This study aimed to determine the impact of nurse generation on (a) turnover risk factors (low meaning/joy in work, low resilience, high occupational fatigue, high burnout) and (b) turnover intentions before and during the COVID-19 pandemic. Survey methods were used to compare two samples of hospital nurses who completed online surveys in 2017 or 2021. The results were compared on burnout and turnover risk by generation. Results indicate that in 2017, high acute fatigue and low inter-shift recovery differed by nurse generation, with Baby Boomers (Boomers) being the least affected. Additionally, Boomers were the least likely to report a likelihood of leaving the hospital within 6-12 months. However, in 2021, Millennial nurses experienced significantly higher levels of low meaning and joy in work, low resilience, high acute fatigue, low inter-shift recovery, and high burnout than Generation X (GenX) and Boomers. Millennials were the most likely generation to report turnover intention. This leads to the conclusion that the pandemic may have worsened the work experience of millennial nurses and increased their risk of leaving hospital jobs and the profession.
Key Words: nurses, occupational fatigue, burnout, turnover/turnover intention, hospital, pandemic, meaning and joy in work, resilience, nurse generation
The novel coronavirus outbreak was declared an international public health emergency that has affected hospital-based nurses and other clinicians due to the high number of COVID-19 patients, especially during virus surges (International Council of Nurses [ICN], 2021). The high numbers, the levels of care intensity, and the mortality of COVID-19 patients led to hospital staffing and unit changes and increased job demands for frontline nurses (ICN). COVID-19's infectious nature led to nurses enforcing severely restrictive visitation policies, including refusing families to be present with dying patients (Littzen, 2021; Odom-Forren, 2020; Pfefferbaum & North, 2020). The added burdens associated with COVID-19 may have intensified nurses’ desire to leave hospital environments and even nursing. To ameliorate the effects on the impending nursing shortage, nurse leaders must be aware of factors affecting retention and engagement, including generational differences.
Background
During COVID-19, frontline workers experienced mental health distress due to a “lack of personal protective equipment, the physical weight caused by wearing it, fears of contracting COVID-19 and infecting family members, the conflict between safety procedures and the desire to provide support, longer working hours, pressing multitasking, and the stigmatization of people working in high-risk environments” (Giorgi et al., 2020, p. 3). Other work-related sequelae included moral distress due to involvement in resource-allocation decisions related to staffing and limited oxygen, medications, or beds (Fernandez et al., 2020; Odom-Forren, 2020; Pfefferbaum & North, 2020). A systematic review of psychiatric problems for hospital healthcare workers reported that “direct exposure to SARS-CoV-2 patients was the most common risk factor identified for all mental health outcomes except occupational burnout” (Sanghera et al., 2020, p.11). Nurses faced these COVID-19-related work issues against the backdrop of quarantining/social distancing outside the hospital and the economic turmoil caused by the pandemic.
When surveyed during a 2021 pandemic surge, 70% of 8810 acute care and psychiatric mental health nurses reported exhaustion, with 13% indicating that they intended to leave their position within six months for non-retirement reasons (American Nurses Association, 2021). Over half of the nurses reporting turnover intention reported negative effects of work on their health/well-being and insufficient staffing; over a quarter of these nurses sought professional mental health support. The “mass traumatization of the nursing workforce could potentially exacerbate nurse shortages globally” (ICN, 2021, p. 2).
Nurses already experience higher levels of burnout than other healthcare professionals (Sanghera et al., 2020). On average, 11% of nurses worldwide experience high burnout symptoms (Woo et al., 2020), with estimates for burnout in United States nurses being as high as 30-40% (National Academies of Science, 2019). Contributors to burnout are work overload and lack of time and support from superiors (Membrive-Jiménez et al., 2020), and in times of the coronavirus pandemic, the perceived threat of contracting the virus (Manzano García & Ayala Calvo, 2021). Burnout contributes to negative personal and job-related consequences and tends to be greater among younger workers (National Academies of Science, 2019). Thirty-two percent of over 400,000 United States nurses reported burnout as one reason for leaving their jobs in 2017 (Shah et al., 2021). Nurses working in hospitals were more than twice as likely as those working elsewhere to report this trend (Shah et al., 2021).
