The use of virtual reality and other technology mediated simulations is in early stages. Guidelines and protocols are still being developed. However, much of what we have used in other forms of simulation can be successfully adapted and implemented. This article will highlight selected areas for use of virtual reality in nursing education. Current literature describes the evidence in this area that includes immersive and desktop virtual realities. Both modalities provide an experiential learning platform that has demonstrated gains in knowledge acquisition and effective learning outcomes. There are several options available to use virtual reality in nursing education. Appropriate educational frameworks and alignment of the virtual reality experience with learning outcomes are important considerations. Infrastructure and support for immersive or desktop virtual reality will look different. It is beneficial to collaborate with instructional technology support staff early in the process as options are explored. Overall, technology mediated simulations using virtual reality is a promising new area for nurse educators. A thoughtful, informed approach can facilitate positive learner experiences and strong outcomes.
Key Words: simulation, nursing education, virtual reality, augmented reality, mixed reality, desk virtual reality simulation, immersive virtual reality simulation, technology medicated simulations
Simulation has been an integral part of the nursing education curriculum for many years and has integrated high level technology since the 1990s (Aebersold, 2016). As the use of technology driven simulators (i.e., manikins) has increased, educators have increased their knowledge and skills and incorporated best practices and standards to create, facilitate, and debrief a variety of simulations. Many schools have robust simulation programs using manikins, standardized patients, and task-trainers. As the technology options increases, computer-based simulations such as virtual and augmented reality simulations using head mounted displays (HMD) are becoming more available.
...computer-based simulations such as virtual and augmented reality simulations using head mounted displays are becoming more available.
This article will discuss the use of these new forms of technology mediated simulations. A brief overview of the technology will be presented, along with educational frameworks that have been used with virtual education, exemplars from the authors’ own work, and a brief review of selected scholarly literature. The scope of this article does not include a comprehensive review of the literature but rather highlights key information to introduce readers to the use of virtual reality as one form of technology-mediated learning.
Working Definitions
There are several definitions to describe many of the newer technology-mediated simulations so we begin with definitions that will be used throughout our discussion. These definitions are based on the published literature and current standards. The most up-date listing for definitions in this area is the XR Safety Initiative Taxonomy (XRSI, 2019-23). This is a living document that is regularly updated as needed. Currently there are no standard set of definitions or taxonomy, although the Simulation in Healthcare Simulation Dictionary has also been adopted by many to use and provides a good set of definitions (Lioce et al., 2020)
Important key terms include extended reality (XR), virtual reality (VR), augmented reality (AR), mixed-reality (MR) and the meta-verse. One distinction of the term virtual reality is important to consider. According to Shorey and Ng (2021), there are two variations of virtual worlds: desk virtual reality simulation (dVRS) and immersive virtual reality simulation (iVRS). A dVRS, also known as non-IVRS (non-immersive), is when learners interact with an environment displayed on a computer. In contrast, the iVRS is a completely immersive, simulated environment that requires a head mounted display (HMD). Immersive virtual reality (iVRS) provides 360 degrees of viewing and allows tracking of user movements and interactions. It also mimics reality more closely as the user can see all around the environment (Shorey & Ng, 2021).
...there are two variations of virtual worlds: desk virtual reality simulation and immersive virtual reality simulation.
The Table below further defines key terms used in this article. We will use the terms Immersive Virtual Reality (iVR) and Desktop Virtual Reality (dVR) to distinguish between VR that is viewed through a headset or head mounted display (HMD) and VR that is viewed on a computer screen.
Table. XR Definitions
|
XR Modality |
Definition |
|
Extended Reality (XR) |
XR does not refer to any specific technology; instead it is a way to group the realities. XRSI defines XR as a fusion of all the realities, which are “… technology-mediated experiences enable via a wide spectrum of hardware and software, including sensory interfaces, applications, and infrastructure.” XR is immersive and interactive (XRSI, 2019-23, para. 2). |
|
Screen Based Simulation |
A simulation presented on a computer screen like a computer game where users interact with the simulation using a keyboard/mouse or joystick/controller (Lioce, 2021). |
|
Virtual Reality |
A fully immersive, digital environment which is artificially created using software. Users engage in VR through an HMD or other specialized equipment. Virtual reality is immersive because the user is fully integrated into the experience and does not experience the outside world (XRSI, 2019-23). |
|
360 Video |
An immersive video format where the video is often recorded using a 360-degree camera that captures the view in all directions. The scene is experienced through a fixed point and can be viewed on a computer or via an HMD (XRSI, 2019-23). |
|
Augmented Reality |
AR overlays digital content into the user’s real world through a tablet or smart phone. The user is still present in the real world yet can visualize virtual or digital objects (XRSI, 2019-23). |
|
Mixed Reality |
MR blends the user’s world with digital content in such a way that the environments can interact with each other. In MR, virtual objects behave as if they are in the real world. (XRSI, 2019-23). |
|
Haptics |
Haptics is a mechanism or technology used for tactile feedback during the XR experience. This can include vibration, touch, or force feedback. (XRSI, 2019-23). |
|
Desktop Virtual Reality |
Learners interact with an environment displayed on a computer using mouse, keyboard, and touchpad (Shorey & Ng, 2021). |
Currently the use of XR and other technology mediated simulations is in the early stages and guidelines and protocols are still being developed. However, much of what we have used in other forms of simulation can be adapted and implemented.
