Increased utilization of videoconferencing platforms to conduct meetings and patient encounters has illuminated the need to focus on video etiquette. Though telehealth has been utilized since the 1950s, the SARS-COV-2 (COVID-19) pandemic propelled virtual care into the forefront of healthcare to protect both patients and providers. Historically, few academic programs have incorporated telehealth into the curriculum, and the rapid transition to telehealth typically left providers to learn the art of virtual care without education. The experience of many nurse providers is often limited to virtual platforms typically used for casual interactions versus a successful patient encounter. A quality telehealth encounter that enhances patient-provider communication and strengthens the provider-patient relationship must include telehealth etiquette and webside manner. This article describes the PEP framework for telehealth encounters to provide a detailed description of the elements of performance, environment, and privacy/security as best practices to underpin successful virtual health visits.
Key Words: Telehealth etiquette, webside manner, Advanced Practice Nursing, nursing, telehealth, telehealth education, telemedicine, nursing education, nurse patient experience, telehealth nursing, nursing faculty, telehealth quality
Increased utilization of videoconferencing platforms to conduct meetings and patient encounters has illuminated the need to focus on video etiquette.
Increased utilization of videoconferencing platforms to conduct meetings and patient encounters has illuminated the need to focus on video etiquette. What many people assume will be easy, or come naturally, often does not. There is a fine line between inappropriate video etiquette and offenses that may lead to termination of employment; thus, every video encounter should be met with professionalism to prevent avoidable missteps.
Successful encounters require participants to have an intentional focus on video etiquette.
Many may remember the Good Morning America reporter caught broadcasting in boxer briefs or the California commissioner who resigned after throwing his cat while on a video call (Shein, 2020). These faux pas may seem egregious, yet there are many other potential lapses in video etiquette that diminish the quality of the interaction and increase the risk of negative repercussions such as losing one’s job or creating a negative patient-provider experience. Without specific education on important details of appropriate video etiquette, providers risk providing ineffective telehealth encounters. Successful encounters require participants to have an intentional focus on video etiquette. The purpose of this article is to present a telehealth etiquette framework that can be used by nurses, providers, and educators to improve the delivery of telehealth.
Telehealth
Brief History of Telehealth
Telehealth, as defined by the U. S. Health Resources and Services Administration (HRSA), is “the use of electronic and telecommunication technologies to support long-distance clinical health care, patient and professional health-related education, public health, and health administration” (U. S. Department of Health and Human Services [DHHS], 2021, para 1). Telehealth encompasses a variety of technologies including real-time audio-video interaction, store-and-forward communications, streaming media and wireless communications (HRSA, 2020).
The pandemic may prove to be the most significant facilitator of telehealth utilization since its inception.
Telehealth is not new. The first mention of telehealth in the literature was in the February 1925 issue of Science and Invention magazine when Hugo Gernsback envisioned a device, he called the “teledactyl” for the year 1975 that would allow a physician to see and feel from a distance (Novak, 2012). Actual use of telehealth began in the late 1940s with the transmission of radiologic images by telephone, with video transmission following in 1959 (Institute of medicine [IOM], 1996). Growth in telehealth utilization continued to be slow until the advent of the COVID-19 pandemic which catapulted telehealth into the forefront of medicine to provide healthcare while reducing exposure to the SARS-CoV-2 virus for both patients and providers. The pandemic may prove to be the most significant facilitator of telehealth utilization since its inception. Some anticipate a seven-fold increase in the telehealth market by 2025 beginning with a year-over-year increase in 2020 of 64.3% (Imaging Technology News, 2020).
Historically, few nursing programs have incorporated telehealth into the healthcare curriculum
Telehealth and Providers
As a result of this rapid expansion of telehealth, providers, including Advanced Practice Registered Nurses (APRNs), were thrust into caring for patients virtually with little to no telehealth education or training. Historically, few nursing programs have incorporated telehealth into the healthcare curriculum (Rutledge et al., 2017). Furthermore, there is no consistency among health professions training programs regarding the content that is included (Chike-Harris et al., 2020). Prior to the COVID-19 pandemic, lack of education and training was cited as the primary barrier to telehealth provider adoption (Mozer et al, 2015). Though the pivot from in-person care to virtual care to protect the health and safety of the public may have appeared successful, the patient and provider experience may have suffered due to this lack of provider training in telehealth.
