We live in uncertain times. That uncertainty, however, gives nurses opportunities to use their powerful and strategic position to positively impact healthcare and society at large. One evidence-based means to make that impact is through policy advocacy. It is broadly accepted that nurses have a professional, ethical, and social responsibility to advocate. Yet, too often, they default on advocacy responsibilities within the policy arena. An original correlational research study, which investigated barriers and motivators toward policy advocacy for members of one state nursing organization, serves as an exemplar of how to systematically address this practice gap. Findings from this study demonstrated significant relationships and positive correlations between advocacy frequency and three variables: participant perceptions of speaking skills when addressing a policy maker; understanding the organizational daily advocacy activities; and understanding policy creation. This article reviews the research process, study results and discussion, and concludes with implications for applicable, practical recommendations for readers to move forward in advocacy.
Key Words: Nurse, advocacy, policy, change, practice gap, research, motivators, barriers
Despite the frequent call for nurses to advocate, there is evidence of a nursing practice gap in the policy arena.Despite the frequent call for nurses to advocate, there is evidence of a nursing practice gap in the policy arena. Advocacy, or the act of supporting or recommending action, is among the characteristics and responsibilities which define nurses. We live in an uncertain era when our nation’s healthcare system is undergoing tremendous changes. Also, the nursing profession continues to experience the challenges and growing pains necessary to take its rightful place among healthcare leaders. Thus, the impact and necessity of policy involvement by nurses, from the bedside to the international arena is increasingly apparent (Patton, Zalon, & Ludwig, 2019b); Robert Woods Johnson Foundation [RWJF], 2010, 2012). As members of America’s most trusted profession, and healthcare experts with a unique frontline perspective, registered nurses (RNs) have the potential to powerfully impact healthcare policy (Brenan, 2017; Kreitzer & Koithan, 2014).
Drivers and hindrances toward member advocacy participation needed study to determine where to act to close the gap.Yet, a practice gap in nurse policy advocacy has been demonstrated. This gap was noted by a national nursing organization’s state affiliate. The state nursing organization (SNO) leaders perceived its members’ lack of advocacy skills and commitment to engaging in advocacy. This was despite repeated and ongoing endeavors by leaders to motivate and empower members. Drivers and hindrances toward member advocacy participation needed study to determine where to act to close the gap (Spath & Kelly, 2017; Rosswurm & Larrabee, 1999). Therefore, when in January 2016 the aforementioned SNO leadership requested development of a policy advocacy toolkit (PAT), an evidence-based needs assessment survey was issued. We analyzed a group of RN participants who were members of the nursing organization in this Midwest state to determine motivators and barriers to policy advocacy. The results guided the organization through development of the PAT. That needs assessment and its analysis is the research focus of this article.
Research Process
Research Purpose Statement and Question
The purpose of this research was to clarify SNO members’ perceived motivators and barriers to policy advocacy. The research question was framed around the variables listed in the SNO’s May 2016 advocacy survey, and inquired as to a potential statistically significant relationship with participant advocacy frequency in the preceding 6 months. These variables included skills to address a policy maker (PM); understanding creation of political policy; SNL daily activities related to activism and advocacy; linkage of the nursing profession to political regulations; and power for any one person to influence a political issue. Working from Sudduth’s (2008) definition, a PM is one involved in creating authoritative, purposeful action plan(s) or guideline(s) toward specific goals. Although the term is often associated with government policy, it can to anyone in any policy making role.
Model and Framework
The framework guiding the overall project was Rosswurm and Larrabee’s (1999) model for change to evidence-based practice. Specific to the research and application discussed here are Rosswurm and Larrabees’ first three steps: 1) Assess the need for change in practice, 2) Link the problem to potential interventions and desired outcomes; 3) Synthesize evidence to develop a feasible solution.
Assessing the Need: Background and Local Context
The appropriateness of policy activism for nurses was established by Florence Nightingale.The appropriateness of policy activism for nurses was established by Florence Nightingale. Nightingale, though often remembered for her bedside care, dedicated a significant portion of her career to social and healthcare policy promotion (Selanders & Crane, 2012). Carrying that legacy forward, the SNO is among many healthcare and nursing associations, including the American Nurses Association (ANA), which promote nurse policy advocacy. Emphasizing its importance, the SNO lists policy advocacy in its vision and mission statements, and promotes it through education, publications, policy update alerts, toolkit type resources, and in leading by example (ANA, 2018). Yet, despite these efforts, leaders noted a continued practice gap among its members (SNO leader of membership advocacy, personal communication, January 8, 2016).