Review of Selected Literature
Medical Education
The medical community has shown a greater affinity for iVRS. Proctor and Campbell-Wynn (2014) assessed the effectiveness, usability, and acceptability of manikins and haptic-enabled VR simulators when performing surgical cricothyroidotomy and found the VR simulator effective. The system met user acceptance (95%) and technology acceptance (85%). Wilson et al. (2020) evaluated the effectiveness of high-fidelity virtual reality and physical model simulation for teaching undergraduate medicine orthopedic concepts and found among the VR group that 64 participants improved their post-training scores (p<.00001). In 2020, Zackoff et al. found exposure to an immersive virtual reality curriculum on pediatric respiratory distress improved medical students’ recognition of impending respiratory failure (p=0.0004). Albufaraj et al. (2021) compared the efficacy of VR to manikin-based simulation to manage status epilepticus and found no statistical difference. Kotwal et al. (2021) hypothesized that novice clinicians could achieve proficiency in diagnosing dizziness by training with virtual patients.
The impetus to use virtual patients was the opportunity to introduce learners to deliberate practice to fine-tune diagnostic acumen.
The impetus to use virtual patients was the opportunity to introduce learners to deliberate practice to fine-tune diagnostic acumen. Participants used a virtual interactive case. Findings suggest that after 9 hours of virtual patient training there was a substantial increase in the diagnostic accuracy of interns.
Jaskiewicz et al. (2020) assessed chest compression quality performed in VR and found no statistical significance when compared to traditional chest compression training, suggesting that VR training is a viable option. Learners rated the VR training as superior to traditional training. Kononowicz et al. (2019) completed a systematic review and meta-analysis of virtual patient use in health professions education (n = 51). Outcomes of interest were knowledge, skills, attitudes, and satisfaction. Findings include mixed evidence that when compared with traditional education, use of virtual patients can more effectively improve skills and at least effectively improve knowledge.
Learners rated the VR training as superior to traditional training.
With regards to dVRS, Dubovi (2018) explored the impact of learning with online computer-based simulations on student clinical reasoning. The study investigated the Simple-to-Complex and Productive Failure approach to instructional design. Simple to complex design contains learning tasks in the learner’s zone of proximal development. Productive failure proposes beginning the learning process with complex challenges that are beyond the learner's abilities. Student achievement after learning with well-designed simple-to-complex computer-based simulations was higher than with traditional lecture-based instruction (p<.001).
Nursing Education
Nurse educators have been slower to adopt iVRS. Choi et al. (2022) completed a systematic review of immersive virtual reality in nursing education (n = 9) and found the iVRS is a viable technology for nursing students. Similar to recent findings, iVRS has a positive effect on cognition and learning performance. Barriers to iVRS, which are less frequently discussed, included left-handed players struggling with the controllers, prescription glasses fitting with the HMD, simulator sickness, and discomfort (Choi et al., 2022).
Nurse educators have been slower to adopt iVRS.
Chang & Lai (2020) explored the experience of nursing students learning to place nasogastric tubes using an immersive environment. Approximately 60 nursing students were interviewed; researchers found that learners describe the iVRS experience as convenient to practice, stress-free, and environmentally friendly, but required adaptation. The researchers suggested that, moving forward, iVRS can be seen as a student self-learning support tool.
Screen-based virtual simulations are gaining popularity. These options are typically commercially available, off-the-shelf solutions used to enhance the traditional simulation curriculum or to prepare learners for the clinical space. Foronda et al. (2020) completed a systematic review spanning 1996-2017 on the use of virtual simulation in nursing education. The focus of the review was to identify how virtual simulations impact learning outcomes among nursing students. Most of the learning outcomes were in the cognitive domain. Findings highlighted that when VR was compared to traditional manikin-based simulation, the learning outcomes were similar.
...when VR was compared to traditional manikin-based simulation, the learning outcomes were similar.
Verkuyl et al. (2017) explored virtual gaming simulation with a focus group and found that virtual simulation gaming can provide an experiential learning platform that promotes engagement and allows learners to acquire new knowledge while practicing in a safe environment. Tolarba (2021) completed a systematic review of virtual simulation in nursing (n =3) and found overwhelming evidence to support the positive impact on student learning, including theoretical knowledge and affective learning outcomes. Shorey and Ng (2021) completed a systematic review on the use of virtual simulation among nursing students and registered nurses (n = 18). Some advantages of virtual simulation that they found included higher time-cost-effectiveness as compared to mannikin-based simulation and classroom didactic.