The idea that these platforms prepare clinicians to provide virtual care is false
Most clinicians who transitioned to virtual care had prior experience only with platforms such as Zoom, FaceTimeR or SkypeR, which are typically used for more casual interactions than those required for a successful patient encounter. The idea that these platforms prepare clinicians to provide virtual care is false (Sharma et al, 2019). In fact, the casual use of social media for interpersonal interactions may have a negative effect on professional telehealth communication by reducing one’s empathetic expression (Konrath et al., 2011) and one’s ability to recognize nonverbal cues (Mullen, 2011).
New graduates may be among those who struggle to conduct successful telehealth encounters because they are not yet proficient with their in-person skills. However, even seasoned providers may benefit from education specific to conducting a virtual visit. Thorough education about important skills necessary to conduct successful telehealth encounters may enhance long term provider satisfaction with telehealth, patient outcomes, and the patient-provider relationship.
Telehealth etiquette does not refer to “what” care is delivered...
Telehealth Etiquette and Webside Manner
Essential to a successful telehealth encounter is telehealth etiquette. Telehealth etiquette does not refer to “what” care is delivered virtually, but rather “how” that care is delivered. The standard of care remains unchanged when care is provided virtually. Telehealth etiquette refers to the critical soft skills necessary to conduct a successful telehealth visit (Gustin et al., 2019) and is inclusive of “webside manner.” Bedside manner, a skill that receives focus in great detail during healthcare training, refers to a clinician’s way of interacting with patients to make them feel comfortable. The term webside manner, a skill that is rarely taught, refers to similar behaviors occurring through care via videoconference (McConnochie, 2019). Essential to a strong bedside or webside manner, and thus to establishing a therapeutic patient relationship, is effective communication incorporated with active listening (Jagosh et al., 2011; Chichirez & Purcarea, 2018).
Patient-Provider Communication
Impact of Communication
Communication has long been a key component of education for nurses and is identified by the National Council of State Boards of Nursing (NCSBN) as fundamental to the practice of nursing (NCSBN, 2013). Communication competency contributes to establishing a trusting, collaborative relationship with patients, families, and caregivers (Arnold & Boggs, 2019). Foundational to communication that enhances the emotional state of another person is the expression of genuine warmth, accurate empathy, and unconditional positive regard (Rogers, 1957).
The patient-provider relationship has also been shown to have a significant effect on healthcare outcomes
Establishing a patient-provider relationship on the foundation of trust enhances patient understanding and acceptance of the diagnosis and treatment plan and encourages patients to follow the guidance offered by the clinician (McConnochie, 2019). The patient-provider relationship has also been shown to have a significant effect on healthcare outcomes (Kelley et al., 2014; Matusitz & Spear, 2014). Atul Gawande (2007), a surgeon and observer of medical behavior and practice, emphasized the importance of the social interaction with patients when he stated:
"It is unsettling how little it may take to defeat success in medicine. You come as a professional equipped with expertise and technology. You do not imagine that a mere matter of etiquette could foil you. But the social dimension turns out to be as essential as the scientific matter of how casual you should be, how formal, how reticent, how forthright. In this work against sickness, we begin not with genetic or cellular interactions but with human ones" (p. 81-82).
Recently, communication has been identified as a key driver to patient likelihood of recommending a specific care provider or recommending a video visit (Press Ganey, 2020b). Specifically, if a care provider expressed concerns for the patient’s questions or worries, made effort to include the patient in decisions, and provided an explanation of the patient’s illness and treatment, the patient was 98.7% likely to recommend the care provider. In addition, patients were 96.3% likely to recommend a video visit if the video visit staff worked together to provide care, it was easy to speak with the care provider over video, and the video connection was strong (Press Ganey, 2020b).