Assessing the Need: Literature Review
Many individuals have written about and encouraged nurses and nursing students to embrace their ethical responsibility toward nurse advocacy and leadership.The need to increase advocacy beyond this United States (U.S.) Midwest state is evidenced by national nursing and healthcare-related leaders and agencies’ consistent calls and actions to promote it. Many individuals have written about and encouraged nurses and nursing students to embrace their ethical responsibility toward nurse advocacy and leadership (Frey & Murphy, 2018; Khoury, Blizzard, Wright Moore, & Hassmiller, 2011; Patton, Zalon, & Ludwig, 2019a; Porter-O’Grady, Malloch, & Johnson, 2019).
Numerous nursing and healthcare organizations have also promoted advocacy, offering education, updates, and tools. The American Academy of Nursing (n.d.) emphasized nurse advocacy as imperative to achieve national healthcare goals. The ANA (2015) listed advocacy as an ethical obligation for all nurses to promote positive social change. Toward that end, ANA leadership and members lead by example as they represent RNs and nursing to the policy world; publish articles, texts, and news briefs regarding advocacy; maintain an advocacy toolkit; and declared 2018 the Year of Advocacy (ANA, n.d.; 2018). The American Academy of Nursing (n.d.) “serves the public and the nursing profession by advancing health policy and practice” (p. 1). The American Association of Colleges of Nursing (2006, 2008, 2011) promotes advocacy in professional nursing education, research, and practice and requires it be included in all baccalaureate and graduate nursing programs. The National League for Nursing (NLN; 2018), also promotes advocacy and provides a free, online public policy toolkit. A final example, and one outside nursing, is the Committee on the RWJF Initiative on the Future of Nursing, at the Institute of Medicine (Institute of Medicine of the National Academies, 2014). This group’s landmark work recommended that nurses practice to the full extent of their education and training (including policy advocacy) and that they be full partners in redesigning our healthcare system. The call for nurses to participate in policy advocacy is well established.
Study Design
A non-experimental, correlational research design, studying the relationship between variables, was employed to address the research question. The chi square test of independence determined statistically significant relationships between variables by comparing the observed variables’ frequency with their expected frequency. The assumption of minimum expected count for chi square was met.
Setting; Participants and Their Protection
The SNO is a Midwest statewide organization representing RNs. Among its foci are education, advocacy, and the advancement of nurses and the nursing profession. Invitees were comprised of all the SNO members who have given their email address to SNO headquarters. Participants were SNO members who chose to answer the SNO advocacy survey. There were 226 participants, 176 of whom offered complete, usable data.
This research was approved by the affiliated university institutional review board (IRB). The IRB was aware that the survey discussed in this article was previously generated by the SNO as part of their typical operations.
Procedures
A survey was created using information gleaned from a literature review and from field expert input. It consisted of 31 multiple choice questions and one question requiring preference ranking. Questions inquired about participant demographics and their perceptions regarding the appropriateness and effectiveness of nurse advocacy, motivators and barriers to personal advocacy involvement, personal advocacy skills, and preferred learning mode. The survey announcement, including the link to the questionnaire, was distributed to SNO members on May 16th, 2016 through a password secured email account. Invitees were told the survey would be available through May 31st, 2016 and were assured anonymity.
To encourage involvement, a single $40 Amazon gift card was raffled (Grove, Burns, & Gray, 2013). Participants wishing to take part in the drawing obtained access to the raffle by clicking a link within the survey which redirected them to a separate site. Survey results, displayed on a spreadsheet, were obtained by the SNO from the survey sponsor and forwarded to the researcher via email. Both the SNO’s and the researcher’s accounts were username and password protected.
Although not an established tool, the SNO survey was appropriately designed with input from literature findings and insights and advice from SNO experts regarding issues...Data were transferred to Statistical Package for the Social Sciences (SPSS), an analytical software tool (IBM, n.d.). The data were coded and respondents divided into subsections according to advocacy frequency (0-2, 3-5, 6 or more advocacy occurrences) within the preceding 6 months. The null hypotheses (H0) stated there was no relationship between each variable and the participant’s advocacy frequency in the preceding 6 months. The alternate hypotheses (Ha) stated a dependent relationship existed between each variable and the participant’s advocacy frequency in the preceding 6 months.