Findings described by Shorey and Ng (2021) were similar to those of Tolarba (2021). Learning outcomes amenable to virtual reality include theoretical knowledge and cognitive outcomes. Both systematic reviews highlighted that there were no significant differences when using dVR on skills-based outcomes; however, among cognitive outcomes, there were significant improvements in theoretical knowledge such as medication administration, aseptic technique, managing respiratory distress, and administering a blood transfusion. In both reviews anxiety was higher in students who used screen-based or dVR, suggesting a challenge when using new technology.
Learning outcomes amenable to virtual reality include theoretical knowledge and cognitive outcomes.
Resoundingly, students appreciated the anytime, anywhere approach to learning. Dang et al. (2018) compared the three learning modalities active participation, VR observation, and television observation among nursing students and found a greater presence among the VR participants when compared to the television modality. Lastly, Haerling (2018) found that screen-based virtual simulation was a cost-effective solution when compared to manikin-based simulation. The virtual simulation activity had a cost utility ratio of U.S. $1.08 versus manikin-based simulation U.S. $3.62.
Resoundingly, students appreciated the anytime, anywhere approach to learning.
In summary, both immersive and desk virtual reality provide an experiential learning platform that has demonstrated gains in knowledge acquisition and affective learning outcomes. Furthermore, well-designed online simulations can provide authentic learning that improves clinical learning. While not exhaustive, this selected review of literature on VR supports the assertion that education outcomes using these virtual technologies add to, or at the minimum compared to, those of traditional manikins-based simulation.
Education Frameworks for Simulation
...well-designed online simulations can provide authentic learning that improves clinical learning.
Deliberate Practice
Simulation pedagogy is underpinned by several popular education and learning theories. Among them is deliberate practice, which is defined as deliberate effort to become an expert (Ericsson, 2008). This framework posits practice with immediate feedback and that the opportunity to redo improves competence and is recommended as an appropriate framework for nursing education. Inherent in simulation-based experiences is the opportunity to restart and perform again, incorporating feedback with the goal of greater knowledge acquisition and confidence in a psychologically safe environment.
Virtual simulation is a safe and effective way to achieve mastery level learning. Proponents of dVR recommend asynchronous opportunities free from pressure to perform. Learners are engaged in an active environment. Mabry et al. (2020) found that the use of virtual simulation in advance of manikin-based simulation increased learner self-efficacy. The premise behind the study included the ability to repeat the virtual simulation as many times as needed to ensure a particular score; deliberate practice allowed for mastery that prepared learners for the in-person traditional manikin-based simulation. The precursor of deliberate practice is mastery learning, which posits that a learner must achieve a defined proficiency in a given instructional unit before proceeding to the next unit. The focus is on the role of feedback (Siddaiah-Subramanya et al., 2017). Abdulonour et al. (2022) developed a screen based virtual simulation application based on the principles of deliberate practice to aid medical students in clinical reasoning. The application offers students this detailed feedback to support mastery in learning.
Virtual simulation is a safe and effective way to achieve mastery level learning.
Zone of Proximal Development
Another framework applicable in virtual simulation is Vygotsky’s (1978) Zone of Proximal Development (ZPD). The ZPD suggests that learning is developmental and constitutes two zones: current knowledge and proximal or potential knowledge. The proximal zone is an extension of the actual zone. It is the space between what learners can do independently and what they have the potential to do. The goal is to keep learning outcomes in the ZPD; breaching the zone can result in increased cognitive load and frustration on the part of the learner. As learners move across the zones, it expands to accommodate new knowledge.
Many screen-based simulations use artificial intelligence with adaptive guidance to ensure that learners remain in the ZPD. Learning with ZPD must provide a personalized challenge. Virtual escape rooms are an example where the learner is presented with a task which represents a particular concept or skill. To progress further, learners must discover and interact with the items referenced in the list, which contain further information on the concepts. The experience must be sufficiently difficult with the appropriate amount of cognitive load. Adaptive technology ensures the correct ZPD leads to cognitive interest and higher engagement (Ferguson et al., 2022)
Many screen-based simulations use artificial intelligence with adaptive guidance to ensure that learners remain in the ZPD.
Experiential Learning
Experiential learning has been used extensively in healthcare simulation and aligns well with technology mediated simulations. Kolb (1984) stated, “learning is the process whereby knowledge is created through the transformation of experience” (p. 38). This theory has four stages which are cyclical: concrete experience, reflective observation, abstract conceptualization, and active experimentation. Experiential learning theory is very appropriate for situations where the learner can explore and experiment and then cognitively process those experiences. This learning theory works well for virtual reality whereby the learner is immersed in an environment that features a problem-solving situation (Radianti et al, 2020). For nursing students, an example might be a patient who is experiencing some respiratory deterioration and the nurse needs to assess and implement interventions.