...virtual encounters require a different set of communication competencies than those of in-person care.
New Skills for Virtual Communication
Communication skills vary significantly among individuals and are influenced by personality and life experience (McConnochie, 2019). While professionalism and communication are part of nursing education, virtual encounters require a different set of communication competencies than those of in-person care. For example, quality and safety depend on strong education and training (van Galen et al., 2019). Ensuring dedicated attention to telehealth etiquette and webside manner is essential to enhance the quality of virtual encounters for patients and care providers. Visual information in the form of a framework enhances learning through stimulating visual thinking, which promotes understanding and information retention (Raiyn, 2016). Change to a framework that addresses this process can help providers and educators to effectively address all components of telehealth etiquette.
PEP Framework for Telehealth Encounters
Telehealth etiquette encompasses a variety of factors and behaviors beyond that of typical professional conduct to ensure successful telehealth encounters (Rutledge et al., 2020). The PEP framework (see Figure) highlights three crucial elements of telehealth etiquette: 1) performance, 2) environment, and 3) privacy/security.
Figure. PEP Framework for Telehealth Encounters
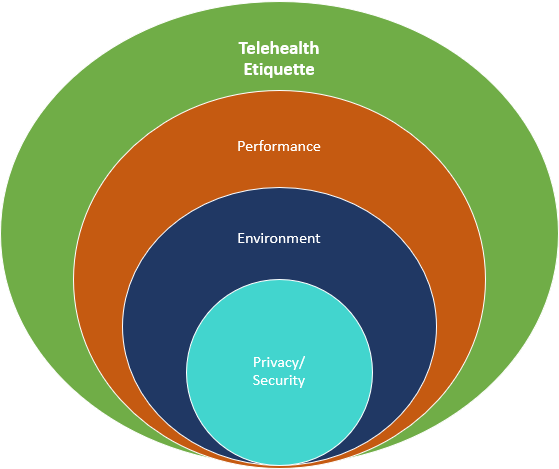
Each element of the framework encompasses essentials needed for a successful telehealth encounter (see Table). Using the PEP framework to model a comprehensive approach for telehealth etiquette can ensure that key elements of the virtual encounter are prioritized to enhance the patient and provider experience and improve patient outcomes.
Table. PEP Framework for Telehealth Encounters with Essential Components
| Element |
Essentials |
|
Performance |
|
|
Environment |
|
|
Privacy/ Security |
|
P - Performance
Performance encompasses professionalism, communication, and technology proficiency. To enhance patient perception of professionalism, it is essential that providers maintain professional behavior consistent with that provided during in-person encounters. For example, greeting the patient, establishing rapport, and setting the stage for the visit are key.
Communication Skills in Telehealth. Relationship centered communication skills are among the most important elements of an effective telehealth encounter. Successful telehealth encounters that enhance the patient provider relationship and patient satisfaction require an understanding about how to overcome technology barriers to project respect, empathy, and communication (Gustin et al., 2019). Patient-centered communication patterns, including expressions of empathy and praise, have been shown to be fewer during telehealth encounters than in-person encounters (Liu et al., 2007). Telehealth encounters also require providers and patients to have heightened attention to compensation for missing environmental cues (van Galen et al., 2019) and nonverbal communication.
Relationship centered communication skills are among the most important elements of an effective telehealth encounter.
Established by Albert Mehrabian in 1971, and widely used today, the 7-38-55 rule indicates that seven percent of meaning is communicated through spoken word, 38 percent through voice tone, and 55 percent through body language (Mehrabian, 1971). Telehealth encounters limit the ability of participants to interpret body language such as gestures, subtle movements, and posture. Tone of voice, inflection, and pitch also may not be fully appreciated virtually. These limitations, along with the absence of the ability to communicate through touch, provide inherent challenges to successful telehealth communication and require intentional effort by providers to overcome them.