Reliability and validity
Although not an established tool, the SNO survey was appropriately designed with input from literature findings and insights and advice from SNO experts regarding issues such as survey question clarity, suitability, and readability; and survey length (Grove et al., 2013). DeVon et al. (2007), and later Grove et al. (2013, discussing DeVon et al.’s writing), noted that this input gives the tool face validity. Furthermore, subjects’ willingness to participate gives credence to a tool’s face validity because it suggests their perception that the tool measures that which they agreed to evaluate (Grove et al., 2013). The SNO leaders declined piloting the survey, stating it was not part of their normal operating procedures.
Results
A chi-square test of independence demonstrated a significant relationship between the following five variables and SNO survey participant’s advocacy frequency.
- Participant’s perception of speaking skills when addressing a PM (χ2 [4, n = 176] = 30.435, p < .001).
- Participant’s perceived understanding of how political policy is created (χ2 [4, n = 176] = 33.830, p < .001).
- Participant’s perceived understanding of the SNO’s daily activities as they relate to activism and advocacy (χ2 [4, n = 176] = 17.814, p =.001). Checking into that
- Participant’s perceived understating of how closely the nursing profession is linked to political regulations (χ2 [4, n = 176] = 11.219, p = .024).
- The participant’s perception of the extent to which any one person has the power to influence a political issue (χ2 [4, n = 176] = 12.611, p = .013).
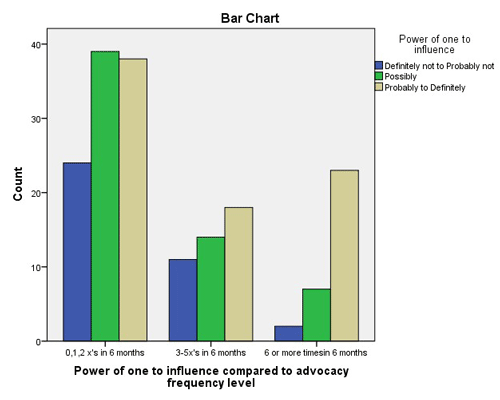
For these five variables, the null hypothesis was rejected. While chi-square tests and non-experimental designs do not demonstrate causation, positive correlations, or relationships, should be examined. The cluster-bar charts illustrate the study correlations. In the charts, participants were divided into three clusters according to their perception/understanding of the variable and another three reflecting the number of times he/she advocated in the previous six months. Each participant is represented in one of the nine columns within each bar chart. The bar charts in Figures 1, 2, and 3 demonstrate that the more a participant perceived he/she had skill or knowledge related to that given variable, the more often they advocated in the preceding 6 months.
The bar charts in Figures 4 and 5 show no relationship between participant perceived understanding or belief in those variables and how often he/she advocated in the previous six months. That is, although participants recognized the link between nursing and policy, and that even one person could affect a change (variables 4 and 5), that recognition was not associated with increased advocacy action. Thus, of the five significant variables, only variables 1, 2 and 3 (i.e., speaking skills when addressing a PM; political policy creation; and the SNO daily activities as they relate to activism and advocacy) were considered appropriate subjects for the PAT.
Figure 1. Speaking Skills
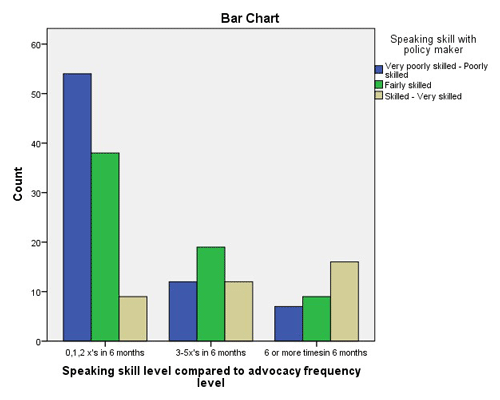
Figure 2. Understanding of Policy Creation
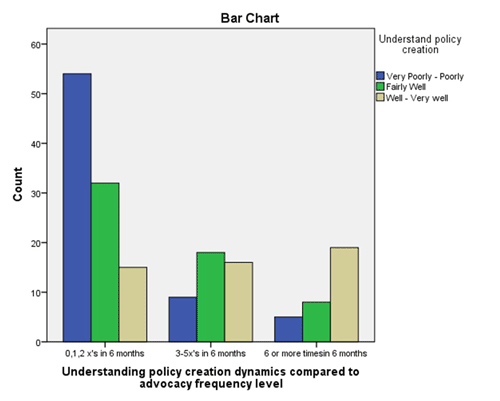
