As the scientific evidence for human-caused climate change grows and awareness of the related health impacts increases, there is a need for nursing leadership in addressing climate change as a priority public health concern. The nursing role related to climate and health encompasses the nursing domains of research, education, practice, and policy/advocacy. Further, the Nursing Collaborative on Climate Change and Health - a partnership that includes the Alliance of Nurses for Healthy Environments, Climate for Health, and national nursing organizations - provides visible nursing leadership on climate change as a health imperative and creates momentum for solutions that nurses can engage in personally, in their communities and within the health sector.
Key Words: climate change, nursing, climate and health, global warming, nursing leadership, environmental health, sustainability, climate-smart healthcare, mitigation, adaptation, policy
The 1995 Institute of Medicine Report (IOM) Nursing, Health, and the Environment recommended that environmental health be integrated into the following four domains of the nursing profession: research, education, practice, and policy/advocacy (IOM et al., 1995). These four domains provide the framework for the work of the Alliance of Nurses for Healthy Environments (ANHE), which is an international nursing organization that focuses on the integration of environmental health into the nursing profession. These same four domains provide a useful framework for the integration of nurses’ knowledge of and responses to climate change. Nurses already have made great strides on this critical environmental health issue, but the threat and adverse outcomes related to climate change persist and are worsening. This article describes nurses’ responses in each of these domains. In addition, nursing’s professional and ethical obligations to do no harm will be examined through a climate change lens invoking the American Nurses Association’s (2015) Nursing Scope and Standards of Practice. Finally, recommendations for expanding nurses’ roles regarding climate health are offered.
Climate and Health Background
Since the mid-20th century increases in levels of greenhouse gas concentrations are causing more heat to be trapped in the atmosphere and are leading to a rise in global temperature (National Aeronautics and Space Administration [NASA], 2018). Current levels of carbon dioxide - a critical greenhouse gas - have reached the highest levels on record, and global temperature has risen 0.8 degrees Celsius (1.4 degrees Fahrenheit) since 1880 (NASA, 2018). Human activities are contributing to this unprecedented rise in atmospheric greenhouse gases and are indicated as the dominant cause of global warming since 1950 (Pachauri et al., 2014). The culpable human activities include, but not limited to, are transportation, housing, manufacturing, agriculture, and fossil fuel energy sources (oil/gas extraction, production, and use/combustion).
Changes in climate patterns contribute directly and indirectly to human health risks.
Changes in climate patterns contribute directly and indirectly to human health risks. Climate-related health risks are associated with temperature extremes and extreme weather, exposure to poor air quality from ground-level ozone pollution and wildfires, changes in the quality and availability of food and water, increases in vector-borne disease transmission, and mental health impacts and stress-related illness (Intergovernmental Panel on Climate Change [IPCC], 2018; U.S. Global Change Research Program [USGCRP], 2018; Watts et al., 2018). The Lancet Countdown, which is an interdisciplinary collaboration of academic institutions, intergovernmental agencies, and the United Nations, stated in its 2018 report on health and climate change that “the nature and scale of the response to climate change will be the determining factor in shaping the health of nations for centuries to come” (Watts et al., 2018, p. 1). The United States Fourth National Climate Assessment - a report mandated by the US Congress - notes that: a) communities are already experiencing effects related to climate change, and b) highlights both the need for substantive mitigative action to reduce greenhouse gas emissions and for adaptive action to prepare for unavoidable climate-related impacts (USGCRP, 2018).
Nursing Response to Climate Change: Research, Education, Advocacy, and Practice Framework
As the scientific evidence for a warming Earth grows, the risks to human and ecological health from environmental changes are becoming a more central part of the nation’s conversation and there is a more urgent need for action. The categorization of climate change as a critical public health concern rather than solely as an environmental issue has gained momentum over the past decade. As nurses have a significant understanding of the science behind health conditions and necessary treatments or interventions, their awareness of the science of climate change can further their recognition of climate change as a health issue and motivate action across the four domains of nursing: research, education, practice, and policy/advocacy.
The categorization of climate change as a critical public health concern rather than solely as an environmental issue has gained momentum over the past decade.
Research
The International Council of Nurses (ICN) (2018) issued an updated position statement Nurses, Climate Change, and Health that calls on nurses to participate in climate and health research as an avenue for leadership in addressing this health challenge. Adlong and Dietsch (2015) identified potential research topics on the health effects of climate change such as interventions designed to protect against climate-related extreme weather impacts, hospital-based practices to reduce greenhouse gas emissions, evaluation of needed infrastructure to enhance community resilience, and the implementation and evaluation of climate change educational programs for health professionals.