CBL has emerged as an important concept...
Competency-Based Learning
Another learning theory is competency-based learning (CBL). CBL has emerged as an important concept as nurse educators seek to measure behavioral competency and not just knowledge acquisition. The term CBL dates back to the 1920s and is a pedagogical approach that considers the mastery of measurable student outcomes (Henri et al, 2018). Students’ progress from basic to more advanced competencies. This theory can be applied to the use of virtual patients in XR. For example, nursing students might progress from learning how to ask basic questions of patients to conducting more complex patient interviews (Berman et al., 2016).
Virtual Reality Exemplars
Screen-based simulation provides learners with engaging, authentic encounters that have demonstrated knowledge transferability
Screen-based or dVR has seen an explosion in the post-pandemic period. The opportunity to provide learners with an alternative to face-to-face classroom instruction or in-lab high-fidelity simulation has freed resources and eliminated space constraints. Screen-based simulation provides learners with engaging, authentic encounters that have demonstrated knowledge transferability (Foronda et al., 2020). Users can practice in a safe environment, receive immediate feedback, and “level up” once they master certain learning outcomes. Numerous commercially available software options can be deployed with a web browser, with minimal technical requirements (see Figure 1). Learning can occur anytime and anywhere. The value of dVR is the ability to learn in either a synchronous or asynchronous environment.
Figure 1. Sentinel City© Screen Based VR

©Sentinel U (Used with permission)
Gonzalez et al. (2020) developed an augmented virtual reality neurological assessment trainer (see Figure 2). The technology was used as an overlay on a high-fidelity manikin. The enhanced imagery and dynamic facial features add value when performing a neurological assessment. The dimensionality of the AR experience allowed learners to notice the nasolabial flattening and facial drooping indicative of a stroke. The use of AR conferred a greater sense of urgency when assessing the patient for stroke-like findings. The details in this example of augmented VR highlight the limitations of static high-fidelity manikins to depict certain conditions.
Figure 2. Virtual Patient

©Salam Daher (Used with permission)
Butt et al. (2018) investigated the use of virtual reality haptic technology for psychomotor skill acquisitions. The skill under investigation was urinary catheterization. The study outcomes included time on task and the number of procedures completed within a prescribed amount of time. They found that students in the intervention cohort spent more time practicing. Findings suggested game-based VR may be an effective way to promote mastery learning (Butt et al., 2018).
...students in the intervention cohort spent more time practicing.
Aebersold and colleagues (2023) have developed 360-degree video to support caring for military veterans. This series of nine videos highlights unique care needs of this population and demonstrates effective ways of interacting to provide assistance and support. Three videos were created to establish foundational learning objectives around establishing rapport, asking appropriate questions, and establishing a dialogue around the veteran’s unique experience (see Figure 3). The videos can be accessed online without charge (Aebersold, 2023).
Figure 3. 360-Degree Video Recording for Caring for Our Veterans
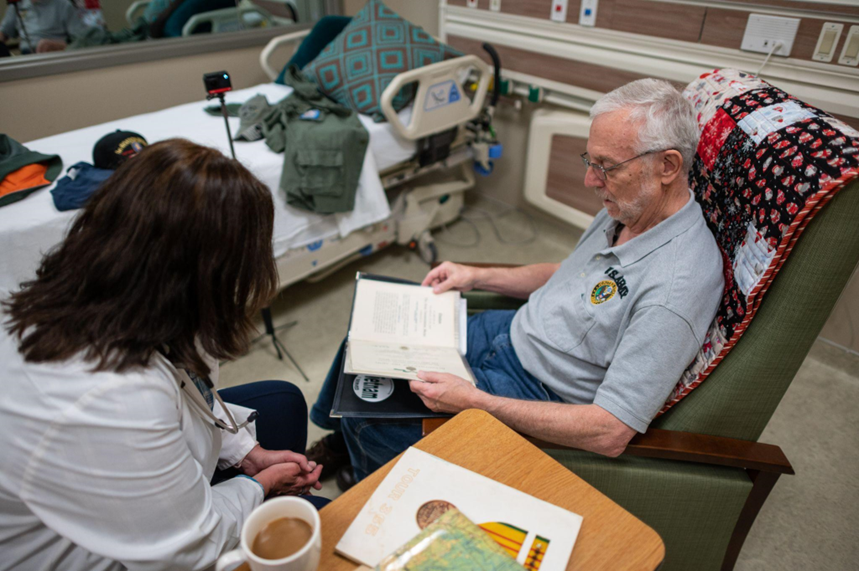
©University of Michigan School of Nursing (Used with permission)
Immersive VR and screen-based VR are widely used in nursing education. Aebersold and colleagues (2023) developed a VR simulation focused on improving the understanding of oncology emergencies. In this VR simulation, called Under the Skin, learners are introduced to two patients who are receiving a type of chemotherapy that can cause serious injury if the drug extravasates (see Figure 4). The VR program was developed as part of our work to improve cancer drug safety (Aebersold et al., 2021). The simulation focused on providing learners with an opportunity to practice donning personal protective equipment (PPE) and responding to an extravasation event. In addition, learners were able to go inside the human body to see the effects of the drug at the cellular level as it invades the cells and destroys them. The goal was to provide learners with a sense of how quickly an extravasation needs to be treated to prevent tissue destruction.