Figure 3. Understanding of SNO Daily Advocacy Activities
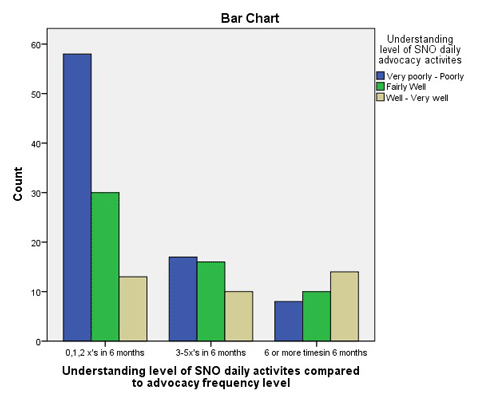
Figure 4. Link between Political Regulations and Nursing
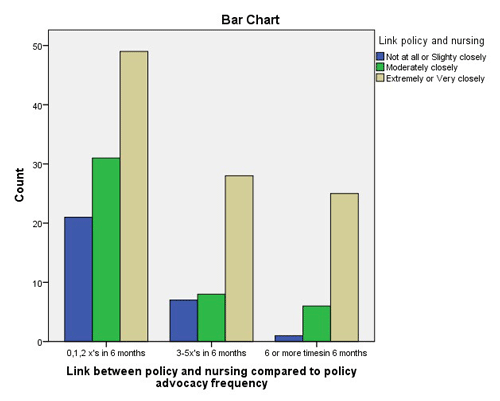
Figure 5. Perceived Perception of Power of One to Influence
Discussion
Applying Research Results to the SNO
The evidence generated in this study clarified three variables with a statistically significant relationship and positive correlation with SNO members’ policy advocacy frequency: speaking skills when addressing a PM; understanding political policy creation; and understanding the SNO daily activism and advocacy activities. The analysis confirms work from a number of previous authors and/or researchers.
The relationship between verbal communication skills and advocacy has been supported by Tomajan and Hatmaker (2019); and Verba, Schlozman, & Brady’s (1995) civic volunteerism model. The positive relationship between participant nurses’ perceived understanding of political policy creation and advocacy frequency is also supported by others’ work. Examples include Moreland-Russell, Zwald, & Golden (2016) and Vandenhouten, Malakar, Kubsch, Block, & Gallagher-Lepak (2011). As this relationship was confirmed for the SNO end-users, modules covering these subjects were included in the policy advocacy toolkit (Jurns, 2017).
Research results generated in this study suggest that there is value in taking the additional step to better inform members regarding the SNO daily advocacy activities.No other work found demonstrated, or referenced, a correlation between nurse understanding of nursing organization daily activism activities and individual nurse policy activity frequency. Like numerous other organizations, the SNO leadership promotes advocacy and goes to great lengths to educate and encourage members to this end. Research results generated in this study suggest that there is value in taking the additional step to better inform members regarding the SNO daily advocacy activities. This information was shared with SNO leadership, who were best equipped to create a means to inform members of the organization regarding this daily advocacy work.
Broader Application and Implications
The SNO May 2016 survey analysis results offer implications for the broader nursing community. Nurses can use this and other research to actively channel the need for change in a positive direction. This is especially true as we experience uncertainty on many fronts, such as social or political instability. This section will discuss application of the results of this study, and offer practical recommendations to move forward in advocacy.
Speaking with policy makers. Although nurses reported a perceived lack of speaking skills when addressing PMs, nurses are educated and trained to communicate. One of many means they effectively use to do so is through using the evidence-based (I)SBAR tool (Marshall, Harrison, & Flanagan, 2008). The author suggests that nurses use this already honed skill with confidence to address PMs. This is further discussed in the article, “Using SBAR to Communicate with Policy Makers” (Jurns, 2018). Additional practical, evidence-based strategies are detailed below in Table 1.