Research that analyzes nurses’ beliefs, knowledge, and awareness regarding climate and health can assist in identifying gaps in their understanding and engagement. A lack of awareness of concepts relating to environmental health, sustainability, and climate change can be a barrier to understanding the role of nurses in sustainable healthcare. Griggs, Fernandez, and Callanan (2017) identified barriers to sustainable health care that include the low priority given to environmental issues in high-pressured care settings, confusion about what the term sustainability means, and a disconnect between how local actions affect global issues. The Climate, Health, and Nursing Tool (CHANT) is a brief voluntary survey that was developed to further understand nurses’ awareness, behaviors, and engagement on climate change (Cook, Demorest, & Schenk, 2019). Results of the CHANT survey can provide valuable information to identify both progress and barriers in nursing engagement around climate change and to inform nurse-specific interventions to increase engagement. Nurses can take the CHANT survey at https://envirn.org/nurses-climate-survey/, and they are encouraged to take the survey annually so that results can be analyzed over time.
Nurses are skilled in translating complex research findings into easily digestible information by patients and the public and can similarly assist in the translation of climate science. Strategies for effective climate science communication include use of repeated messages to target audiences to strengthen public concern and support strategies to address climate change (Brulle et al., 2012) and “simple clean messages, repeated often, by a variety of trusted voices” (Maibach et al., 2014, p. 297). By framing issues in a specific manner and adopting effective strategies from past successful public health campaigns, nurses can increase public understanding, engagement, and support for climate action and solutions.
Finally, nurse researchers have an opportunity to evaluate the effectiveness of climate mitigation and response actions. For example, assessing the most effective way to engage hospital employees in commuting via public transportation or to promote plant-based dietary choices and address food waste in the institutions in which nurses serve, can help provide the evidence for best practices beyond more traditional clinical best practices.
Education
Although there has been a notable and well documented lack of environmental health content integrated into nursing education (Giddens & Brady, 2007; Richardson et al., 2014; Sweeney & Peyster, 2005; Whitehead, 2007), nursing faculty still are being called upon to further integrate healthcare sustainability and climate change into nursing education and training (Lilienfeld et al., 2018). Fortunately, there are a growing number of climate change-related educational tools created by and for nurses that are available to assist nursing faculty and other nurses who may have never learned about climate change in their education and training. For instance, the Nurses Climate Challenge (Challenge) (www.nurseclimatechallenge.org), a web-based educational program launched by Health Care Without Harm (HCWH) and the Alliance of Nurses for Healthy Environments (ANHE), features an array of resources to assist nurses who want to educate their colleagues about climate and health, either in formal academic settings or in other venues, such as the workplace or nursing conferences/workshops. The Challenge resources include slide decks of information on climate change and health, information and promotional materials to organize an educational session, and suggested action steps to address climate change in practice settings and at home. Those who use the materials and train health professionals are asked to log the numbers of nurses and other health professionals educated onto the site, which keeps a running total of all those who have been trained to date. When launched in May 2018, the Challenge set a goal of educating 5,000 health professionals on climate and health. Since the initial launch, nurses signed up for the Challenge have educated over 10,000 health professionals, prompting the launch a new goal in May 2019 - to educate 50,000 health professionals on climate and health by 2022.
In addition to the Challenge, ANHE regularly hosts webinars on various aspects of nursing and climate change, including webinars focused on effectively communicating about climate and health and how to advocate for the advancement of climate solutions across practice settings. These webinars are archived on the ANHE website: www.enviRN.org. ANHE (2018a) has developed a Climate and Health Toolkit tailored for nurses as well, which provides an online repository of information and resources to learn more about climate change and health.
The integration of the complex issues associated with climate change - defining what it is, how to reduce the contributors (greenhouse gases), how to respond to the emerging health effects, and how to prepare for extreme weather events and fires - into all levels of nursing education is critical to adequately prepare nursing students and practicing nurses to care for those affected by climate-related impacts. Environmental Health in Nursing - an open access electronic textbook created by ANHE member nurses (2016) - includes a chapter on climate change and can be utilized by faculty for their nursing curricula. Further, many new community and public health textbooks now include climate change content. Nursing faculty can also refer to the Global Consortium on Climate and Health Education (GCCHE) (2019) hosted by the Columbia University Mailman School of Public Health. The GCCHE aims to advance health professional education on climate and health impacts and provides faculty with course materials and resources for incorporating climate and health content into curricula. At present, 186 health professional schools globally are members of the GCCHE, including 25 schools of nursing.
Practice
In the practice domain, nurses are operating at two levels to address climate change. They are recognizing and acting on their knowledge of climate change’s health effects through their patient care and community health practices and are helping to make their hospitals and other health care settings into more climate ready and resilient institutions (climate-smart health care).
...nurses are operating at two levels to address climate change...through their patient care and community health practices and... climate-smart health care.