Figure 4. Under the Skin

©Michelle Aebersold (Used with permission)
Implementation of VR Technologies
The use of VR technologies poses some barriers to implementation that may not always be recognized in advance. As with all new technologies to facilitate learning it is important to consider best practices for implementation in support of students and faculty. A strong relationship with the information technology (IT) department can provide support and assistance to identify potential barriers such as connectivity, security, data management, and accessibility. Most technology mediated learning uses commercial devices and programs where data may be hosted outside of the school system.
Most technology mediated learning uses commercial devices and programs where data may be hosted outside of the school system.
In addition to technological needs, it is important to address faculty development. While simulation using technology mediated methods is similar to manikin-based simulation, there are some unique differences which we will outline below.
Infrastructure Requirements
The required support for dVR and iVR technologies will look different. Desktop VR generally requires a traditional computer and mouse, or a smartphone or tablet, for learners to engage with the scenario. Support needed for both faculty and students is generally similar to other forms of desktop IT support. This includes troubleshooting web browser compatibility, accessing the virtual scenario, and navigating the program.
The required support for dVR and iVR technologies will look different.
Support for iVR technologies is different. Traditional desktop IT support staff may be unfamiliar with the equipment that is used. There are a variety of HMDs available, and they do not all run on the same software. Accessing and engaging with scenarios in iVR is a different experience. For example, privacy, security, and safety issues are different from dVR. Each HMD has sensors built into the headset which collect information from the user, such as body movement and eye gaze. These data are used to support engagement with the scenario. Understanding what data are collected by the headset and the virtual learning program is important to ensure that only the minimum amount of necessary data are collected. The XR Safety Initiative (2019-2023) has identified a set of standards that can assist faculty to understand these privacy concerns and mitigate concerns. The XRSI Privacy and Safety Framework and resources are freely online (XRSI, 2019-2023).
When users are wearing the HMD for iVR they are immersed in the experience and do not ‘see’ the outside world. This can create safety issues if users are not careful about the physical environment they are in when engaging in iVR. When users are immersed in the activity, they often lose track of their surroundings and could trip or bump into things. CyberSickness is a real condition that can be caused by VR experiences. Learners may experience nausea, disorientation, headaches, and eye strain. “Cybersickness is introduced when there is abnormal visual-vestibular integration and vergence-accommodation” (Aebersold et al., 2023, p. 187). As technology improves, the incidence of cybersickness should decrease; however, some individuals may always be sensitive to this condition. Sitting during the iVR experience and taking breaks can help.
When users are wearing the HMD for iVR they are immersed in the experience and do not ‘see’ the outside world.
Faculty who are interested in using iVR will need support for management of the headsets. Actions required will include updates to firmware and software, access to internal wireless networks, installing applications, and general guidance about how to use headsets (Aebersold et al., 2023). Use of headset management software can support large numbers of headsets and student users.
Faculty Development
Historically, nursing faculty vary in response to change. Some faculty prefer ‘the way we have always done it.’ This mentality is in part responsible for the slow adoption of innovative technologies. From the inception of manikin-based simulation, there have been those who do not see the benefit and have resisted this technology. Fast forward to 2023 after experiences in the recent coronavirus pandemic: simulation labs and manikins are a feature of most nursing programs.
Given the rapid evolution of options, once again we are asking nursing faculty to consider another technology – one that removes the faculty member from the center of the conversation as we allow learners to engage in an alternative or asynchronous format. Nasrabadi et al., (2022) found that faculty need to develop the capacity and related competencies as stakeholders in employing these technological approaches. Furthermore, faculty need to be open to new ideas, committed to change, and capable of communicating with students (Nasrabadi et al., 2022). Similarly, Schuelke et al. (2022) found that faculty have concerns regarding change and unfamiliarity with the process. They recommend addressing faculty resistance early in the process to allay concerns prior to implementation.
...faculty need to develop the capacity and related competencies as stakeholders in employing these technological approaches.
In addition to faculty buy-in to incorporate use of technology mediated nursing education, it is important for them to understand the implementation needs unique to advanced technology. This is especially true if students are learning asynchronously or outside of the traditional simulation center. In particular, faculty need education about the use of headsets, pre-briefing, and debriefing. Verkuyl and colleagues (2018) have published recommendations on debriefing methods and Luctkar-Flude et al. (2021) has published a systematic review of virtual simulation methods. Findings from this research work have indicated that various options for students provide benefit and that debriefing experience is at important.