Table 1. Meeting Your Policy Maker
|
Making the Appointment |
|
|
Be succinct but not hurried |
Consider using (I)SBAR to synopsize and guide your core message. |
|
Person(s) |
Be flexible to meet with the PM or with a staff member. Do not discount a staff member’s influence. He/she Go alone or with others. Both are acceptable. |
|
Place |
Be open to meeting in-person or electronically at any mutually agreeable, safe, and legitimate place. |
|
Time |
Learn in advance how much time is allotted. Organize to be prepared to leave when the time is competed. |
|
Confirmation |
Send a clear follow-up appointment confirmation. |
|
Before the Meeting |
|
|
|
Clothing should be neat, clean, and setting appropriate. Read through the person’s biographical information to better understand and relate to them. Practice. It makes experts of novices. |
|
During the Meeting |
|
|
|
Give name cards if possible. Relax. Maintain a calm voice. Be conscious of body language. Be friendly yet professional. Acknowledge status. Be succinct but not hurried. Demonstrate empathy. Ask and invite questions. |
|
The Conversation |
|
|
General Tips |
Facts shared must be verifiable. Otherwise state as opinion, observation, or experience. If going with others, predetermine who will speak on what subtopics. Use understandable words/terms (avoiding professional jargon). If asked a question you cannot answer, do not guess or be intimidated. Acknowledge your uncertainty and commit to investigating the issue and responding as soon as possible. If representing an organization, only state its position. Personalize it. Know the PM’s views and concerns and share how he/she and his/her interest would advance/benefit. Tell a personal narrative/anecdote. A story can make the concern more real for the PM. |
|
Keeping the conversation focused |
If the PM speaks tangentially, or is talkative: Acknowledge his/her comments and then return the conversation back to the primary issue. (Example: “Yes, it is true that X is occurring in our hospital. That is a great example of why my suggested solution is timely.”) Ask direct questions during a pause. (Example: “That is an interesting point. Perhaps there is a connection between [the topic the PM just mentioned] and the issue which concerns me. Could we work together to support each other?” Listen carefully. If the PM is being talkative, try to determine why. What message is (s)he trying to communicate? If you can identify the message, you can build on it. (Example: “Yes, Mr. President, we appreciate your past support of X. That is why we are looking for your leadership in this [named] issue.”) Listen actively. Only interrupt if necessary, following the above strategies. |
|
Closing |
Be prepared to leave at the end of allotted time. Offer a clear recommendation. The recommendation must be feasible (politically, financially, within the policymaker’s authority, and within a workable timeframe). If representing an organization, state its recommendation. Leave a brief, bulleted fact sheet. Say thank you and discuss an appropriate time and means to follow-up. |
|
Afterward |
|
|
Follow-up Actions |
Send an immediate thank you and reiterate key points. If representing an organization, inform that group of the contact with PM. Follow up as per agreement. This is important as in the interim others are presenting possibly opposing views. Follow-up every 2-3 months with politicians. This allows time for the slow political progress to move forward and gives opportunity to build an ongoing relationship. |
Sources: Advocacy and Communication Solutions, 2015; ANA, 2018; American Public Health Association, 2018; Benner, 2001; Brownson, Royer, Ewing, and McBride, 2006; Jurns, 2017, 2018; Kingdon, 2003; Patton et al., 2019b; Teater, 2009; White and Dudley-Brown, 2012.
Understanding policy creation. This section contains information about both governmental policy and organizational policy. In addition, table 2 lists resources for policy creation.
Governmental policy. There are many ways to learn about how policy is created. One may consider courses on this subject to meet continuing education requirements. Following in Table 2 are a list of selected resources which primarily discuss governmental policy, using different means to communicate the information. It is noteworthy that, although there is some variation between the state and federal processes, there are many similarities; therefore, all offer valuable information.
Table 2. Selected Resources Explaining Policy Creation
|
Resource |
Offered information |
|
Cairney; Jurns |
Written (and audio) explanations of Kingdon’s (2003) research regarding how issues get on the political agenda. |
|
Georgia Public Broadcasting |
Animated discussion of the three branches of government and a bill |
|
The Ohio Legislature, 132nd General Assembly |
Schematic explanation of bill to law summary |
|
Lanier |
Author literally spells out the legislative process and how nurses can effectively be involved. |
|
NLN |
Public policy toolkit: A rich example of a nursing organization offering information and/or a toolkit on policy advocacy and related topics. |
|
World Health Organization |
Health service planning and policy making |
|
Joint Commission International |
Create effective policies (this includes available workshops) |
Sources: Cairney, 2013; Georgia Public Broadcasting, 2018; Joint Commission International [JCI], n.d.; Jurns (2017, see p. 121-128); Lanier, 2016; NLN, 2018; The Ohio Legislature, 132nd General Assembly, 2018; World Health Organization, Regional Office for the Western Pacific [WHO], 2005.
Nurses can learn about organizational policy in a variety of ways.Organizational policy. Nurses can learn about organizational policy in a variety of ways. Working on organizational boards or involvement in shared governance offers firsthand knowledge. Workshops and webinars are also available on the topic of policy and on the closely related topic of organizational theory. Readers are encouraged to search for what is available, interesting, and convenient. Understanding organizational systems, and the policies within them, empowers nurses as change agents.
This research offers evidence that understanding an organization’s daily advocacy activities is positively correlated with advocacy frequency. It is not known if this correlation can be generalized. Even if so, it would be impossible to cover this topic here as each organization is unique. Instead, it is suggested that organization’s members, leaders, and staff work proactively to cross this advocacy barrier.