Best Practices for Telehealth Visit Professionalism. It is important to initiate the encounter on time (Lafolla, 2015). At the beginning of the visit, providers must ensure they are positioned properly on the screen by checking the self-view. Recommended is the “passport view” with the head and top of shoulders centered in the field of view to facilitate communication, eye contact, and respect for the patient’s personal space (American Telemedicine Association [ATA], 2018). Confirm that the patient can see and hear you before conducting the encounter. Begin with an introduction and identify your facility. A confident introduction may foster trust and initiate rapport (Press Ganey, 2020a). Set the agenda for the visit by identifying patient priorities and concerns and summarizing the plan for the visit. Speak clearly and at a slower pace than normal to ensure clear enunciation and clarity (Sharma et al., 2019). It is helpful to wait two to three seconds to respond as there may be lag time between when the patient speaks and when the audio is received (Lafolla, 2015). As with an in-person visit, providers should avoid eating, chewing gum, or drinking during visits.
Confirm that the patient can see and hear you before conducting the encounter.
Best practices for virtual communication begin with eye contact. Providers should look into the camera rather than at the patient image or self-view on the screen. Eye contact has been shown to increase patient perception of the clinician’s level of empathy (Montague et al., 2013) and to serve as an important nonverbal cue (Gustin et al., 2019). Individuals may be sensitive to shifts in gaze, so it is helpful to maintain a direct gaze without staring by shifting occasionally from the eyes to the forehead (Press Ganey, 2020a; Tam et al., 2007). Additionally, it is essential to consider cultural, gender, and age preferences for direct versus indirect eye contact (Press Ganey, 2020a; ATA, 2016). If looking away from the screen, explain why. Inform patients if viewing a different screen for purposes of charting or reviewing records and minimize the amount of time spent diverting one’s gaze away from the patient. Be sure to look into the correct camera if using multiple screens. Inadvertently using the wrong camera may create distance between the provider and patient. While they may not comment, do not be surprised if a patient, especially a child, lets you know when you are not looking at them. They may say, “Hey, who are you looking at? You’re not looking at me!”
Eye contact has been shown to increase patient perception of the clinician’s level of empathy...
Be authentic and genuine throughout the visit and use nonverbal cues such as leaning in, nodding, and intentionally using facial expressions to deliberately convey warmth, interest, concern, and empathy (Gustin et al., 2019). Be sure to engage with the patient and offer introductory remarks and small talk in the same manner as in-person encounters.
Once the visit is ended, the patient typically cannot reconnect to the provider.
Before concluding the visit, an opportunity must be provided for the patient and care giver to ask questions. During in-person encounters, there is often a “by the way” question as the provider reaches for the door. Virtual encounters do not afford patients this opportunity. Once the visit is ended, the patient typically cannot reconnect to the provider. Summarizing the plan of care and post visit plan, providing clear follow up instructions, and ensuring the patient has a mechanism to reach the provider following the visit are important to complete a successful telehealth encounter (Press Ganey, 2020).
Technology Skills. Telehealth providers must be proficient in the technology used to conduct encounters. Not only must they be familiar with that at the distant site, but also with the technology at the originating or patient site. Providers must be comfortable with trouble shooting technology issues at both locations and have easy and quick access to technology support when needed. In addition to understanding how to operate the telehealth technology, providers and telepresenters must be proficient in how to conduct a virtual exam, particularly if using peripheral devices such as digital stethoscopes, otoscopes, and exam cameras. It is helpful for providers to use descriptive anatomical terminology, rather than medical jargon, when guiding a telepresenter through the physical exam to ensure clear communication.
...providers and telepresenters must be proficient in how to conduct a virtual exam, particularly if using peripheral devices...
E – Environment
The environment should be free from visual and audio distractions. Background, lighting, and framing are essential components of a virtual encounter (Sharma et al., 2019). Lighting is best behind the camera, rather than behind providers, to avoid casting a shadow and ensure that they can be seen clearly (Press Ganey, 2020a). Providers must have a well-groomed, professional appearance, wear identification at eye level and wear a lab coat (Haney et al., 2015) or other clothing typically associated with the clinician’s role. Solid clothes with a neutral background project best in a virtual encounter (Sharma et al, 2019).