In particular, faculty need education about the use of headsets, pre-briefing, and debriefing.
Discussion
We have seen an increase in the adoption of VR technology, dVR to a greater extent than iVR. The research is still nascent but early work suggests that VR is comparable, if not better, for theoretical knowledge gain (Foronda et al., 2020; Shorey & Ng, 2020; Tolarba, 2021). Unfortunately, the research to date is heterogenous and in many cases underpowered, with questionable rigor. It remains a challenge to make assumptions that can be generalized to the population under review.
There is reason to be cautiously optimistic. When contemplating implementation of XR, especially iVR and dVR, into curriculum, educators should specifically consider learning outcomes and how these technologies can address learning outcomes or competency based learning. With this in mind, faculty should intentionally ask, is it the best approach? Often a VR method is a great option and can be implemented at a lower cost or with fewer resources. With all methods it is important to consider learning objectives, the level of the learner, and faculty expertise when designing a simulation experience, including those that use VR. Best practice guidelines, such as the International Nursing Association of Clinical and Simulation Learning (INACSL) Healthcare Simulation Standards of Best PracticeTM (INACSL Standards Committee, 2021) should be used to guide development and implementation.
Often a VR method is a great option and can be implemented at a lower cost or with fewer resources.
Recommendations for Practice
As we move toward a more technology mediated learning environment in nursing education in all settings (e.g., simulation laboratory, classroom, clinical, practice) it is important to review evidence-based implications for use of these resources. Key strategies include collaborating with others, experimenting with new options, and measuring effectiveness on learning outcomes. Some considerations may include timing, frequency of implementation, and commitment. Technology and innovative strategies should be introduced early and often. For learners to appreciate the value of these technologies, faculty must also be invested in these pedagogical methods.
Technology and innovative strategies should be introduced early and often.
When planning for dVR simulations, provide students with clear instructions about how to access the technology (e.g., passwords, software downloads). When introducing new iVR technology, plan for a comprehensive pre-brief with a minimum increase in the prebrief by 30 minutes to allow time for troubleshooting equipment if needed. If possible, students should come in advance of the simulation experience to familiarize themselves with the technology. Donning HMDs adds time to the experience as it is important to ensure that the headset is snug and instruct learners about how to adjust the lenses for best viewing. Always review safety precautions when students are in a headset to avoid injury as they are not able to ‘see’ their surrounding environment.
Adequate preparation will enhance the simulation experience for learners. Cybersickness can occur during an iVR experience; it is important to have alternatives available for students who cannot use HMDs. In general, it is helpful to have students begin in a seated position, keep the environment cool, and ensure that equipment is adjusted for each learner. Post experience, have a plan to sanitize equipment between users. Faculty should consider attaching a grade to the experience. Earning some points helps to ensure that learners are engaged and adds value to the simulation experience. Above all, set a goal to have fun with these new technologies.
Overall, technology mediated simulation experiences providing promising options for nursing education.
Overall, technology mediated simulation experiences providing promising options for nursing education. Faculty buy-in and planning are critical components for a good experience and strong outcomes. Collaboration with IT staff and others who have used the technology can also be helpful. Most importantly, many students embrace these new technologies and are eager to try them as they prepare for their nursing career.
Authors
Michelle Aebersold, PhD, RN, CHSE, FSSH, FAAN
Email: mabersol@umich.edu
ORCID ID: 0000-0001-8109-5643
Dr. Michelle Aebersold is a Clinical Professor at the University of Michigan School of Nursing, Certified Healthcare Simulation Educator, and a Fellow in the American Academy of Nursing and the Society for Simulation in Healthcare. Dr. Aebersold has extensive experience in using a variety of simulation learning methods to improve the care of patients through caregiver education and training. She is well published and presents on a variety of topics.
Laura Gonzalez, PhD, APRN, CNE, CHSE-A, ANEF, FAAN
Email: laura.gonzalez@sentinelu.com
ORCID ID: 0000-0002-1688-8142
Dr. Laura Gonzalez is the Vice President of Clinical Learning Resources at Sentinel U®. She is an internationally recognized simulation expert. She holds the prestigious certification of advanced certified healthcare simulation educators (CHSE-A). She is also a FAAN and ANEF. She is the current President of INACSL. Her focus is on advancing the science of nursing education using simulation and its impact on learner outcomes. She is well published and holds two patents.
References
Abdulnour, R., Parson, A.S., Muller, D., Drazen, J., Rubin, E. & Rencic, J. (2022). Deliberate practice at the virtual bedside to improve clinical reasoning. New England Journal of Medicine, 386. 1946-1947. https://www.nejm.org/doi/full/10.1056/NEJMe2204540
Aebersold, M. (2023). Carried for military veterans. University of Michigan Nursing in XR (NIXR). https://nixr.nursing.umich.edu/
Aebersold, M., Lee, D. & Nelson, J. (2023). Using augmented and immersive virtual reality in nursing education. In Jeffries, P. (Ed) Clinical simulations in nursing education: Advanced concepts, trends, and opportunities (2nd ed).