Factors that protect nurses from turnover and burnout are meaning and joy in work and resilience
Chronic occupational fatigue was the strongest predictor of turnover intentions among hospital nurses pre-pandemic (Lee & Jang, 2020; Rutledge et al., 2021; 2022) and a significant predictor during the coronavirus pandemic (Lavoie-Tremblay et al., 2022). Acute or chronic occupational fatigue results from tiredness that can be overwhelming and may impair function (Smith-Miller et al., 2014). Unchecked chronic fatigue may decrease perceived and actual job performance (Sagherian et al., 2017; Steege & Rainbow, 2017; Winwood et al., 2006). A higher prevalence of fatigue in nurses compared to general workers may be related to rotating shift work, including 12-hour shifts (Smith-Miller et al., 2014), and from nurses picking up extra shifts due to staff shortages, especially during the pandemic (Littzen, 2021). Another factor may be the “supernurse” phenomenon, where the sense of duty preempts personal health (Steege & Rainbow, 2017) or the belief that fatigue-ameliorating offerings are unnecessary (Smith-Miller et al., 2014).
Factors that protect nurses from turnover and burnout are meaning and joy in work and resilience (Rushton et al., 2015; Rutledge et al., 2021). Understanding these factors may help nurses balance health and well-being during disruptive times such as pandemics. A survey of hospital-based young adult nurses during the pandemic found higher resilience was associated with increased work-related well-being (Littzen, 2021). Higher levels of meaning and joy in work mediated the effect of chronic fatigue on turnover intention (Rutledge et al., 2021). Resilience demonstrated a mediating or potentially protective effect on psychological outcomes (depression, PTSD), moral distress, and burnout among hospital nurses (Rushton et al., 2015). Among an international sample of workers, resilience at work was positively related to feeling refreshed from the last period worked, which was negatively associated with acute fatigue (Winwood et al., 2013).
While workplace factors that engage nurses are fairly similar across generations, changes in the workforce environment, such as online job searches and changing norms for staying with a single employer, may make younger nurses less likely to stay in a job despite apparent satisfaction (Koppell, Deline, & Virstis, 2017; Tyndall, Scott, Jones, & Cook, 2019). Generational nurse cohorts had different childhood and educational experiences (Dimock, 2019, January 17) and may also differ in coping with work-related challenges faced during the COVID-19 pandemic. In a mixed-method systematic review, Stevanin and colleagues (2018) found different resilience traits and levels of burnout in nurses from different generations. Among 1500 German/Austrian respondents ages 18 to 99 years, older persons experienced significantly less stress from COVID-19 than younger participants (Schnell & Krampe, 2020). Similarly, in a British sample of university staff, younger age predicted more vulnerability to COVID-19 stress (Van Der Feltz-Cornelis et al., 2020). However, younger nurses may be disproportionately burdened with clinical care delivery to coronavirus patients due to positions as bedside nurses in highly impacted areas (e.g., medical-surgical, critical care).
Yu et al. (2019) found that resilience-mediated job demand factors (e.g., bullying, fatigue) were positively associated with job satisfaction and retention. Among hospital nurses, resilience did not differ across years of experience, but moral distress was higher and hope lower with greater nurse experience (Rushton et al., 2015). In a systematic review (Stevanin et al., 2018), high workloads and interpersonal relationships impacted turnover intention among all generations of nurses. GenX and Millennial nurses perceived the effect on their private lives as significant in their decision to leave their jobs, which was not as important to Boomers. Research is needed to evaluate generational differences in turnover processes and rates (Stevanin et al., 2018) to develop strategies to strengthen the nursing workforce.
