Food allergies can significantly impact school-age children and the teachers and staff who interact with children. A nurse educator used materials from the Food Allergy Research & Education (FARE, 2019) to provide an educational intervention at a parochial urban school to help school staff and administrators become better prepared to manage students with food allergies. Academic training on allergy knowledge, attitudes, and beliefs was provided to non-medical staff at the school. The educational intervention impacted participants' knowledge and understanding of food-related policy development. As food allergies continue to rise in school-age children, coupled with the decrease in school nurses, the need for this type of intervention will expand. A nurse educator-led food allergy intervention could ensure informed staff caring for school children with allergies.
Key Words: nurse educators, nurse-led interventions, food, food allergies, school, school-age children, school nurses
Over the past decades, there has been a significant increase in food allergies in the United States population (Centers for Disease Control [CDC], 2016; Gupta et al., 2020). A specific characteristic of food allergies is that they are particularly prevalent in children and adolescents. Eighty-four percent of food-allergic children experience an allergic reaction in school (Behrmann, 2010). Approximately twenty-five percent of children with undiagnosed food allergies experience their first allergic reaction in school (Murphy, 2014). Effective food allergy management is always necessary in all situations. The pillars of food allergy management are prevention and emergency preparedness (Pistiner et al., 2015).
Over the past decades, there has been a significant increase in food allergies in the United States population
Guidelines have been published on preventative strategies for food allergen exposure and anaphylaxis. Behrmann (2010) notes that policies have been broken down into emergency action plans, templates for allergic students' medical information, and decreased risk of accidental ingestion. There is a need for guidelines to be in place for all those who work with children in a school setting because, as Pumphrey (2000) found when examining a series of 164 fatalities due to anaphylaxis, the median time interval between onset of symptoms and respiratory or cardiac arrest was 30 minutes in food-induced anaphylaxis. The proper assessment, prevention of exposure, and treatment are essential to save a life from accidental ingestion (Bedolla-Barajas et al, 2014).
In the past, prevention and response to food allergies have fallen upon school nurses. However, some limitations of the school nurse's response to anaphylaxis were present in the literature. Carlisle et al. (2010) noted there should be increased training requirements for registered nurses in response to anaphylaxis. Even with increased training, it was found that the school nurse's ability to prevent and respond was limited due to a ratio of one nurse to 650 students. Even with licensed personnel, a learning curve was present to respond appropriately (Carlisle, 2010; Pistiner, 2015). Other researchers found that even when school nurses were trained and competent in preventing and treating food allergies, only 53.6% of schools had a full-time nurse (Hogue et al., 2018; Triggiani et al., 2008).
These factors undermine guidelines by the American Academy of Allergy Asthma and Immunology, which recommends that all schools have a solid administration and prevention plan for each child diagnosed with an allergy and the ability to respond to anaphylaxis appropriately (LeBrovidge et al., 2015). Further research has noted multiple deficiencies in response to emergent planning and response to an allergic reaction (Carlisle et al., 2010).
Evidence-based food allergy policy and implementation gaps were found within schools with unique food allergy needs populations (Eldredge, 2014; Sicherer & Sampson, 2018). The allergy guidelines and policy were in place but lacked an emergency response plan. Most schools surveyed (90%) requested additional training, and 80% reported a registered nurse present only 10 hours weekly (Eldredge et al., 2014). These trends are concerning as children spend up to 50% of their waking hours attending school. There is a high risk of allergy exposure during school hours (Carlisle et al., 2010). Not all children at-risk for allergic reactions will have a registered nurse present during a reaction. Even then, Carlisle et al. (2010) found that self-reported proficiency among school nurses for critical areas of food allergy knowledge and management varied and found a weakness in staff education, delegation, developing guidelines for banning specific foods, and planning school trips. This is especially concerning as nurses are often absent on school and sports trips. Despite potential obstacles, the school environment can provide an opportunity to increase awareness, prevention, and treatment of food-allergic children outside the home (Illinois Dept of Ed, 2010; Sicherer & Sampson, 2018; Wang et al., 2017).
The opportunity to reinforce established training with the school personnel and staff will decrease anxiety, potentially reduce exposure, and improve response in an anaphylactic event.