Backgrounds should be clean and free of clutter and inappropriate items (Calm, 2016; Rutledge et al., 2020). An ideal setting includes the provider sitting at a desk or table with identifying information such as a diploma or the institution name in the background. A portable screen with the organization/company logo is an excellent option for both home and office locations. If using a virtual background, be sure to consider the image that is being projected. While images can be helpful, they can also provide distractions. Avoid a background image that is not consistent with a professional clinical encounter, such as those that make the provider appear to be at the beach or in outer space. Even a blurred background can present problems.
If using a virtual background, be sure to consider the image that is being projected.
Avoid auditory distractions, such as keyboarding and tapping pens, as they may be amplified by the microphone during telehealth visits (Gustin et al., 2019). Cell phone and email alerts should be turned off during visits. If working remotely, there should be no music, television, or other noise in the background. Doors to the provider location should be closed and a “do not disturb” sign posted to alert others that a visit is in progress (Gustin et al., 2019). Noise cancelling devices placed at the doorway are an excellent method to muffle sounds during a visit in busy locations. While it may not be possible in emergency situations, pets should generally not be allowed in the room while conducting an encounter. Even the most well-behaved pet can suddenly cause a distraction through barking, vomiting, or jumping up onto the provider.
Technology placement is also a key component of the environment. Placing the computer and camera on a stable platform reduces risk of wobbling during a visit (Press Ganey, 2020a). The webcam should be placed at eye level or above the face at a seven-degree viewing angle to accurately estimate gaze (ATA, 2018). Use a Wi-Fi sufficient to support the connection without interruption or alternatively, a wired ethernet connection. Ideally, conduct a test connection prior to initiating the patient encounter to ensure that the technology works properly.
P - Privacy/Security
The third element of the PEP framework for telehealth etiquette is privacy/security. Privacy and security are key considerations for telehealth encounters. It is best practice to use a Health Insurance Portability and Accountability Act (HIPAA) compliant and secure platform for telehealth encounters and to utilize vendors who will enter into a HIPAA business associate agreement (BAA) in connection with the technology (DHHS, 2021). While some exceptions were made during the COVID-19 public health emergency to allow for rapid transition to telehealth for providers who did not have access to secure platforms (DHHS, 2021), this does not replace long term solutions for best practices to protect patient information. Consent should be confirmed, and patients should be reassured that the area from which the visit is taking place is secure prior to commencing the encounter (Gustin et al., 2019).
During telehealth encounters, patients and providers should identify anyone else present and confirm permission for participation in the visit (Gustin et al., 2019). Additionally, to ensure that the correct patient is being evaluated and to prevent fraud, providers should confirm patient identity via physical identification (if unknown) before beginning the visit.
Telehealth providers should secure their location by ensuring they are in a private space with the door closed.
Telehealth providers should secure their location by ensuring they are in a private space with the door closed. To further protect patient privacy, headphones with a microphone should be used to conduct the encounter rather than speaker phone or the built-in speaker on the computer. This not only enhances privacy, but also enhances the quality of the communication.
Conclusion
The PEP framework for telehealth encounters provides a comprehensive approach to the crucial components of telehealth etiquette necessary to enhance the patient and provider experience, patient satisfaction, and patient outcomes. Nurses and APRNs may be experts in providing in-person care but may lack knowledge and expertise necessary to transition these skills successfully to the virtual patient encounter. Education about the key components of telehealth etiquette may not only enhance the quality of the virtual encounter, but also strengthen the nurse-patient relationship while ensuring a positive experience for all. Health professions students learning to provide virtual care as part of their curricula will also benefit from specific guidance on telehealth etiquette to ensure a seamless transition into telehealth practice.
Education about the key components of telehealth etiquette may not only enhance the quality of the virtual encounter, but also strengthen the nurse-patient relationship...
This etiquette framework can be easily used to develop clinical case studies and standardized patient experiences. Utilizing the PEP framework for telehealth encounters will guide development of educational content and actions of providers as they conduct virtual visits by ensuring that all important components of telehealth etiquette are addressed.