Aebersold, M. L., Kraft, S., Farris, L. B., Scherdt, M., Olsen, M., Polovich, M., Shelton, B. K., Montgomergy, G. H., & Friese, C. R. (2021). Evaluation of an interprofessional training program to improve cancer drug therapy safety. JCO Oncology Practice, 17(10), e155-1558. https://doi.org/10.1200/op.20.00816
Aebersold, M. (2016). The history of simulation and its impact on the future. AACN Advanced Critical Care, 27(1), 56-61. https://doi.org/10.4037/aacnacc2016436
Abulfaraj, M. M., Jeffers, J.M., Tackett, S., & Chang, T. (2021). Virtual reality vs. high-fidelity manikins-based simulation: A pilot randomized trial evaluating learner performance. Cureus 13(8).e17091. https//doi.org/10.7759/cureus.17091
Berman, N. B., Durning, S. J., Fischer, M. R., Huwendiek, S., & Triola, M. M. (2016). The role for virtual patients in the future of medical education. Academic Medicine, 91(9), 1217-1222. https://doi.org/10.1097/acm.0000000000001146
Butt, A., Kardong-Edgren, S., & Ellertson, A. (2018). Using game-based virtual reality with haptics for skill acquisition. Clinical Simulation in Nursing,16, 25-32, https://doi.org/10.1016/j.ecns.2017.09.010
Chang, Y. M. & Lai, C. L. (2021). Exploring the experiences of nursing students in using immersive virtual reality to learn nursing skills. Nurse Education Today, 97, 104670. https://doi.org/10.1016/j.nedt.2020.104670
Choi, J., Thompson, C., Choi, J., Waddill, C., & Choi, S. (2022), Effectiveness of immersive virtual reality in nursing education: Systematic review. Nurse Educator 47(3). E57-E61. https://doi.org/10.1097/nne.0000000000001117
Dang, B. K., Palicte, J. S., Valdez, A., & O'Leary-Kelley, C. (2018). Assessing simulation, virtual reality, and television modalities in clinical training. Clinical Simulation in Nursing, 19. 30-37. https://doi.org/10.1016/j.ecns.2018.03.001
Dubovi, I. (2018). Designing for online computer based clinical simulations: Evaluation of instructional approaches. Nurse Education Today, 69, 67-73. https://doi.org/10.1016/j.nedt.2018.07.001
Ericsson, K. A. (2008). Deliberate practice and the acquisition and maintenance of expert performance: A general overview. Academic Emergency Medicine, 15(11), 988-994. https://doi.org/10.1111/j.1553-2712.2008.00227.x
Ferguson, C., van den Broek, E. L., van Oostendorp, H. (2022) AI-Induced guidance: Preserving the optimal zone of proximal development. Computers and Education: Artificial Intelligence, 3, 100089. https://doi.org/10.1016/j.caeai.2022.100089
Foronda, C., Fernandez-Burgos, A., Nadeau, C., Kelley, C. N., Henry, M. N. (2020). Virtual simulation in nursing education: A systematic review spanning 1996-2018. Society for Simulation in Healthcare, 15(1), 46-54. https://doi.org/10.1097/SIH.0000000000000411
Gonzalez, L., Daher, S., & Welch, G. (2020). Neurological assessment using a physical-virtual patient (PVP). Simulation & Gaming, 51(6), 802-818. https://doi.org/10.1177/1046878120947462
Haerling, K. (2018). Cost utility of virtual and manikins based simulation. The Journal for the Society for Simulation in Healthcare, 13(1), 33-40. https://doi.org/10.1097/SIH.0000000000000280
Henri, M., Johnson, M. D., & Nepal, B. (2017). A review of competency‐based learning: Tools, assessments, and recommendations. Journal of Engineering Education, 106(4), 607-638. https://doi.org/10.1002/jee.20180
International Nursing Association of Clinical and Simulation Learning (INACSL) Standards Committee. (2021). Healthcare simulation standards of best practiceTM. Clinical Simulation in Nursing, 58, 66. https://doi.org/10.1016/j.ecns.2021.08.018
Jaskiewicz, F., Kowalewski, D., Starosta, K., Cierniak, M., & Timler, D. Chest compressions quality during sudden cardiac arrest scenario performed in virtual reality: A crossover study in a training environment. Medicine (Baltimore), 99(48), e23374. https://doi.org/10.1097/md.0000000000023374
Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development. Prentice Hall, NJ. http://www.learningfromexperience.com/images/uploads/process-of-experiential-learning.pdf
Kononowicz, A. A., Woodham, L. A., Edelbring, S., Stathakarou, N., Davies, D., Saxena, N., Car, L. T., Carlstedt-Duke, J., Car, J. & Zary, N. (2019). Virtual patient simulations in health professions education: A systematic review and meta-analysis by the digital health education collaboration. Journal of Medical Internet Research, 21(7), e14676. https://doi.org/10.2196/14676
Kotwal, S., Fanai, M., Fu, W., Wang, Z., Bery, A. K., Omron, R., Tevzadze, N., Gold, D., Garibaldi, B. T., Wright, S. M. & Newman-Toker, D. E. (2021). Real world virtual patient simulation to improve diagnostic performance through deliberate practice: A prospective quasi-experimental study. Diagnosis, 8(4), 489-496. https://doi.org/10.1515/dx-2020-0127
Lioce, L. Loprieto, J., Downing, D., Chang, T. P., Robertson, J. M., Anderson, M., Diaz, D. A., Spain, A. E., and the termnology and Concepts Working Group. (2020). Healthcare simulation dictionary (2nd ed.). AHRQ, Rockville, MD.