The lesson learned is that each nurse and subgroup of nurses is unique and it is prudent to consider end-users unique needs when developing education or a program.Just as important as what was demonstrated to be significant for this one Midwestern state’s RNs is what was demonstrated to not be significant. That is, it is instructive to consider the results of this study do not completely align with those of other researchers. One reason for this is simply different participants involved in different studies. The lesson learned is that each nurse and subgroup of nurses is unique and it is prudent to consider end-users unique needs when developing education or a program (Billings & Halstead, 2016; Hodges & Videto, 2011). Additionally, if planning a program, nurses are encouraged to use a theoretical foundation for program support (McEwen, 2014). Several strong and practical examples are the Agency for Healthcare Research and Quality knowledge transfer framework (Nieva et al., 2005; see figure 1); and Kotter’s (1995), and Rosswurm & Larrabee’s (1999) work.
Limitations
One limitation of this study was the survey tool's validity and reliability. Although face validity and reliability are legitimate, they are the weakest forms of evidence (Grove et al., 2013). A tool with stronger validity and reliability would have strengthened the study. A second limitation was use of a convenience sample of RNs in one Midwest state, who chose to participate in the survey in June 2016. Studying a broader population of RNs, employing random sampling, and studying this phenomenon over time would strengthen future research.
While individual advocacy can occur at the bedside, nurses are encouraged to broaden their influence to include the policy realm.
Conclusion
The uncertainty of life calls on nurses to act on their privilege, right, and ethical responsibility to advocate to effect positive change. While individual advocacy can occur at the bedside, nurses are encouraged to broaden their influence to include the policy realm. To do this, nurses must be equipped to act as policy advocates. This research suggests that nurses are more likely to advocate if they have confident speaking skills when addressing a PM, they understand their organizations’ daily policy activity, and they know how policy is created. It is the responsibility of individual nurses, and nursing and healthcare organizations, to ensure that this knowledge and skill is attained. While this may be a formidable task, it is worthwhile as the issues with which nurses are professionally engaged are tremendous: the wellbeing of nurses and of all humanity.
Acknowledgment
The author would like to acknowledge Dr. Mattie Burton and Dr. Deb Arms for their consistent encouragement and practical advice during this research process, and Dr. Sarah Inkpen for her extensive assistance in the statistical analysis of the data.
Authors
Carolyn Jurns, DNP, MSN, RN
Email: cjurns@gmail.com
Carolyn Jurns DNP, MSN, RN has extensive experience related to nurse advocacy in state nursing organization and campaign manager capacities, as well as clinical experience in adult medical surgical critical care. Her doctoral research at Walden University in Minneapolis, Minnesota focused on understanding variables correlated with nurses’ advocacy frequency.
References
Advocacy and Communication Solutions. (2015). Key tips for meeting with policymakers. Retrieved from http://www.advocacyandcommunication.org/wp-content/themes/acs/docs/resources/policy_maker_engagement_December_2015/ACS_Key_Tips_Policymaker_Meeting_Tips_.pdf
AHRQ, Agency for Healthcare Research and Quality. (n.d.). Home page. http://www.ahrq.gov/
American Academy of Nursing. (n.d.). Policy and advocacy. Retrieved from http://www.aannet.org/home
American Association of Colleges of Nursing. (2006). The essentials of doctoral education for advanced nursing practice. Retrieved from American Association of Colleges of Nursing: https://www.aacnnursing.org/Portals/42/Publications/DNPEssentials.pdf
American Association of Colleges of Nursing. (2008). The essentials of baccalaureate education for professional nursing practice [Educational standards]. Retrieved from http://www.aacnnursing.org/portals/42/publications/baccessentials08.pdf
American Association of Colleges of Nursing. (2011). The essentials of master’s education in nursing [Educational standard]. Retrieved from http://www.aacnnursing.org/portals/42/publications/mastersessentials11.pdf
American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. Retrieved from https://www.nursingworld.org/coe-view-only
American Nurses Association. (2018). Year of advocacy [Press release]. Retrieved from http://ana.aristotle.com/SitePages/YearOfAdvocacy.aspx
American Nurses Association. (n.d.). ANA advocacy toolkit. Retrieved from https://www.nursingworld.org/practice-policy/advocacy/ana-advocacy-toolbox/
American Public Health Association. (2018). Tips for making a visit to your policy-maker. Retrieved from https://www.apha.org/-/media/files/pdf/advocacy/policymaker_visit_tips.ashx
Benner, P. (2001). From novice to expert: Excellence and power in clinical nursing practice (Commemorative ed.). Upper Saddle River, NJ: Prentice-Hall.