Authors
Kelli Garber, DNP, APRN, PPCNP-BC
Email: garberk@musc.edu
ORCID ID: 0000-0002-6841-6526
Dr. Garber has over 25 years of experience as a pediatric nurse practitioner providing primary care to children from birth to 21 years of age. She has been providing care via telehealth to children across the state of South Carolina in the school setting through synchronous virtual encounters as well as direct to patients via a virtual urgent care platform for the past 7 years. She has dedicated herself to preserving the patient-provider experience and quality of care provided via telehealth by developing, implementing and sharing best practices for telehealth care. Dr. Garber is a published author and has delivered over 50 local, state and national presentations on the subjects of telehealth and related quality of care, telehealth related health policy, telehealth etiquette, school-based telehealth and Advanced Practice Registered Nurse (APRN) telehealth practice. She has also worked collaboratively with several universities to integrate telehealth education into graduate nursing programs. Dr. Garber is passionate about telehealth and educating the current and future healthcare workforce on preserving the quality of care and enhancing the patient-provider experience during the virtual encounter. Dr. Garber is Chair of the Health Policy Committee for the National Association of Pediatric Nurse Practitioners (NAPNAP) and represents NAPNAP as the Liaison to the Executive Committee of the American Academy of Pediatrics Section on Telehealth Care. She is also a member of the South Carolina Board of Nursing. Dr. Garber received a BSN from the Johns Hopkins University, an MSN from the University of Maryland and a DNP from Old Dominion University.
Tina Gustin, DNP, CNS, RN
Email: tgustin@odu.edu
ORCID ID: 0000-0002-9520-6583
Tina Gustin has over 35-years of advanced practice nursing experience. She is an Associate Professor at Old Dominion University (ODU) School of Nursing where she teaches in the Doctor of Nursing Practice Program. She is Director of the school’s Center for Telehealth Innovation, Education, and Research (C-TIER). The center serves as a telehealth learning hub and research center for the state and East Coast Region of the US. She is the clinical manager for the Pediatric Telehealth program at Children’s Hospital of the King’s Daughters in Norfolk Virginia. Dr. Gustin was responsible for the development of this new program and assuring clinical competence of the telehealth providers. She is the PI and Co-PI for several HRSA grants totaling over 6 million dollars to reach rural and underserved populations though telehealth and interprofessional collaboration. Dr. Gustin has extensively published and presented on both interprofessional team-based care and preparing providers for telehealth both nationally and internationally. She served on the ANA task force for technology and was elected to the Center for Telehealth and eHealth Law (CTeL) Advisory Board. She currently chairs the Telehealth Education Taskforce for CTeL. She has assisted several nursing and medical schools in the development of a telehealth curriculum.
Carolyn Rutledge, PhD, FNP-BC
Email: crutledg@odu.edu
Carolyn Rutledge is Professor and Associate Chair of the School of Nursing at Old Dominion University (ODU). She is the director of the online Doctor of Nursing Practice (DNP) program at ODU, which ranks 15th in the nation. Dr. Rutledge is also a Professor of Family Medicine at Eastern Virginia Medical School where she maintained an active clinical practice for 32 years and served in a faculty role for the medical school, family practice residency, and faculty development. Dr. Rutledge has published over 60 articles and served as an investigator on 32 successful grant applications totaling over $23 million with a primary focus on utilizing new models of care such as telehealth to provide care to rural and underserved populations. Since 2010, Dr. Rutledge has focused on improving the way healthcare is delivered in remote areas using telehealth to enhance patient care and communication. She was the lead in developing the NONPF position paper on educating Nurse Practitioners in telehealth. She is a national consultant in the area of telehealth education and has a book, “Telehealth Essentials for Advanced Practice Nursing”. She currently serves as the Academic Director of the Center for Telehealth Innovation, Education, and Research (C-TIER) at ODU. In 2014, Dr. Rutledge received the SCHEV Outstanding Faculty Award, the highest honor provided to faculty in Virginia.