People who are likely to do outdoor work are at higher risk of heat exhaustion and heat-related deaths (Riley et al., 2018). To address these health risks, nurses working in federally qualified health centers in the Central Valley of California have been providing patient and community education regarding the early warning symptoms and early interventions for hyperthermia. In the Central Valley - where the temperature can exceed 110 degrees Fahrenheit and there are significant agricultural and oil / gas sectors that involve outdoor work - higher rates of acute and chronic kidney disease in farmworkers are being observed and are thought to be associated with chronic dehydration (Glaser et al., 2016). Farmworkers that are paid by the bushel or pound are at particular risk because they are often hesitant to stop working despite high temperatures. Nurse-led educational programs have focused on the need for linguistically appropriate messaging regarding both the importance of hydration and the awareness of early signs and symptoms of dehydration. Other nurses are working on Valley Fever - a chronic disease with recurrent acute episodes that is caused by soil-based fungal coccidioides organisms whose incidence is increasing due to climate change. There was a 46% increase from 2016 – 2017 in Kern County, which is a highly agricultural area of the Central Valley (California Department of Public Health [CDPH], 2018). See Figure 1 for areas in which coccidioidomycosis is endemic. Other vector borne diseases such as dengue fever and malaria also are increasing and moving into geographic areas where they have seldom appeared before (Watts et al., 2018). Therefore, nurses’ clinical assessment skills must be responsive to changes in climate related disease incidence (Chamberlain, 2008).
Figure 1. Areas Endemic for Coccidioidomycosis.
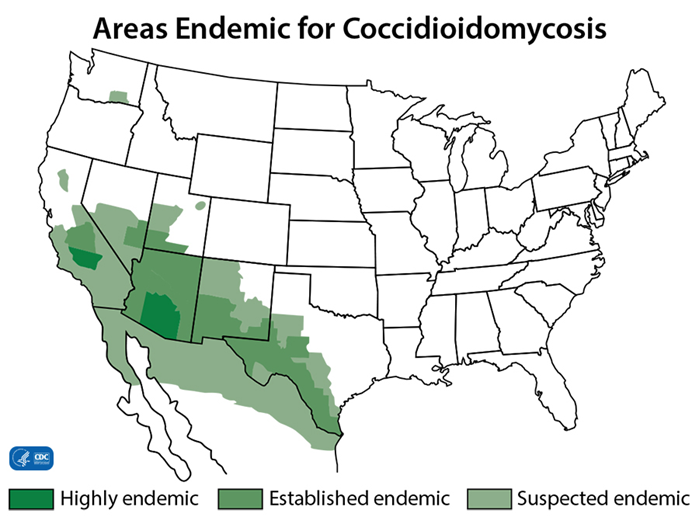
Reprinted from the Centers for Disease Control and Prevention (2019).
From a mitigation and sustainability perspective, nurses in the practice setting are taking leadership on a wide range of responses to climate change. They are engaged in energy conservation, incentivizing active transportation and use of public transportation, and helping to bring more plant-based food options to their hospitals’ cafeterias. Nurses and others in health care are also looking at the purchasing decisions made by hospitals and health care institutions.
At CleanMed 2019, the premier conference for health care sustainability leaders, nurse Jessica Dolan, BSN, RN received a national award for her efforts to better manage her hospital’s waste, helping to reduce impacts on the environment and saving her hospital unnecessary costs (HCWH, 2019). Nurses Julie Kleber, BSN, RN, BMTCN and Katie Cortes, BSN, RN, OCN working on the bone marrow transplant unit at Memorial Sloan Kettering Cancer Center work on have supported their institution’s sustainability efforts through the implementation of an unit-based energy efficiency initiative to turn off non-patient care computers in the evening, from 10 p.m. to 6 a.m., when no one uses them. They also have been successful in reducing wasted medical supplies on their unit and most recently challenged their fellow nurses to bring cutlery from home for their meal breaks rather than using disposable plastic cutlery. All of these small changes add up to shifts in our energy use and reduce our reliance on fossil-fuel derived plastics.
More nurses are assuming hospital leadership positions in their climate change efforts, such as Beth Schenk, PhD, MHI, RN-BC, a nurse scientist who co-directs sustainability for her health system’s 13 hospitals. Dr. Schenk has worked on initiatives across the health system to assess energy use in clinical areas and promote nurses’ awareness of energy conservation and efficiency and to promote waste reduction and optimization by recycling and composting as much as possible to minimize incinerated waste. Through public and staff (clinical and non-clinical) educational engagement, Dr. Schenk helps to prepare her health system and surrounding communities for the impacts of climate change through education on topics such as preparing for high heat and wildfire smoke days, as well as monitoring indoor air quality on high smoke days.
Health Care Without Harm (www.hcwh.org) - an international organization that supports sustainability in health care - has a robust program on climate change, including a Healthy Foods in Health Care Program that helps educate dietary/food services and other hospital workers about the health and environmental impacts of food choices. There are many interventions regarding food purchasing that can benefit climate change. For instance, sourcing food from local producers can reduce the carbon footprint created by the long distances that food is transported from farm to table - estimated between 1,500 to 2,500 miles (Worldwatch Institute, 2016).
