and potentially dangerous,” (Chantler, 1999, p.1181). Individual knowledge and skill is essential, yet insufficient to deliver care safely and reliably. We are moving from individual competency and performance to team skills, system reliability, and resilience.
In today’s healthcare environment, it is essential to understand our context of complexity, with its attendant uncertainties, ambiguities, emergent properties, and need for continual learning, sensemaking, and resilience. This environment requires the essential and combined efforts of everyone involved in delivering care, and everyone involved in managing the conditions in which the care is delivered, to make the changes that will result in (a) improved outcomes, (b) improved organizational and system performance, and (c) improved intraprofessional learning and team work.
A Model for Nursing Intervention
A model that has great utility in understanding safety in complex, dynamic systems is the Dynamic Systems Model. This model describes the boundaries of financial performance (production), workforce satisfaction, and patient safety (Cook & Rasmussen, 2005). Of particular note is the safety boundary, to be described later in the text. Failure to recognize migration (or drift) of practice from the safety boundary into areas of risk results in greater vulnerability and the increased probability of medical accidents and harm being introduced into the care delivery system. Nurses, who are present at the ‘defining moments’ of such system migration, are in key positions to recognize and respond to restore safe practice. Transparency and knowledge of boundaries for safe practice are required for nurses to identify and intervene when care is moving into the unsafe practice boundary.
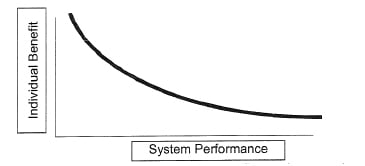
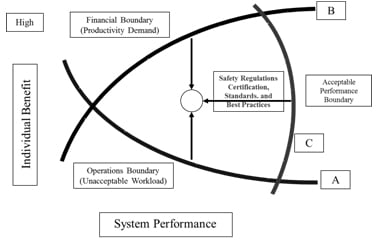
The Dynamic Systems Model includes two axes: one of individual benefit (personal benefit) and one of system performance (organizational benefit), as illustrated in Figure 1. Amalberti (2001), a scientist and physician who has studied safety systems extensively, has identified that as individual benefit accrues, system performance often denigrates. This process is noted in the following discussion and figures accompanying this discussion.
|
Figure 1. Dynamic Systems Model
Figure 1. Interaction between individual benefit and system performance. As individual benefit increases, system performance decreases, and vice versa. Adapted with permission from “Going Solid,” by R. Cook and J. Rasmussen, 2005, Quality & Safety in Health Care, 14, p. 131. Copyright 2004 by R.I. Cook. |
For example, a nurse caring for four or five patients, each of whom requires administration of medications twice during the shift, may accrue individual benefit by accessing the medication dispensing device to withdraw each patient’s medications for both the first and second medication administration at one time. By placing the medications in a storage area, such as a uniform pocket, until needed the nurse can efficiently administer the specified medications to each patient without returning to the stationary device a second time during the shift.
In doing so, the nurse reduces process steps, increases individual productivity, and increases the probability of having time for a break and completing the shift at the scheduled time. In doing so, the nurse reduces process steps, increases individual productivity, and increases the probability of having time for a break and completing the shift at the scheduled time. Soon other colleagues begin to accept this practice. However, because it is in violation of medication administration policy, the practice is not transparently discussed among the nurses. Because medication errors and adverse events are rare at this patient care site, there is a belief on the part of the nurses that defends them against seeing this violation of procedure as being at risk for error (Haraden, 2008). This style of medication administration will continue in this manner, perhaps for a time with positive feedback for reducing overtime through greater productivity, until the laws of probability are realized and there is a serious event due to a mix-up in medication.
This work-around migrates (moves) the boundaries of practice into the area of risk-prone practice, or as expressed in safety-science terminology, into Borderline Tolerable Conditions of Use (BTCU), in which a system migrates toward unsafe practice as individuals gain the maximum benefit for the minimum perceived probability of harm (Amalberti, 2006). Eventually,as harm or near-miss events accrue, this migration is met by management with more strident policies, additional process steps, staff re-training, and greater complexity. These well-intended interventions in the name of safety may well result in little individual benefit and no improvement in system performance.