References
American Telemedicine Association (ATA). (2018, October 3). A concise guide for telemedicine practitioners: Human factors quick guide eye contact. Resources. https://www.americantelemed.org/resources/a-concise-guide-for-telemedicine-practitioners-human-factors-quick-guide-eye-contact/
Arnold, C., & Boggs, K. (2019). Interpersonal Relationships: Professional communication skills for nurses (8th ed.). Elsevier Health Sciences.
Calm, P. (2016). The Polycom guide to vidiquette. Resources. https://utn.org/resources/downloads/polycom-vidiquette-guide-enus.pdf
Chichirez, C. M., & Purcărea, V. L. (2018). Interpersonal communication in healthcare. Journal of Medicine and Life, 11(2), 119–122. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6101690/
Chike-Harris, K., Durham, C., Logan, A., Smith, G., & DuBose-Morris, R. (2020). Integration of telehealth education into the health care provider curriculum: A review. Telemedicine Journal and e-Health, 27(2). https://doi.org/10.1089/tmj.2019.0261
Gawande, A. (2007). Better: A surgeon’s notes on performance. Metropolitan Books.
Gustin, T. S., Kott, K., & Rutledge, C. (2019). Telehealth etiquette training: A guideline for preparing interprofessional teams for successful encounters. Nurse Educator, 45(2), 88–92. https://doi.org/10.1097/nne.0000000000000680
Haney, T., Kott, K., & Fowler, C. (2015). Telehealth etiquette in home healthcare: The key to a successful visit. Home healthcare now, 33(5), 254–259. https://doi.org/10.1097/NHH.0000000000000228
Imaging Technology News (ITN). (2020, May 13). Telehealth to experience massive growth due to COVID-19. Teleradiology. https://www.itnonline.com/content/telehealth-experience-massive-growth-due-covid-19
Institute of Medicine (IOM). (1996). Telemedicine: A guide to assessing telecommunications for health care. [Report]. National Academies Press. https://doi.org/10.17226/5296
Jagosh, J., Boudreau, J. D., Steinert, Y. MacDonald, M. E., & Ingram, L. (2011). The importance of physician listening from the patients’ perspective: Enhancing diagnosis, healing, and the doctor-patient relationship. Patient Education and Counseling, 85(3), 369-374. https://doi.org/10.1016/j.pec.2011.01.028
Kelley, J. M., Kraft-Todd, G., Schapira, L., Kossowsky, J., & Riess, H. (2014). The influence of the patient-clinician relationship on healthcare outcomes: A systematic review and meta-analysis of randomized controlled trials. PloS ONE, 9(4), e101191. https://doi.org/10.1371/journal.pone.0101191
Konrath, S., O’Brien, E., & Hsing, C. (2011). Changes in dispositional empathy in American college students over time: A meta-analysis. Personality and Social Psychology Review, 15(2), 180–198. https://doi.org/10.1177/1088868310377395
Lafolla, T. (2015, December 15). Ten telemedicine etiquette tips to deliver professional care. Resources. https://blog.evisit.com/virtual-care-blog/10-telemedicine-etiquette-tips-deliver-professional-care
Liu, X., Sawada, Y., Takizawa, T., Sato, H., Sato, M., Sakamoto, H., Utsugi, T., Sato, K., Sumino, H., Okamura, S., & Sakamaki, T. (2007). Doctor-patient communication: A comparison between telemedicine consultation and face-to-face consultation. Internal Medicine, 46(5), 227–232. https://doi.org/10.2169/internalmedicine.46.1813
Matusitz, J., & Spear, J. (2014). Effective doctor-patient communication: An updated examination. Social Work in Public Health, 29(3), 252–266. https://doi.org/10.1080/19371918.2013.776416
McConnochie K. M. (2019). Webside manner: A key to high-quality primary care telemedicine for all. Telemedicine journal and e-Health, 25(11), 1007–1011. https://doi.org/10.1089/tmj.2018.0274
Mehrabian, A. (1971). Silent Messages. Wadsworth Publishing Company.