Food allergy training is essential in schools with few or no school-based nurses, such as parochial schools. Many parochial schools do not employ full-time registered nurses. Thus, a trusted adult may or may not have extensive allergy training and policies related to allergy interventions. Guidelines exist to assist school administrators and personnel in developing local procedures to manage students with severe allergies. Benchmark training programs are available to help the public and private school systems (Wang et al., 2017). The Illinois Department of Education (2010) provides a detailed emergency action plan, but additional allergy awareness training is necessary for parochial schools. A pilot allergy awareness and training program could enhance and support the allergy response policy. The opportunity to reinforce established training with the school personnel and staff will decrease anxiety, potentially reduce exposure, and improve response in an anaphylactic event. Focused training could also facilitate adherence to CDC guidelines to ensure all schools can administer, prevent, and respond to emergency allergy plans (CDC, 2016). This article describes the impact of a nurse-led allergy awareness and training program for non-medical personnel on increasing knowledge, attitudes, beliefs, and support for an allergy response policy at a parochial school.
Methods
This study occurred at an inner-city parochial school serving 672 students with 79 known allergies. The location did not have a full or part-time school nurse on site, and even if there was a food allergy, administrators or other adults responded to the child. Previous training or certification in food allergies was not required, and no specific person was designated as the primary responsible adult. The educational intervention was delivered by qualified nurse educators using materials from the Food Allergy Research & Education (FARE) "Keeping Students Safe and Included" program (FARE, 2019). FARE is a free, nationwide, and validated online training course designed to help school staff and administrators better manage students with food allergies and respond to anaphylaxis appropriately (FARE, 2019). FARE measures and assists schools in implementing the CDC’s best practices for food allergies (FARE, 2019). This training course is encouraged and offered to the public and school systems upon inquiry.
Procedures
Due to the lack of a designated allergy-related person and school nurse on site, the educational interventions were made available and given to each faculty, staff, and volunteer adult who consented to participate in the study at the location. Participation was voluntary. Participating in the allergy education was free of charge and aligned with existing policies and programs (See Appendix A). The data retrieved from the surveys was encrypted and stored on a hard drive to which only the researchers had access. Due to the use of Survey Monkey, all responses recorded in the pre and post-test survey could be matched to each participant and remain anonymous to the researchers. The educational training for allergy knowledge, attitude, and beliefs was provided via one Zoom session (due to the Department of Public Health directives during COVID-19). The session was recorded and made available to individuals who could not attend the training. This study was approved by the Resurrection University IRB.
...the educational interventions were made available and given to each faculty, staff, and volunteer adult who consented to participate in the study at the location.
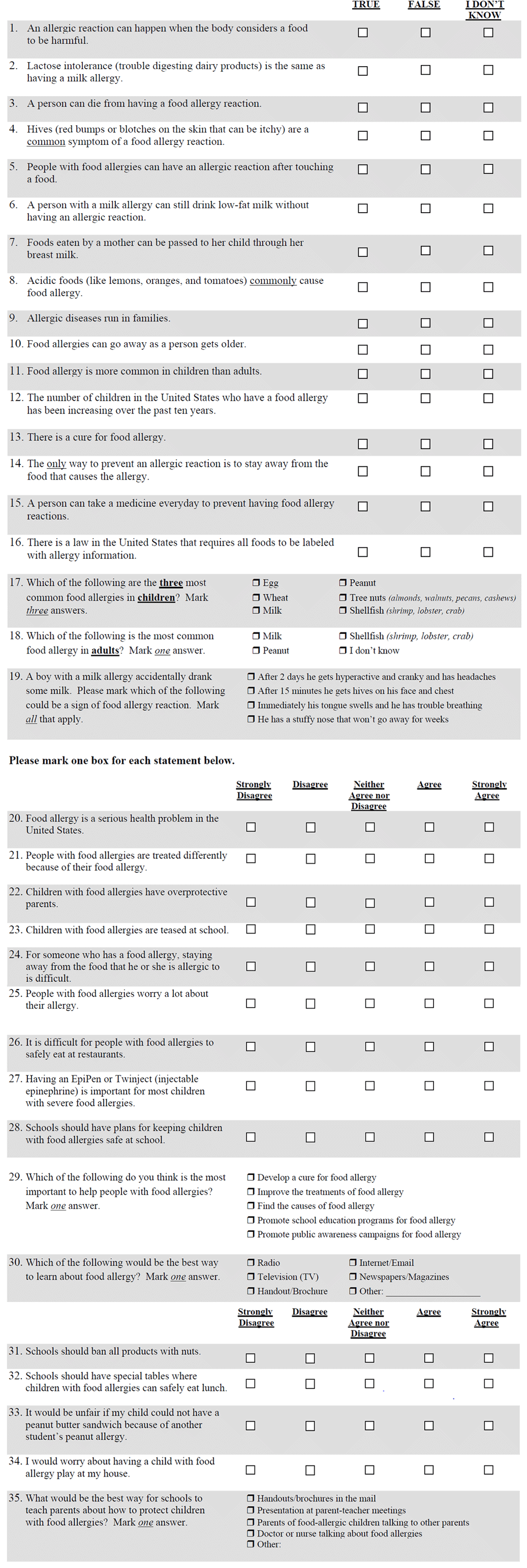
Survey Monkey was used to provide anonymity for online pre- and post-surveys. The participants had computer access at the parochial school if they did not have home access to complete the survey. In October 2020, before the intervention, a 35-question survey was sent via Survey Monkey to all faculty, staff, and volunteer adults at the location who consented to participate in the study (n=44). The survey included questions about knowledge (1-19), attitudes (20-30), and beliefs (31-35). The same survey was administered post-intervention to 44 participants in December 2020.