Nurses have helped to organize farmers’ markets at their hospitals that serves several functions: decreasing food miles, serving affordable fresh produce for hospital staff including many of the low-income workers in health care, supporting local farmers, and providing more food options for those in the surrounding neighborhoods. Serving more plant-based food choices decreases the methane that is associated with meat production and is healthier for patients. Nurses are also involved in the 50by40 Campaign (2019), a recently launched global initiative to reduce meat consumption 50% by 2040. Nurses also are helping to support food policies that call for purchasing organically grown foods, which reduces the use of many fossil fuel-derived, synthetic fertilizers. In addition, organic foods, which are grown without the use of potentially harmful pesticides, decrease health risks for farmworkers’, the environment, and others, thus achieving another set of disease-prevention strategies (Mie et al., 2017). To support and educate nurses, a Food and Agriculture webinar series and initiative was launched by ANHE in 2019.
Nurses have a role in the promotion of community-level resiliency, including helping communities prepare for climate-related impacts such as extreme weather events like fires, floods, and storms. In Montana, Dr. Schenk helped to organize Climate Smart Missoula, which is committed to zero waste, 50% “active” transportation, and 100% clean electricity by 2015 (Climate Smart Missoula, 2019). Another nurse, Lisa Hartmayer, MSN, NP employed the tools provided by the Cool Block Project (https://coolblock.org/) to convene the neighbors on her San Francisco block to support each other in building personal and community-wide resilience and readiness for potential disasters including earthquakes and extreme heat events. In each of these community-based activities the co-benefits of building relationships are invaluable to everyone, but especially to the most vulnerable community residents and those that are often isolated.
Rosemary Chaudry, PhD, MPH, RN, PHNA-BC, CPH has played a critical role in the Ohio Public Health Association’s (OPHA) interdisciplinary Ohio Public Health Climate Resilience Coalition (OPHCRC). The Coalition developed a white paper “Climate Resilience in Ohio - A Public Health Approach to Preparedness and Planning” (OPHA, 2017; OPHCRC, 2017) to assist Ohio’s public health professionals in addressing the health impacts of climate change and climate-related weather events in their jurisdictions. She wrote the white paper’s sections on climate impacts and health equity and ensured that the OPHCRC’s work reflected the OPHA’s policy initiative to advocate for state legislation to adopt a “Health and Equity in All Policies” approach to policy-making (OPHA, 2019; Ohio Senate, 2022; Thoughtwell, OPHA, 2018). Dr. Chaudry’s on-going work with OPHCRC reflects public health nursing standards of practice (Assessment, Consultation, Planning) and performance (Leadership, Ethics, Communication, Collaboration, Environmental Health, and Advocacy) (American Nurses Association, 2013).
In another example, a San Francisco city-wide collaboration that included the Mayor’s Office, Health Department, Senior Social Services, and the University of San Francisco School of Nursing initiated a set of neighborhood-based efforts to identify seniors and people with functional disabilities in order to develop practical plans during extreme heat events. These plans could be easily employed for other types of disasters and the process of creating the plans is helping to build sustainable relationships and thus a more resilient and less isolated community.
Policy and Advocacy
In addition to nurses’ roles in preparing for and responding to increased risks from clinical and public health perspectives, nurses are playing an important role in educating policy-makers at the local, state, and federal levels. In California, a state with a significant fossil fuel sector, Barbara Sattler, RN, DrPH, FAAN and other nurses are part of a state-wide coalition supporting legislation to decrease oil drilling in the state. This advocacy follows on the heels of successful campaigns in New York and Maryland where nurses participated in statewide initiatives to keep hydraulic fracturing or “fracking” out of their states by banning it. In Minnesota, nurses are part of Health Professionals for a Healthy Climate – a collaboration of health professionals focused on addressing climate change in the state – and engaging in advocacy activities such as the 100% Campaign that is focused on moving the state towards an equitable and clean energy future. In Tennessee, Carol Zeigler, DNP, NP-C, RD educates students at Vanderbilt University on the importance of advocacy through an interprofessional course on planetary health, policy, and social justice. Dr. Zeigler is a founding and current member of the Tennessee Climate Network, which focuses on regional cross-sector partnerships and developing a state climate action plan. These examples show the extent and potential for nursing involvement around climate and health beyond the walls of health care.
Nurses and nursing organizations are part of a national coalition of health professionals that are promoting a policy-driven U.S. Call to Action on Climate, Health, and Equity: A Policy Action Agenda (2019) that calls on various sectors of society – civil society, business, health, government, etc. – to act on climate change as a health emergency and to prioritize the actions outlined in the Call to Action. Currently more than 100 health organizations, including ANHE, the American Academy of Nursing and the American Nurses Association, and health systems have endorsed the Call to Action. The elements of the Call to Action’s represent 10 priorities for addressing climate change as an urgent health threat and demands national, state, local, and cross-sector leadership in addressing climate change. See Table 1 for the priority elements of the Call to Action. To view the priority actions in further detail, read the full statement and its associated signatories, and to become a signatory organization visit: climatehealthaction.org.