Billings, D. M., & Halstead, J. A. (2016). Teaching in nursing: A guide for faculty (5th ed.). St. Louis, MO: Saunders Elsevier.
Brenan, M. (2017). Nurses keep healthy lead as most honest, ethical profession. Retrieved from https://news.gallup.com/poll/224639/nurses-keep-healthy-lead-honest-ethical-profession.aspx
Brownson, R. C., Royer, C., Ewing, R., & McBride, T. D. (2006). Researchers and policy makers: Travelers in parallel universes. American Journal of Preventative Medicine, 30(2), 164-172. http://dx.doi.org/10.1016/j.amepre.2005.10.004
Cairney, Paul (Producer). (2013, October 31). Policy concepts in 1000 words: Multiple streams analysis. In Paul Cairney: Politics & public policy [Audio podcast]. Retrieved from https://paulcairney.wordpress.com/2013/10/31/policy-concepts-in-1000-words-multiple-streams-analysis/
DeVon, H. A., Block, M. E., Moyle-Wright, P., Ernst, D. M., Hayden, S. J., Lazzara, D. J., ... Kostas-Polston, E. (2007). A psychometric toolbox for testing validity and reliability. Journal of Nursing Scholarship, 39(2), 155-164. https://doi.org/10.1111/j.1547-5069.2007.00161.x
Frey, J. L., & Murphy, C. K. (2018). Healthcare policy and advocacy. In G. Roux & J. A. Halstead (Eds.), Issues and trends in nursing: Practice, policy, and leadership (2nd ed., pp. 393-424). Burlington, MA: Jones and Bartlet Learning.
Georgia Public Broadcasting, NPR. (2018). The legislative process [Web episode]. In Georgia Public Broadcasting, NPR (Producer), Georgia Stories. Retrieved from http://www.gpb.org/georgiastories
Grove, S. K., Burns, N., & Gray, J. R. (2013). The practice of nursing research: Appraisal, synthesis, and generation of evidence (7th ed.). St. Louis, MO: Elsevier, Saunders.
Hodges, B. C., & Videto, D. M. (2011). Assessment and planning in health programs (2nd ed.). Sudbury, MA: Jones & Bartlett Learning.
IBM (n.d.). IBM SPSS Software. Retrieved from https://www.ibm.com/analytics/spss-statistics-software.
Institute of Medicine of the National Academies. (2014). The future of nursing: Leading Change, Advancing Health. Retrieved from http://www.iom.edu/Reports/2010/The-Future-of-Nursing-Leading-Change-Advancing-Health.aspx
Joint Commission International. (n.d.). Create effective policies. Retrieved March 19, 2019, from https://www.jointcommissioninternational.org/improve/create-effective-policies/
Jurns, C. S. (2017). Promoting policy advocacy in nursing via education (Doctoral dissertation). Available from ProQuest Dissertations and Theses database. (UMI No. 10280307)
Jurns, C. S. (2018). Using SBAR to communicate with policymakers. Online Journal of Issues in Nursing, 24. doi: 10.3912/OJIN.Vol24No01PPT47
Khoury, C. M., Blizzard, R., Wright Moore, L., & Hassmiller, S. (2011). Nursing leadership from bedside to boardroom: A Gallup national survey of opinion leaders. JONA: Journal of Nursing Administration, 41(7/8), 299-305. http://dx.doi.org/10.1097/NNA.0b013e3182250a0d
Kingdon, J. W. (2003). Agendas, alternatives, and public politics (2nd ed.). New York, NY: Addison-Wesley Education Publishers.
Kotter, J. P. (1995). Leading change: Why transformation efforts fail. Harvard Business Review, 73, 59-67. Retrieved from https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2
Kreitzer, M. J., & Koithan, M. (2014). Integrative nursing. New York, NY: Oxford University Press.
Lanier, J. (2016). The ABCs of effective advocacy: Attention, bipartisanship, & collaboration. Ohio Nurses Review, 91(1), 16-25. Retrieved from https://www.bluetoad.com/publication/?i=288144&article_id=2376583
Marshall, S., Harrison, J., & Flanagan, B. (2008). The evaluation of structured communication tools in healthcare. Retrieved from Proceedings of the Human Factors and Ergonomics Society 52nd Annual Meeting-2008. doi: 10.1177/154193120805201221
McEwen, M. (2014). Overview of theory in nursing. In M. McEwen, & E. M. Wills (Eds.), Theoretical basis for nursing (4th ed., pp. 23-48). Philadelphia, PA: Wolters Kluwer / Lippincott Williams & Wilkins.