Methods
The research question guiding this study is: Before and during the 2020-22 coronavirus pandemic, did generation (Generation Z, Millennial, Generation X, Baby Boomer, Earliers) impact turnover risk factors (low meaning and joy in work, low resilience, high occupational fatigue, and high burnout), and turnover intention among Registered Nurses (RNs)?
This comparative study drew on data from two correlational studies completed at a Southwestern U.S. Magnet-accredited hospital. For Study 1, the 2017 data came from one of two sister hospitals (Rutledge et al., 2021). For Study 2, the data came from a 2021 replication and expansion project at the same hospital during the coronavirus pandemic downturn and vaccination campaign (Rutledge et al., 2022).
Convenience sampling was used to recruit a sample from approximately 1000 RNs. Study 1 included complete responses from 421 RNs, and Study 2 included 151 RNs. Nurses were eligible if they had been employed for three or more months. While fewer nurses participated in Study 2, the participant demographic data is like the larger sample in Study 1 (Table 1). The number of participants in each study and within each generational category was appropriate for planned analysis procedures.
Table 1. Demographic Data
|
|
2017 |
2021 |
||||||
|---|---|---|---|---|---|---|---|---|
|
Variable |
N |
% |
Mean |
SD |
N |
% |
Mean |
SD |
|
Years in nursing |
421 |
|
18.05 |
13.13 |
151 |
|
17.21 |
13.22 |
|
Years in position |
421 |
|
8.77 |
8.59 |
151 |
|
8.40 |
8.88 |
|
Years at hospital |
421 |
|
12.32 |
11.52 |
149 |
|
11.96 |
10.06 |
|
Agea |
413 |
|
44.21 |
12.54 |
150 |
|
45.03 |
12.81 |
|
Generation |
|
|
|
|
|
|
|
|
|
Before 1945 |
2 |
0.48 |
|
|
0 |
0 |
|
|
|
Boomer |
121 |
29.30 |
59.26 |
4.18 |
30 |
19.87 |
63.77 |
4.21 |
|
GenX |
163 |
39.47 |
43.96 |
4.44 |
62 |
41.06 |
48.40 |
4.35 |
|
Millennial |
126 |
30.51 |
29.67 |
3.76 |
55 |
36.42 |
32.16 |
4.55 |
|
After 1996 |
1 |
0.24 |
|
|
3 |
1.99 |
|
|
|
Genderb |
|
|
|
|
|
|
|
|
|
Female |
381 |
90.51 |
|
|
135 |
89.40 |
|
|
|
Male |
36 |
8.55 |
|
|
14 |
9.27 |
|
|
|
Other |
0 |
0 |
|
|
1 |
0.66 |
|
|
|
Nursing education |
|
|
|
|
|
|
|
|
|
Masters or higher |
78 |
18.53 |
|
|
34 |
22.52 |
|
|
|
Baccalaureate |
262 |
63.23 |
|
|
98 |
64.90 |
|
|
|
Associates |
73 |
17.34 |
|
|
16 |
10.60 |
|
|
|
Diploma |
8 |
1.9 |
|
|
1 |
.66 |
|
|
|
Not Stated |
0 |
0 |
|
|
2 |
1.32 |
|
|
|
Hospital work settingc |
|
|
|
|
|
|
|
|
|
Behavioral health |
0 |
0 |
|
|
2 |
1.32 |
|
|
|
Critical care |
54 |
12.83 |
|
|
19 |
12.58 |
|
|
|
Emergency care |
52 |
12.35 |
|
|
13 |
8.61 |
|
|
|
Medical surgical |
97 |
23.04 |
|
|
54 |
35.76 |
|
|
|
Surgical services |
29 |
6.89 |
|
|
10 |
6.62 |
|
|
|
Women’s health |
62 |
14.73 |
|
|
24 |
15.89 |
|
|
|
Other |
127 |
30.17 |
|
|
29 |
19.21 |
|
|
|
Specialty certification |
218 |
51.78 |
|
|
94 |
62.25 |
|
|
aMissing age data for 8 (2017) and 1 (2021) participants.
bMissing gender data for 4 (2017) and 1 (2021) participants.
cAmbulatory departments were listed under their patient specialty.