Table 1 Elements of the U.S. Call to Action on Climate, Health, and Equity: A Policy Action Agenda
|
Elements of the U.S. Call to Action on Climate, Health, and Equity: |
|---|
|
Climate Action for Health Priority Actions 1. Meet and strengthen greenhouse gas emission reduction commitments and support the Paris Agreement 2. Transition rapidly away from the use of coal, oil and natural gas to clean, safe, and renewable energy and energy efficiency 3. Emphasize active transportation in the transition to zero-carbon transportation systems 4. Promote healthy, sustainable and resilient farms and food systems, forests, and natural lands 5. Ensure that all U.S. residents have access to safe and affordable drinking water and a sustainable water supply 6. Invest in policies that support a just transition for workers and communities adversely impacted by climate change and the transition to a low-carbon economy |
|
Health Action for Climate Policy Actions 7. Engage the health sector voice in the call for climate action 8. Incorporate climate solutions into all health care and public health systems 9. Build resilient communities in the face of climate change |
|
Financing Climate Action for Health and Health Action for Climate Priority Action 10. Invest in climate and health |
(2019)
Organizational Leadership: Nursing Collaborative on Climate Change and Health
Climate change, which is considered an existential threat to human existence as we know it, demands nursing engagement and nursing leadership. Professional nursing organizations are called upon to recognize the role of the profession in advancing strategies and solutions (Nicholas & Breakey, 2017). To answer the call for action by nurses, professional associations, and nursing faculty, the Alliance of Nurses for Healthy Environments in partnership with Climate for Health and US-based national nursing organizations formed the Nursing Collaborative on Climate Change and Health (Nursing Collaborative). The Nursing Collaborative is building national nursing leadership on climate change by generating commitments from national nursing organizations to address this issue as a health priority and further engage memberships in climate solutions. There are currently 11 national nursing organizations that are members of the Nursing Collaborative; these organizations represent nurses from various practice settings and specialties and underrepresented groups in nursing. See Table 2 for a full list of Nursing Collaborative member organizations.
Table 2. Nursing Collaborative on Climate Change and Health Member Organizations
|
Nursing Collaborative on Climate Change and Health Member Organizations |
|---|
|
● Alliance of Nurses for Healthy Environments (ANHE) ● American Academy of Nursing (AAN) ● American Association of Occupational Health Nurses (AAOHN) ● Association of Public Health Nurses (APHN) ● Center for Climate Change, Climate Justice, and Health at the MGH Institute of Health Professions ● National Association of Hispanic Nurses (NAHN) ● National Association of Nurse Practitioners in Women’s Health (NPWH) ● National Student Nurses’ Association (NSNA) ● Nurse Alliance of Service Employees International Union Healthcare ● Public Health Nursing Section of the American Public Health Association ● Preventive Cardiovascular Nurses Association (PCNA) |
The activities that these nursing organizations are implementing as part of the Nursing Collaborative effort vary and reflect each member’s mission and vision, nursing specialty, and member interest and engagement. Examples of activities undertaken by the Nursing Collaborative include incorporating climate change into annual meetings, writing organizational position statements or resolutions, forming climate change committees or workgroups, and hosting webinars to educate members. For example, the National Student Nurses’ Association - the premier organization for nursing students in the US - passed a resolution in 2017 titled Increased Nursing Student Action on and Awareness of the Effects of Climate Change on Health and a resolution in 2018 titled In Support of Increasing Awareness on the Effects of Climate Change on Mental Health. Climate Change was the featured topic for their annual meeting in 2018, where over 3,000 nursing student leaders attended (view the plenary talk recording here).
The National Association of Hispanic Nurses has been instrumental in bringing attention to the need to actively address climate change-related health inequities within Latino communities. The Association of Public Health Nurses has provided leadership among public health nurses through the development of position papers outlining the role of public health nurses in disaster preparedness, response, and recovery, and in addressing the public health impacts of climate change. The American Academy of Nursing (AAN) is planning to use the Call to Action document as a guide for their policy work. AAN’s Expert Panel on Public and Environmental Health is also developing a policy position paper on disaster preparation, largely in response to the effects of climate change.
Collective Nursing Leadership on Climate Change as Health Imperative
In October 2018, the Nursing Collaborative, in partnership with Climate for Health, hosted a strategic planning convening of nursing leaders from 12 national organizations and generated four key themes to guide their work over the next 3 to 5 years: 1) engagement, 2) partnerships, 3) communications and messaging, and 4) serving as a resource for addressing climate, health, and nursing. See Table 3 for a summary of the four key themes determined at the convening event.