Moreland-Russell, S., Zwald, M., & Golden, S. D. (2016). Policy help needed, experience required: Preparing practitioners to effectively engage in policy. Health Promotion Practice, 17(5), 648-655. https://doi.org/10.1177/1524839916650433
National League for Nursing. (2018). Public policy toolkit. Retrieved from http://www.nln.org/professional-development-programs/teaching-resources/toolkits/advocacy-teaching/toolkit-home
Nieva, V. F., Murphy, R., Donaldson, N., Combes, J., Mitchel, P., Kovner, C., ... Carpenter, D. (2005). From science to service: A framework for the transfer of patient safety research into practice. In K. Henriksen, J. B. Battles, & E. S. Marks (Eds.), Advances in patient safety: From research to implementation (Volume 2: Concepts and methodology). Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK20521/
Patton, R. M., Zalon, M. L., & Ludwick, R. (2019a). Leading the way in policy. In R. M. Patton, M. L. Zalon, & R. Ludwick (Eds.), Nurses making policy: From bedside to boardroom (2nd ed., pp. 3-35). New York, NY: Springer.
Patton, R. M., Zalon, M. L., & Ludwick, R. (Eds.). (2019b). Nurses making policy: From bedside to boardroom (2nd ed.) New York, NY: Springer
Porter-O’Grady, T., Malloch, K., & Johnson, I. (2019). Changing organizations, institutions, and government. In R. M. Patton, M. L. Zalon, & R. Ludwick (Eds.), Nurses making policy: From bedside to boardroom (2nd ed., pp. 225-260). New York, NY: Springer.
Robert Woods Johnson Foundation. (2010). Groundbreaking new survey finds that diverse opinion leaders say nurses should have more influence on health systems and services. Retrieved from https://www.rwjf.org/en/library/articles-and-news/2010/01/groundbreaking-new-survey-finds-that-diverse-opinion-leaders-say.html
Robert Woods Johnson Foundation. (2012). Advocates call on nurses to take leading role in palliative care. Retrieved from https://www.rwjf.org/en/library/articles-and-news/2012/09/advocates-call-on-nurses-to-take-leading-role-in-palliative-care.html
Rosswurm, M. A., & Larrabee, J. H. (1999). A model for change to evidence-based practice. The Journal of Nursing Scholarship, 31(4), 317.
Selanders, L. C., & Crane, P. C. (2012). The voice of Florence Nightingale on advocacy. Online Journal of Issues in Nursing, 17(1). doi: 10.3912/OJIN.Vol17No01Man01
Spath, P. L., & Kelly, D. L. (2017). Applying quality management in healthcare: A systems approach (4th ed.). Chicago, IL: Health Administration Press.
Sudduth, A. L. (2008). Program evaluation. In J. A. Milsted (Ed.), Health policy and politics: A nurse’s guide (3rd ed., pp. 172-196). Sudbury, MA: Jones and Bartlett.
Teater, B. (2009). Influencing state legislators: A framework for developing effective social work interest groups. Journal of Policy Practice, 8(1), 69-86. http://dx.doi.org/10.1080/15588740802282540
The Ohio Legislature, 132nd General Assembly. (Cartographer). (2018). The legislative process [Schematic]. Retrieved from https://www.legislature.ohio.gov/publications/the-legislative-process
Tomajan, K., & Hatmaker, D. D. (2019). Advocating for nurses and for health. In R. M. Patton, M. L. Zalon, & R. Ludwick (Eds.), Nurses making policy: From bedside to boardroom (2nd ed., pp. 37-71). New York, NY: Springer.
Vandenhouten, C. L., Malakar, C. L., Kubsch, S., Block, D. E., & Gallagher-Lepak, S. (2011). Political participation of registered nurses. Policy, Politics, & Nursing Practice, 12(3), 159-167. http://dx.doi.org/10.1177/1527154411425189
Verba, S., Schlozman, K. L., & Brady, H. E. (1995). Voice and equality: Civic voluntarism in American politics. Cambridge, MA: Harvard University Press.
White, K. M., & Dudley-Brown, S. (2012). Translation of evidence into nursing and health care practice. New York, NY: Springer.
World Health Organization, Regional Office for the Western Pacific. (2005). Module 4: Policy-development process. In Health service planning and policy-making: A toolkit for nurses and midwives. Retrieved from http://www.wpro.who.int/publications/docs/hsp_mod4_1E08.pdf