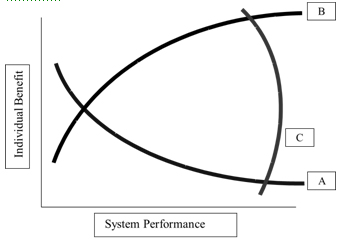
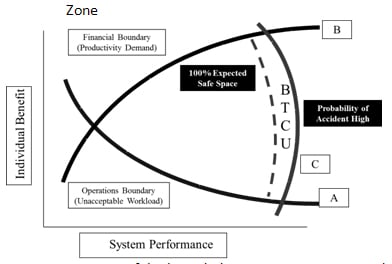
To further elaborate on the dynamics of individual benefit and system performance, consider that as an individual nurse and as an organization, we work within an envelope formed by three boundaries, namely (A) an operations workload boundary, (B) a financial boundary, and (C) a safety boundary as illustrated in Figure 2 and discussed below.
|
Figure 2. Dynamic Systems Model – Boundaries of Operation
Figure 2. Workload, financial, and safety boundaries of operating system. Operations workload, A, has financial implications, B, and both interact with the limits of safety, C. Adapted with permission from “Going Solid,” by R. Cook and J. Rasmussen, 2005, Quality & Safety in Health Care, 14, p. 131. Copyright 2004 by R.I. Cook. |
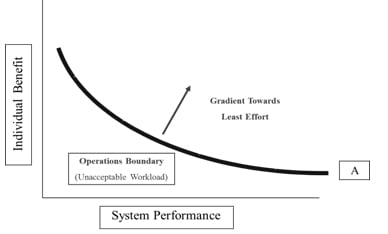
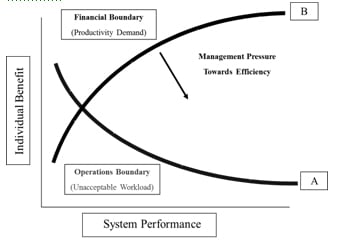
...well-intended interventions in the name of safety may well result in little individual benefit and no improvement in system performance. Each individual and organization has an operating point, an understanding of where practice resides within the organizational boundaries of care. This operating point needs to be understood to hold the boundaries in dynamic tension so as to produce optimal results. The acceptable workload/work life boundary is defined by staff experience and development indicators. The financial/productivity boundary is defined by budget and activity indicators. Although the safety boundary is less well defined, process measures, such as compliance to standards of care and standards of practice, regulatory and accreditation standards, and clinical outcomes, are beginning to define the safety boundary as metrics in these areas become more reliable. The boundaries of the model are illustrated in Figures 3, 4, and 5.
|
Figure 3. Dynamic Systems Model – Operations/Workload Boundary
Figure 3. Further definition of the workload boundary. Adapted with permission from “Going Solid,” by R. Cook and J. Rasmussen, 2005, Quality & Safety in Health Care, 14, p. 131. Copyright 2004 by R.I. Cook. |
|
Figure 4. Dynamic Systems Model - Financial Boundary
Figure 4. Interaction of the financial and workload boundaries. Adapted with permission from “Going Solid,” by R. Cook and J. Rasmussen, 2005, Quality & Safety in Health Care, 14, p. 131. Copyright 2004 by R.I. Cook. |
|
Figure 5. Dynamic Systems Model - Safety Boundary
Figure 5. Interaction of the operations, financial, and safety boundaries. Adapted with permission from “Going Solid,” by R. Cook and J. Rasmussen, 2005, Quality & Safety in Health Care, 14, p. 131. Copyright 2004 by R.I. Cook. |
When the pressures on the financial and production boundaries are great, as experienced by many providers in healthcare today, an equal pressure toward a gradient of least resistance is activated in the people system to restore equilibrium and individual benefit in practice. If this dynamic tension is not recognized and balanced, the pressure gradient pushes the safety boundary out into greater risk-prone practice or BTCU as illustrated in Figure 6.
|
Figure 6. Dynamic Systems Model - Pressure Gradients Pushing Practice into Unsafe Practice Zone
Figure 6. Margins of the bounded system enter BTCU. Adapted with permission from “Going Solid,” by R. Cook and J. Rasmussen, 2005, Quality & Safety in Health Care, 14, p. 131. Copyright 2004 by R.I. Cook. |
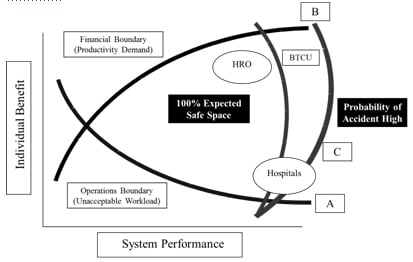
Continued, unmitigated pressure pushes the safety boundary out into a high hazard zone in which the probability of accidents is high. Hospitals routinely operate within the BTCU and migrate into unsafe practice as a course of normal operations. Normalization of deviance is commonplace and situational awareness is limited, because “we have always done it this way.” When individuals or teams migrate into unsafe practice, there are symptoms. These symptoms include breakdowns in communication and teamwork, shortcuts in practice, increased errors, clinical surprises, and failure to recognize subtle warning signs while problems escalate from minor to major problems. Note the following illustration of the operating points, or ability to balance the described boundaries, in high-reliability organizations (HRO) and hospitals. Figure 7 illustrates the operating points within the envelope of the three boundaries.