Table 3. Nursing Collaborative 2018 Convening Event Key Themes
|
Nursing Collaborative on Climate Change and Health |
|
|---|---|
|
Engagement: Deepen engagement and expand outreach to ensure that diverse voices and concerns across the nursing profession are represented in crucial conversations and that efforts are coordinated efforts. |
● Deepen involvement of existing organizational members in climate change activities ● Engage new member nursing organizations |
|
Partnerships: Ensure the perspective of nurses is represented in conversations around climate change and provide opportunities to leverage resources and capacity. |
● Partnerships with non-nursing organizations and disciplines ● Cross-sector/interdisciplinary policy and advocacy efforts |
|
Communications and Messaging: Convey information on climate and health and Nursing Collaborative efforts in a nonpartisan manner. |
● Utilization of a health-messaging frame in climate discussions ● Outreach efforts to showcase nursing leadership around climate and health |
|
Resource for climate, health, and nursing: To provide coordination and unification of climate change efforts across the profession. |
● Serve as a clearinghouse and accessible expert resource on the interrelationship among climate change, health, and nursing ● Justice, diversity, equity, and inclusion are core to efforts |
As an outcome to the Nursing Collaborative convening event, 12 nursing organizations signed-on to a joint statement on climate change and health (ANHE, 2018b). The statement acknowledges the role that nurses have in addressing climate and health-related impacts and outlines the signatories’ commitment to work collaboratively across the profession. The position statement calls for action from nurses and from the nursing profession such as promoting the inclusion of climate change content into nursing educational offerings, supporting sustainable practice environments, educating and informing the public and communities on climate-related impacts, and advocating to advance equitable and just climate policy. The full statement with the list of signers can be accessed at https://envirn.org/joint-statement/.
Conclusion
The seminal report on nursing and the environment (IOM, 1995) recommended that environmental health be integrated into four nursing domains – research, education, practice, and policy/advocacy. This continues to serve as a useful frame and track nursing’s involvement in mitigation and response to climate change. The consequences of climate change are continuing to unfold, and nurses are continuing to find new roles to make a difference in their communities, in their workplaces, and in the halls of power. Nurses’ leadership and trusted voices are essential as we persist in our efforts to help address the causes of climate change, prepare for the predicted human and ecological effects, and care for our patients and communities, especially those who are the most vulnerable. Our collective work through the Nursing Collaborative on Climate Change and Health and other national and international organizations and structures, will allow us to share resources, strengthen our voices, and increase our impact. The criticality of time and urgency of the situation requires nursing’s immediate attention and actions.
Authors
Cara Cook, MS, RN, AHN-BC
Email: cara@envirn.org
ORCID ID: 0000-0002-6669-2746
Cara Cook is the Climate Change Program Coordinator for the Alliance of Nurses for Healthy Environments (ANHE). Her work focuses on elevating climate and health as a national priority by engaging nursing organizations and individual nurses in climate and health advocacy, education, and practice change. Cara gained experience in public health nursing during the completion of a Master of Science in Community/Public Health Nursing through the University of Maryland, in which she focused on environmental health. In addition to a Master of Science, Cara holds a Bachelor of Science in Nursing from the University at Buffalo and a certification as an Advanced Certified Holistic Nurse through the American Holistic Nurses Credentialing Corporation.
Rosemary Valedes Chaudry, PhD, MPH, MHA, RN
Email: rvchaudry@gmail.com
ORCID ID: 0000-0002-0034-612X
Dr. Chaudry has certifications as a public health nurse (PHNA-BC), in public health (CPH), and in healthcare quality (CPHQ). Since her retirement, Rosemary teaches part time but focuses mainly on advocacy for environmental public health issues; for health, equity, and social justice issues in public health; and for issues related to public health nursing practice. Rosemary currently serves as the APHN liaison to the Nursing Collaborative on Climate Change and Health. She also does advocacy as a member of her state nursing association’s Environment & Community Health Caucus, the Ohio Public Health Association, the American Public Health Association, and the Ohio Healthy Homes Network. Her nursing background is in the areas of oncology, home health, public health, and nursing education.
Barbara Sattler, RN, DrPH, FAAN
Email: bsattler@usfca.edu
Dr. Sattler is a Professor at the University of San Francisco School of Nursing and Health Professions and a founding member of the Alliance of Nurses for Healthy Environments. Dr. Sattler started the first environmental health nursing program in the country and continues to educate nurses about a range of environmental health issues including risks through the lifespan, chemical-specific exposures, environmental health patient assessments, and the health effects associated with food and agriculture practices, energy sources, and climate change. She directed a 10-year project to “green” hospitals in Maryland by engaging nurses as change agents and in leadership roles. She is a member of the American Academy of Nursing’s Expert Panel on Environmental and Public Health and the American Association Colleges of Nursing’s Environmental Health Committee. Dr. Sattler is an editor of Environmental Health and Nursing and author of a wide range of journal publications.