Montague, E., Chen, P., Xu, J., Chewning, B., Barrett, B. (2013). Nonverbal interpersonal interactions in clinical encounters and patient perceptions of empathy. Journal for Participatory Medicine,14 (5), e33. https://participatorymedicine.org/journal/evidence/2013/08/14/nonverbal-interpersonal-interactions-in-clinical-encounters-and-patient-perceptions-of-empathy/
Mozer, R., Bradford, N., Caffery, L., & Smith, A. (2015). Identifying perceived barriers to videoconferencing by rehabilitation medicine providers. Journal of Telemedicine and Telecare, 21(8), 479-484. https://doi.org/10.1177/1357633X15607136
Mullen, J. (2011). The impact of computer use on employee performance in high-trust professions: Re-examining selection criteria in the internet age. Journal of Applied Social Psychology, 41(8), 2009-2043. https://doi.org/10.1111/j.1559-1816.2011.00790.x
National Council of State Boards of Nursing (NCSBN). (2013). NCLEX-RN detailed test plan. NCLEX & Other Exams.https://www.ncsbn.org/publications/2013-NCLEX-RN-Test-Plan-Basic
Novak, M. (2012/ March 14). Telemedicine predicted in 1925. History. https://www.smithsonianmag.com/history/telemedicine-predicted-in-1925-124140942/
Press Ganey (2020a). What are best practices for conducting video/phone appointments with patients? https://www.pressganey.com/docs/default-source/default-document-library/four-essentials-of-effective-telemedicine7bfed85d82706b31bd87ff0000a8abfc.pdf
Press Ganey (2020b). The Rapid transition to telemedicine insights and early trends. https://www.matrc.org/wp-content/uploads/2020/04/Press-Ganey-Telemedicine_-1.pdf?e3e490&e3e490
Raiyn, J. (2016). The role of visual learning in improving students’ high-order thinking skills. Journal of Education and Practice, 7(24), 115-121. https://files.eric.ed.gov/fulltext/EJ1112894.pdf
Rogers, C. (1957). The necessary and sufficient conditions of therapeutic personality change. Journal of Consulting and Clinical Psychology, 21(2), 95-103. https://psycnet.apa.org/doi/10.1037/h0045357
Rutledge, C., Gustin, T., & Schweickert, P. (2020). Telehealth competencies: Knowledge and skills. In C. Rutledge & P. Schweickert (Eds.), Telehealth Essentials for Advanced Practice Nursing (pp 171-191). SLACK Incorporated.
Rutledge, C. M., Kott, K., Schweickert, P. A., Poston, R., Fowler, C., & Haney, T. S. (2017). Telehealth and eHealth in nurse practitioner training: Current perspectives. Advances in Medical Education and Practice, 8, 399-409. https://doi.org/10.2147/AMEP.S116071
Sharma, R., Nachum, S., Davidson, K. W., Nochomovitz, M. (2019). It’s not just FaceTime: Core competencies for the medical virtualist. International Journal of Emergency Medicine, 12(8). https://doi.org/10.1186/s12245-019-0226-y
Shein, E. (2020, May 8). How your actions on zoom could get you fired. TechRepublic. https://www.techrepublic.com/article/how-your-actions-on-zoom-could-get-you-fired/
Tam, T., Cafazzo, J. A., Seto, E., Salenieks, M. E., & Rossos, P. G. (2007). Perception of eye contact in video teleconsultation. Journal of telemedicine and telecare, 13(1), 35-39. https://doi.org/10.1258/135763307779701239
S. Department of Health Resources and Services Administration (HRSA). (2020). Telemedicine and telehealth. HealthIT.gov. https://www.healthit.gov/topic/health-it-health-care-settings/telemedicine-and-telehealth
U.S. Department of Health and Human Services (DHHS). (2021). Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. HIPAA. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html
Van Galen, L. S., Wang, C. J., Nanayakkara, P. W. B., Paranjape, K., Kramer, M. H. H., & Car, J. (2019). Telehealth requires expansion of physician’s communication competencies training. Medical Teacher, 41(6), 714-715. https://doi.org/10.1080/0142159x.2018.1481284