|
Figure 7. Boundaries of Exceedency - High Risk and Unsafe Practice
Figure 7. High-reliability organizations remain within system boundaries, while hospitals remain at the outer edge of safety. Adapted with permission from “Going Solid,” by R. Cook and J. Rasmussen, 2005, Quality & Safety in Health Care, 14, p. 131. Copyright 2004 by R.I. Cook. |
In this case, the re-evaluation and possible cancellation of elective cases with future attention to the barriers for timely discharges may create a ‘pull back’ for staff and restore equilibrium and practice within the safety boundary. Cook and Rasmussen (2005) illustrated this phenomenon through a surgical scheduling example: a full Operating Room schedule, a busy Emergency Department with emergency surgical add-on patients, a Post-Anesthesia Care Unit that cannot discharge patients in a timely manner and that is becoming overwhelmed with the escalating risk due to a lack of Intensive Care Unit (ICU) beds, lack of ICU beds attributable to the inability to transfer patients to a post-operative or step-down unit, and a bottleneck for post-ICU beds due to slow discharges from the post-operative care units. The production pressure needs relief so that practice within the envelope of safety can be re-established. In this case, the re-evaluation and possible cancellation of elective cases with future attention to the barriers for timely discharges may create a ‘pull back’ for staff and restore equilibrium and practice within the safety boundary.
High Reliability as the Aim for Healthcare
While there is study of the operating point and boundaries of exceedency in High Reliability Organizations (HROs), i.e., organizations in which failure is not an option because lives are at stake, there is less known about this phenomenon in healthcare delivery. HRO industries, such as the nuclear, aerospace, fire jumper, and Nimitz-style aircraft carrier industries, all have relevant lessons for the healthcare industry in that they continually analyze and maintain an acceptable operating point that does not exceed the boundaries of safety. They have developed a culture of safety.
First, a HRO knows its operating point within the operating envelope and manages that operating point to optimize individual benefit, system performance, and safety. There is awareness and sensemaking at every level of the organization, as safety is everyone’s first obligation. Roles and responsibilities are clearly articulated in the context of robust teamwork:
- The chain of command to escalate concerns is clear, understood, and respected.
- The staff are trained with verified competencies individually, and collectively as team members, through crew resource management, rehearsals, and simulations.
- The technical work is both understood from a detailed process flow perspective, one that is designed for reliability, and also constantly monitored and improved.
- Standardization and simplification are specifications for work.
- Human factors science experts study the relationship(s) between human beings and their technical work environment.
...safety is everyone’s first obligation.Refer back to the medication delivery example. How many nurses who would use the stationary medication dispensing device were involved in understanding and mapping the technical work processes associated with this device before it was installed? Was the technology purchased for inventory control and charge capture so as to optimize financial return for the organization? Or was it purchased to optimize workflow and safety? By examining technical work and workflow processes, the fit between care delivery requirements and technology can be better identified, the method more appropriately selected, and changes more safely implemented.
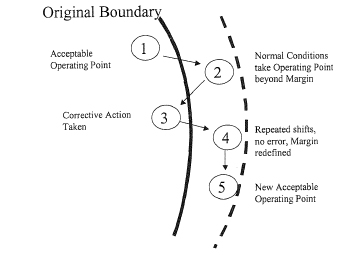
Planned Practices to ‘Push the Boundary’
New practices and technologies are developed by ‘flirting with the edges’ of BTCU. This appropriately occurs, not by drift or migration due to confounding conditions, but through carefully considered, designed, and studied implementation. As new vulnerabilities and risk emerge, professionals work to mitigate the risk of the changed situation. This is a process of simulation; testing; and use of methods, such as the Failure Mode and Effects Analysis (FMEA) (Mikulak, McDermott, & Beauregard, 1996). An example of flirting with the edges might occur when a new infusion pump, a new system of rounding, or new electronic tools are introduced. The important ability to recognize when an environment is in a zone of risk gives nurses the opportunity to ‘pull back’ and use, at least for a time, the ‘tried and true practices’ in which the risk is known and/or can be anticipated, even though these tried and true practices may offer less-optimal care. In this process, a new boundary of safety is established to accommodate new technologies and care design innovations, as illustrated in the five steps diagrammed below (Cook & Rasmussen, 2005). The broken line represents the new boundary.