References
Adlong, W., & Dietsch, E. (2015). Nursing and climate change: An emerging connection. Collegian, 22(1), 19-24. https://doi.org/10.1016/j.colegn.2013.10.003
Alliance of Nurses for Healthy Environments (ANHE). (2016). Environmental health in nursing. J. Leffers, C.M. Smith, K. Huffling, R. McDermott-Levy, & B. Sattler (Eds.). Alliance of Nurses for Healthy Environments.
Alliance of Nurses for Healthy Environments (ANHE). (2018a). Climate and health toolkit. https://climateandhealthtoolkit.org/
Alliance of Nurses for Healthy Environments (ANHE). (2018b). National nursing organizations commit to climate action. AHNE News. https://envirn.org/joint-statement/
American Nurses Association (ANA). (2013). Public health nursing- Scope and standards of practice (2nd ed.). Nursesbooks.org
American Nurses Association (ANA). (2015). Nursing: Scope and standards of practice (3rd ed.). American Nurses Publishing.
Brulle, R. J., Carmichael, J., & Jenkins, J.C. (2012). Shifting public opinion on climate change: An empirical assessment of factors influencing concern over climate change in the U.S., 2002-2010. Climate Change, 114(2), 169-188. https://doi.org/10.1007/s10584-012-0403-y
California Department of Public Health (CDPH). (2018, August 16). Valley Fever continues to increase in California in 2017. Office of Communications. https://www.cdph.ca.gov/Programs/OPA/Pages/NR18-041.aspx
Centers for Disease Control and Prevention (CDC). (2019, January 2). Where Valley Fever (Coccidioidomycosis) comes from. Fungal Diseases. https://www.cdc.gov/fungal/diseases/coccidioidomycosis/causes.html
Chamberlain, B. (2008). Are you prepared for Malaria? Clinical topics. https://www.myamericannurse.com/are-you-prepared-for-malaria/
Climate Health Action. (2019). U.S. Call to action on climate, health, and equity: A policy action agenda. https://climatehealthaction.org/cta/climate-health-equity-policy/
Climate Smart Missoula. (2019). Climate Smart Missoula. Home, https://www.missoulaclimate.org/
Cook, C., Demorest, S.L, & Schenk, E. (2019). Nurses and climate action. American Journal of Nursing, 119(4), 54-60. https://doi.org/10.1097/01.naj.0000554551.46769.49
50by40 Campaign. (2019). Reducing global meat production 50% by 2040. Home https://50by40.org/
Giddens, J. F., & Brady, D. P. (2007). Rescuing nursing education from content saturation: The case for a concept-based curriculum. Journal of Nursing Education, 46(2), 65-69. https://doi.org/10.3928/01484834-20070201-05
Glaser, J., Lemery, J., Rajagopalan, B, Diaz, H.R., Garcia-Trabanino, R., Taduri, G., … Johnson, R.J. (2016). Climate change and the emergent epidemic of CKD from heat stress in rural communities: The case for heat stress nephropathy. Clinical Journal of the American Society of Nephrology, 11(8), 1472-1483. https://doi.org/10.2215%2FCJN.13841215
Global Consortium on Climate and Health Education. (2019). Global Consortium on Climate and Health Education. About. https://www.mailman.columbia.edu/research/global-consortium-climate-and-health-education
Griggs, C., Fernandez, A., & Callanan, M. (2017). Nursing and the barriers to sustainable health care: A literature review. British Journal of Nursing, 26(22), 1230-1237. https://doi.org/10.12968/bjon.2017.26.22.1230
Health Care Without Harm. (2019, May 3). 2019 Stephanie Davis Waste Reduction and Pollution Prevention Award and Scholarship. News. https://noharm-uscanada.org/articles/news/us-canada/2019-stephanie-davis-waste-reduction-and-pollution-prevention-award
Pachauri, R. K., Allen, M. R., Barros, V. R., Broome, J., Cramer, W., Christ, R., Church, J. A., Clarke, L., Dahe, Q. D., Dasqupta, P., Dubash, N. K., Edenhofer, O., Elgizouli, I., Field, C. B., Forster, P., Friedlingstein, P., Fuglestvedt, J., Gomez-Echeverri, L., Hallegatte, S., ... van Ypersele, J-P. (2014). Climate change 2014: Synthesis report.Contribution of working groups I, II and III to the fifth assessment report of the Intergovernmental Panel on Climate Change. IPCC. http://www.mendeley.com/research/climate-change-2014-synthesis-report-contribution-working-groups-i-ii-iii-fifth-assessment-report-in-20
Institute of Medicine (US) Committee on Enhancing Health Context in Nursing Practice (IOM). (1995). Nursing health, and the environment:Strengthening the relationship to improve the public’s health. National Academy Press. https://doi.org/10.17226/4986
Intergovernmental Panel on Climate Change (IPCC). (2018). Summary for policymakers. In V. Masson-Delmotte, P. Zhai, H.O. Portner, D. Roberts, J. Skea, P.R. Shukla, … T. Waterfield (Eds.), Global warming of 1.5°C: An IPCC Special Report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty. https://doi.org/10.1017/9781009157940.001
International Council of Nurses (ICN). (2018, September 27). International Council of Nurses calls for increased leadership to combat effects of climate change on health. News. https://www.icn.ch/news/international-council-nurses-calls-increased-nursing-leadership-combat-effects-climate-change
Lilienfeld, E., Nicholas, P. K., Breakey, S., & Corless, I. B. (2018). Addressing climate change through a nursing lens within the framework of the United Nations Sustainable Development Goals: A scoping review. Nursing Outlook, 66(5), 482-494. https://doi.org/10.1016/j.outlook.2018.06.010.