The pre- and post-survey results were analyzed using SPSS software. The analyses focused on the impact of the nurse-led educational anaphylaxis educational intervention on the non-medical personnel participants' overall knowledge, attitudes, and beliefs. After the intervention, the participants were expected to increase their knowledge level in each domain.
Results
A total of 44 participants consented to participate in the study and were sent the pre-intervention survey in October 2020. There was a 100% response rate with 44 responses, and no question was left blank. There was variation in the number of years taught. Half of the respondents taught K-4, with the remaining teaching 5-8 grades. Most participants (61%) had some previous training on allergy and allergy-related policies.
Most of the respondents in the pretest survey had a high general knowledge of food allergies. The overwhelming majority (95%) knew an allergy is when food harms the body. Eighty-four percent knew the difference between milk allergy and lactose intolerance. Ninety-seven percent knew someone could die from a food allergy. Everyone knew that someone could have an allergic reaction to just touching food. Just under 75% knew a person with a milk allergy could not have low-fat milk, and 88% knew food from mom could be passed via breast milk.
Respondents knew the top food allergies were peanuts, tree nuts, eggs, and milk but did not know about seafood. Respondents also stated that food allergies have increased (90%), there is no cure for food allergies (81%), and that food allergies do not go away with age (86%).
The respondents were less knowledgeable about specific beliefs concerning food allergies. About a quarter of respondents did not know if food allergies were hereditary, more common in children, if daily medication prevents an allergy, if staying away from allergic foods was difficult, or if children were treated differently or teased for having a food allergy.
The respondents did know specific policies and plans related to food allergies. The majority (81%) knew there were federal laws that required food labels, that those with food allergies should have epi-pens (79%), and that schools should have plans to address food allergies (77%). The policies to prevent exposure to potential food allergies were less supported as over half (65%) disagreed with banning nuts in schools, including not wanting to ban peanut butter sandwiches (43%). They did support having special tables that were nut, milk, and egg-free (85%).
The educational intervention also impacted participants' knowledge and policy despite the majority having some previous food allergy training. The difference was around knowledge about food allergies. The understanding of whether acidic food was a common allergy significantly changed (p = .03) from pre-not knowing (38%) and stating false (39%) to post-intervention, with only 3% not knowing and 60% stating false. Heritability was the second significant change (p = .04) in knowledge. Responses in the pretest had 24% not knowing, 46% stating true compared to the post-test stating true (53%).
Other significant changes were observed in responding to school policies and procedures regarding food allergies. The first significant finding (p = .01) regarded how to prevent food allergies with the policy that “people must stay away from the food that caused their allergies.” The pretest had 18% not knowing and 27% stating false. After the intervention, there were no known facts, and fewer reported false (4%), with the majority supporting the avoidance of food policy (59%). The last significant change (p =. 03) in terms of policy was whether schools should ban all nut products based on the potential of a child having a nut allergy. Once again, 6% strongly disagreed before the intervention, and 52% disagreed with this policy. Post-intervention, there was some change from the pretest strongly agreed (24%) to the post strongly agreed/agreed (60%).