Luctkar-Flude, M., Tyerman, J., Verkuyl, M., Goldsworthy, S., Harder, N., Wilson-Keates, B., Kruizinga, J., & Gumapac, N. (2021). Effectiveness of debriefing methods for virtual simulation: A systematic review. Clinical Simulation in Nursing, 57, 18-30. https://doi.org/10.1016/j.ecns.2021.04.009
Mabry, J., Lee, E., Roberts, T., & Garrett, R. (2020) Virtual simulation to increase self-efficacy through deliberate practice. Nurse Educator 45(4),202-205. https://doi.org/10.1097/nne.0000000000000758
Nasrabadi, A. N., Mohammadi, N., Rooddehghan, Z., Shabani, E., Bakhshi, F., & Ghorban, A. (2021). The stakeholders’ perceptions of the requirements of implementing innovative educational approaches in nursing: A qualitative content analysis study. BMC Nursing, 20, 131. https://doi.org/10.1186/s12912-021-00647-7
Proctor, M. D., & Campbell-Wynn, L. (2014). Effectiveness, usability, and acceptability of haptic-enabled virtual reality and mannequin modality simulators for surgical cricothyroidotomy. Military Medicine, 179(3), 260-264. https://doi.org/10.7205/milmed-d-13-00365
Radianti, J., Majchrzak, T. A., Fromm, J., & Wohlgenannt, I. (2020). A systematic review of immersive virtual reality applications for higher education: Design elements, lessons learned, and research agenda. Computers & Education, 147, 103778. https://doi.org/10.1016/j.compedu.2019.103778
Schuelke, S. A., Davis, K., & Barnason, S. (2022). Implementing immersive virtual reality into a nursing curriculum. Innovations in Health Sciences Education Journal, 1(1). https://doi.org/https://doi.org/10.32873/unmc.dc.ihsej.0002
Shorey, S., & Ng, E. D. (2021). The use of virtual reality simulation among nursing students and registered nurses: A systematic review. Nurse Education Today, 98, 104662. https://doi.org/10.1016/j.nedt.2020.104662
Siddaiah-Subramanya, M., Smith S., & Lonie, J. (2017). Mastery learning: how is it helpful: An analytical review. Advanced Medical Education in Practice, 2(8), 269-275. https://doi.org/10.2147/AMEP.S131638
Tolarba, J. E. L. (2021). Virtual simulation in nursing education: A systematic review. International Journal of Nursing Education, 13(3), 48-54. https://doi.org/10.37506/ijone.v13i3.16310
Verkuyl, M., Romaniuk, D., Atack, L., & Mastrilli, P. (2017) Virtual gaming simulation for nursing education: An experiment. Clinical Simulation in Nursing, 13(5). 238-244. https://doi.org/10.1016/j.ecns.2017.02.004
Verkuyl, M., Lapum, J. L., Hughes, M., McCulloch, T., Liu, L., Mastrilli, P., Romaniuk, D., & Betts, L. (2018). Virtual gaming simulation: Exploring self-debriefing, virtual debriefing, and in-person debriefing. Clinical Simulation in Nursing, 20, 7-14. https://doi.org/10.1016/j.ecns.2018.04.006
Vygotsky, L. (1978). Mind in society: The development of higher psychological processes. Harvard University Press, Cambridge, MA.
Wilson, G., Zargaran, A., Kokotkin, I., Bhaskar, J., Zargaran, D., & Trompeter, A. (2020). Virtual reality and physical models in undergraduate orthopaedic education: A modified randomised crossover trial. Orthopedic Research and Reviews, 12, 97.
XR Safety Initiative (XRSI). (2019-2023) The XRSI privacy and safety framework. https://xrsi.org/publication/the-xrsi-privacy-framework
Zackoff, M. W., Real, F. J., Cruse, B., Davis, D., & Klein, M. (2019). Medical student perspectives on the use of immersive virtual reality for clinical assessment training. Academic Pediatrics, 19(7), 849-851. https://doi.org/10.1016/j.acap.2019.06.008