Maibach, E., Myers, T., & Leiserowitz, A. (2014). Climate scientists need to set the record straight: There is a scientific consensus that human-caused climate change is happening. Earth’s Future, 2(5), 295–298. https://doi.org/10.1002/2013EF000226
Mie, A., Andersen, H. R., Gunnarsson, S., Kahl, J., Kesse-Guyot, E., Rembialkowska, Quaglio, G., & Grandjean, P. (2017). Human health implications of organic food and organic agriculture: A comprehensive review. Environmental Health, 16, 111. https://doi.org/10.1186/s12940-017-0315-4
National Aeronautics and Space Administration (NASA). (2018). Understanding our planet to benefit humankind. Vital signs of the planet. https://climate.nasa.gov/
Nicholas, P. K., & Breakey, S. (2017). Climate change, climate justice, and environmental health: Implications for the nursing profession. Journal of Nursing Scholarship, 49(6), 606-616. https://doi.org/10.1111/jnu.12326
Ohio Public Health Association (OPHA). (2019). Health & equity in all policies of OPHA’s work. News. https://ohiopha.org/health-equity-in-all-policies-a-focus-of-ophas-work/
Ohio Public Health Association (OPHA). (2017). Climate resilience in Ohio: A public health approach to preparedness and planning. https://ohiopha.org/wp-content/uploads/2022/02/ClimateResilienceInOhio.pdf
Ohio Senate, 133rd General Assembly. (2022). Senate Bill No. 302. Legislation. http://www.ohiosenate.gov/legislation/GA132-SB-302
Richardson, J., Grose, J., Doman, M., & Kelsey, J. (2014). The use of evidence-informed sustainability scenarios in the nursing curriculum: development and evaluation of teaching methods. Nurse Education Today, 34(4), 490-3, 490-3. https://doi.org/10.1016/j.nedt.2013.07.007
Riley, K., Wilhalme, H., Delp, L., and Eisenman, D. P. (2018). Mortality and morbidity during extreme heat events and prevalence of outdoor work: An analysis of community-level data from Los Angeles. International Journal of Environmental Research and Public Health, 15(4), 580. https://doi.org/10.3390/ijerph15040580
Sweeney, N. M. & de Peyster, A. (2005). Integrating environmental health into an undergraduate community health nursing course. Public Health Nursing, 22(5), 439-44. https://doi.org/10.1111/j.0737-1209.2005.220509.x
Thoughtwell, Ohio Public Health Association. (2018). Health and equity in all policies (HEiAP)- Enacting HEiAP: Literature review and case studies. https://www.thoughtwell.org/projects/2018/6/21/health-and-equity-in-all-policies-heiap-enacting-heiap-literature-review-and-case-studies
U.S. Global Climate Research Program. (2018). Impacts, risks, and adaptation in the United States: Fourth national climate assessment, volume II: Report-in-brief. D.R. Reidmiller, C.W. Avery, D.R. Easterling, K.E. Kunkel, K.L.M. Lewis, T.K. Maycock, and B.C. Stewart (Eds.). U.S. Global Change Research Program. https://toolkit.climate.gov/reports/impacts-risks-and-adaptation-united-states-fourth-national-climate-assessment-volume-ii
Watts, N., Amann, M., Arnell, N., Ayeb-Karlsson, S., Belesova, K., Berry, H., Bouley, T., Boykoff , M., Byass, P., Cai, W., Campbell-Lendrum, D., Chambers, J., Daly, M., Dasandi, N., Davies, M., Depoux, A., Dominguez-Salas, P., Drummond, P., Ebi, K. L., … Costello, A. (2018). The 2018 report of the Lancet Countdown on health and climate change: Shaping the health of nations for centuries to come. The Lancet, 392(10163), 2479-2514. https://doi.org/10.1016/s0140-6736(18)32594-7 4-9
Whitehead, D. (2007). Reviewing health promotion in nursing education. Nurse Education Today, 27(3), 225-237. https://doi.org/10.1016/j.nedt.2006.05.003
Worldwatch Institute. (2016, March 3). Globetrotting food will travel further than ever this Thanksgiving. Vital Signs Online. https://perma.cc/58SK-77G6