Discussion
Food allergy awareness in schools remains a significant problem for students and those working there. This study found a significant impact on providing non-medical personnel with a nurse-led allergy awareness and training program. It increased knowledge and changed some attitudes, beliefs, policies, and support for allergy response policies. These changes enable what the CDC states in its best practices for volunteer school allergy practices: to ensure that schools can administer and respond to emergency allergy plans (CDC, 2016). Furthermore, these results help improve understanding of primary food allergies and develop school policies to respond to them appropriately. This could help address what Eldredge et al. (2014) found were gaps in evidence-based food allergy policies and implementation within schools with special needs populations.
The fact that the study participants were not nurses but adults working within the school setting also illustrates how this nurse-led educational intervention could be used within multiple school settings beyond the parochial system. This short, focused training for non-medical educators is needed as Eldredge et al. (2014) found that up to 80% of U.S. schools only had a registered nurse present 10 hours weekly.
The lack of a full-time or any registered nurse on-site with extensive food allergy training means that a non-medical person must know about allergies, policies, and policy compliance (Eldredge, et al. 2014; Wang et al., 2017), given a child’s elevated risk of allergy exposure during school hours compared to home (Carlisle et al., 2010). This short educational intervention by a nurse educator illustrated it could increase non-medical staff competency in food allergy knowledge and policies that assist with managing those allergies in the school setting. As Carlisle et al. (2010) and Wang et al. (2017) have shown, there is a need for this type of non-medical staff training to develop guidelines for identifying, isolating, or banning specific foods outside the school setting for sports and educational trips (Sicherer & Sampson, 2018; Triggiani et al., 2008). The study results showed that the school environment could provide and support a one-time nurse-led educational intervention, which provided an opportunity to increase awareness, prevention, and treatment of food-allergic children outside the home in a school setting without a full or part-time school nurse on-site. Results should be interpreted with caution, given its limitations. The study was a one-time, single-site educational intervention with one post-test analysis of its impact. A more extended series of interventions with multiple post-test results may offer differing results. A multiple-site study might produce different results, especially if it included schools with more or fewer students with food allergies.
A nurse educator-led food allergy intervention could help to ensure that children with allergies in school settings are safer with more informed staff.
Conclusion
A food allergy educational intervention by a nurse educator increased knowledge and understanding and supported food allergy policies for non-medical school personnel. As the increase in food allergies continues to be seen in school-age children, coupled with the decrease in school nurses, the need for this type of nurse-led intervention will expand. A nurse educator-led food allergy intervention could help to ensure that children with allergies in school settings are safer with more informed staff.
Appendix A. Survey Tool
Authors
La Vonne A. Downey, Ph.D.
Email: Ldowney@roosevelt.edu
Dr. La Vonne A. Downey is the Program Director and Professor of Health Sciences at Roosevelt University. Her research focuses on identifying and solving healthcare issues, the underserved, health policy, and global health. She teaches various classes, including Public Health, Medical Ethics, Health Economics, Health Policy, and Global Health. She is currently a member of several medical journal editorial boards and a reviewer for various medical and public health journals. She is also an advocate for ONE.org, UNICEF, and the UNA.
Mary C. Heinz, DNP, RN, CCM
Email: maryheinz6@gmail.com
Dr. Heinz is a Clinical Assistant Professor in the Department of Family and Community Health Nursing in the Marcella Niehoff School of Nursing at Loyola University Chicago. She has a child with food allergies and has actively educated parents and teachers about the issue.
Melissa Murphey, DNP, APRN-FPA, FNP-C
Email: murpheme@lewisu.edu
Dr. Melissa Murphey is the director of under graduate nursing at Lewis University in Chicago . She received her RN and DNP from the University of Illinois at Chicago. She is an NP who works for a retail pharmacy urgent care clinic and is a board member of the Illinois State Nursing Organization.