Important things to remember about BTCU:
- It defines the safety and quality boundary.
- It provides a transparent system of production and recovery from any risk that may harm, or has the potential to harm, patients.
- It requires design, anticipation of danger, and ‘pull-back’ strategies.
- It requires teamwork and peer monitoring to safely move into a new and acceptable operating point.
- The innovation/adoption of new technologies requires that margins be tested and studied.
Conclusions: System Performance and Individual Practice
A culture of safety cannot be achieved without collaboration between front-line staff and mid-level managers. While this article has focused on system changes, the practice changes that individual nurses need to make are of equal importance. The discipline of human factors is most helpful in bringing this understanding to the individual-nurse level. Because humans consistently overestimate their abilities, underestimate risks, and are fallible, attention must be paid to the manner in which staff nurses are engaged and prepared to create new clinical standards that enhance a culture of safety within their work setting.
Nurses play an essential role in developing the culture of safety. Using what is known about organizational change, human factors, and safety science, nurse leaders can orchestrate a role-based, patient-centered, social-learning system to improve reliability in care delivery and help nurses provide leadership to strengthen the culture of safety. Staff educators and managers can help front-line practitioners understand and manage the desired operating point between the boundaries of acceptable and unacceptable financial performance, workload, and safe care delivery. Huy (2001) has described the importance and the power of middle management to lead transformational change. Mid-level managers who are entrepreneurial, productive, and flexible are the most effective allies in bringing about changes that will advance the culture of patient safety and habitual excellence on a given unit. A culture of safety cannot be achieved without collaboration between front-line staff and mid-level managers. The ability of both nurses and managers to have shared meaning and understanding of the operating point, within which the boundaries of production, workload, and safety are contained, is essential for establishing a culture of safety.
Author
Julianne Morath, MS, RN
E-mail: Julie.morath@vanderbilt.edu
Julianne Morath has served for three decades in executive leadership positions in healthcare and has held multiple faculty appointments. She is currently Chief Quality and Patient Safety Officer for Vanderbilt University Medical Center (Nashville, TN), Director of the Center for Clinical Improvement, and Associate Professor of Clinical Nursing. Ms. Morath was the inaugural recipient of the John Eisenberg Award for Individual Lifetime Achievement in Patient Safety, awarded through The Joint Commission and National Quality Forum. She currently serves on the Board of the National Patient Safety Foundation and the Virginia Mason Medical Center and Health System. Ms. Morath is a founding member of the Lucian Leape Institute, an elected member of the Board of Commissioners for The Joint Commission (TJC), and chairperson of the National Nursing Advisory Committee. She received her BSN degree from the University of Michigan (Ann Arbor, MI) and her MS degree from the University of California in San Francisco.
References
Amalberti, R. (April, 2001). Human error in medicine. Paper presented at the Salzburg International Seminar on Patient Safety and Medical Accident, Salzburg, Austria.
Amalberti, R., Vincent, C., Auroy, Y., & de Saint Maurice, G. (2006). Violations and migrations in health care: a framework for understanding and management. Quality & Safety in Health Care, 15, i66-i71. doi:10.1136/qshc.2005.015982.
Chantler, C. (1999). The role and education of doctors in the delivery of healthcare. Lancet, 353(9159), 1178-1181.
Cook, R., & Rasmussen, J. (2005). “Going solid”: A model of system dynamics and consequences for patient safety. Quality & Safety in Health Care, 14, 130-134. doi:10.1136/qshc.2003.009530.
Haraden, C., (April, 2008). Executing improvements in large-scale systems. Paper presented at the International Forum on Quality and Safety in Health Care, Paris, France.
Huy, Q. (2001). In praise of middle managers. Harvard Business Review, 79(8), 72, 79.
Leape, L., Berwick, D., Clancy, C., Conway, J., Gluck, P., Guest, J., Lawrence, D., Morath, J.,…Isaac, T. (2009). Transforming healthcare: a safety imperative. Quality & Safety in Health Care, 18, 424-428. doi:10.1136/qshc.2009.036954.
McCandless, K., & Zimmerman, B. (2002, April). Simplicity on the other side of complexity. Patient Safety Fellowship, Health Forum, American Hospital Association, Chicago, IL.
McDermott, R.E., Mikulak R.J., & Beauregard M.R. (1996). The basics of FMEA. Portland, OR: Resources Engineering, Inc.
Morath, J., & Leary, M. (2004). Creating safe spaces in organizations to talk about safety. Nursing Economics, 22(2), 344-352.