References
Bedolla-Barajas, M., Bedolla-Pulido, T. R., Camacho-Pena, A. S., Gonzalez-Garcia, E., & Morales-Romero, J. (2014). Food hypersensitivity in mexican adults at 18 to 50 years of age: A questionnaire survey. Allergy, Asthma & Immunology Research, 6(6), 511-516. https://doi.org/10.4168%2Faair.2014.6.6.511
Behrmann, J. (2010). Ethical principles as a guide in implementing policies for the management of food allergies in schools. The Journal of School Nursing, 26(3),183-193. https://doi.org/10.1177/1059840510364844
Carlisle, S., Vargas, P. A., Noone, S., Steele, P., Sicherer, S. H., Burks, A. W., & Jones, S. M. (2010). Food allergy education for school nurses: A needs assessment survey by the Consortium of Food Allergy Research. Journal of School Nursing, 26(5), 360-367. https://doi.org/10.1177/1059840510369482
Centers for Disease Control and Prevention.(2016). School Health Policies and Practices Study: Results from the School Health Policies and Practices Study. https://www.cdc.gov/healthyyouth/data/shpps/pdf/shpps-results_2020.pdf#page=20
Eldredge, C., Patterson, L., White, B., & Schellhase, K. (2014). Assessing the readiness of a school system to adopt food allergy management guidelines. Wisconsin Medical Journal, 113(4), 155-161. https://pubmed.ncbi.nlm.nih.gov/25211803/
Food Allergy Reseach & Education. (2019). Keeping students safe and included. FARE Training-Food Allergy Academy. https://www.foodallergy.org/our-initiatives/education-programs-training/fare-training-food-allergy-academy/keeping-students
Gupta, R. S., Bilaver, L. A., Johnson, J. L., Hu, J. W., Jiang, J., Bozen, A., Martin, J., Reese, J., Cooper, S. F., Davis, M. M., Togias, A., & Arbes, S. J. Jr. (2020) Assessment of pediatrician awareness and implementation of the addendum guidelines for the prevention of peanut allergy in the United States. JAMA Network Open, 3(7), e2010511. https://doi.org/10.1001/jamanetworkopen.2020.10511
Hogue, S. L., Muniz, R., Herrem, C., Silvia, S., & White, M. V. (2018). Barriers to the administration of epinephrine in schools. Journal of School Health, 88(5), 396-404. https://doi.org/10.1111/josh.12620
Illinois Department of Education and Illinois Department of Public Health (2010). Guidelines for managing life-threatening food allergies in Illinois schools. https://campussuite-storage.s3.amazonaws.com/prod/1559134/3a0e424a-fca4-11ec-93ce-0ec0e2f11e91/2453479/9ac82df4-1247-11ed-85c7-0ea4a7c4e2c3/file/ISBE%20Food%20Allergy%20Guidelines.pdf
LeBrovidge, J., Michaud, A., Deleon, A., Harada, L., Waserman, & Schneider, L. (2015). Evaluating a handbook for parents of children with food allergy: A randomized clinical trial. Annals of Allergy and Immunology, 116(3), 230-236.e1. https://doi.org/10.1016/j.anai.2016.01.001
Murphy, K. M. (2014). Emergency anaphylaxis at school. American Journal of Nursing, 114(9), 51-58. https://journals.lww.com/ajnonline/toc/2014/09000
Pistiner, M., Devore, C. D., & Schoessler, S. (2015). School food allergy and anaphylaxis management for the pediatrician- Extending the medical home with critical collaborations. Pediatric Clinical North America, 62(6), 1425-1439. https://doi.org/10.1016/j.pcl.2015.07.016
Pumphrey, R. S. (2000). Lessons for management of anaphylaxis from a study of fatal reactions. Clinical and Experimental Allergy: Journal of the British and Society for Allergy and Clinical Immunology, 30(8), 1144-1150. https://doi.org/10.1046/j.1365-2222.2000.00864.x
Sicherer, S., & Sampson, H. (2018). Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. Journal of Allergy and Clinical Immunology, 141(1), 41-58. https://doi.org/10.1016/j.jaci.2017.11.003
Triggiani,M., Patella, V., Staiano, R. I., Granata, F., & Marone, G. (2008). Allergy and the cardiovascular system. Clinical Experimental Immunology, 153(supp 1), 7-11. https://doi.org/10.1111%2Fj.1365-2249.2008.03714.x
Wang, J., Sicherer, S., SECTION ON ALLERGY AND IMMUNOLOGY, Matsui, E., Abramson, S., Dinakar, C., Irani, A-M., Kim, J. S., Mahr, T. A., & Pistiner, M. (2017). Guidance on completing a written allergy and anaphylaxis emergency plan. Pediatrics, 139(3), e20164005. https://doi.org/10.1542/peds.2016-4005