Procedures
All nurses on the all-RN hospital listserv received email invitations from study investigators in April of each study year. Second and third reminder invitations were deployed weekly. Respondents received no incentives. Surveys were collected anonymously using Qualtrics (2017) and RedCAP (2021) software, which are both compliant with the General Data Protection Regulation and California Consumer Privacy Act. The health system human research protection program determined both studies exempt from full board review.
Measures
Demographics and Turnover Intention. On a demographic questionnaire, nurses reported their gender; birthyear; education; number of years as an RN, in the hospital, and in their current position; nursing role (clinical/staff nurse vs. other); and certification in a specialty (yes/no).
Generation was calculated by subtracting nurse birthyear from survey year and recoding into generational cohorts as defined by the Pew Research Center (Dimock, 2019, January 17). Nurses were categorized as “Boomers” born between 1946 – 1964; “Generation X” born between 1965 – 1980; or “Millennials” born between 1981 – 1996. Due to small counts, respondents born before 1946 (2017 = 2); after 1996 (2017 = 1; 2021 = 3); or missing age data (2017 = 8; 2021 = 1) were removed from the generational analysis, leaving 410 (2017) and 147 (2021) cases.
Nurse turnover intention has been associated with actual turnover (Kelly et al., 2021). Therefore, Intention to leave the hospital was measured using the question: How likely is it that in the next 6 months to a year you will leave the hospital for another nursing position? Responses were scored from extremely unlikely (1) to extremely likely (5); nurses were considered to have turnover intention if they scored 4 or 5. In 2021, responses of 4 or 5 warranted a follow-up question as to whether the nurse was leaving due to obtaining a new position after earning an advanced degree or for planned retirement. Intention to leave nursing was measured with a similar question and response set: How likely is it that in the next 6 months to a year you will leave nursing?
Nurses were categorized as “Boomers” born between 1946 – 1964; “Generation X” born between 1965 – 1980; or “Millennials” born between 1981 – 1996.
Meaning and Joy in Work were measured using the total scale score for the 17-item meaning and joy in work questionnaire (Rutledge et al., 2018). Prior work shows high internal consistency among items (Rutledge et al., 2021; 2022). The items use a 5-point response set: strongly disagree (1) to strongly agree (5), with higher scores reflecting greater meaning and joy in work.
Resilience. The 20-item Resilience at Work scale was used to measure work-related resilience (Winwood et al., 2013). This scale has shown adequate psychometric strength in prior work (Rutledge et al., 2022; Winwood et al., 2013) and uses a response set from strongly disagree (1) to strongly agree (7). Higher scores reflect greater resilience.
Burnout. Burnout was measured using the 22-item Maslach Burnout Inventory – Health Services Survey (MBI-HSS) with three subscales: emotional exhaustion, depersonalization, and personal accomplishment. Multiple studies support MBI-HSS as a sound instrument (Maslach et al., 2018; Rutledge et al., 2022). Item response set was never (0) to every day (6). Higher total scores, higher emotional exhaustion, higher depersonalization, and lower personal accomplishment reflected higher burnout. Scoring guidelines (MindGarden, Menlo Park [CA], USA) suggest that high levels of subscale constructs are reflected by the following cut-offs: emotional accomplishment > 27, depersonalization > 13. Overall burnout (yes/no) occurred when nurses had high levels of both emotional accomplishment and depersonalization, associated or not with low personal accomplishment. We did not report the total burnout scores (the sum of the three subscales) but used overall burnout as a metric.
Occupational Fatigue. Three subscales from the occupational fatigue exhaustion recovery or OFER-15 scale (Winwood et al., 2006; Winwood et al., 2005) were used: chronic fatigue, acute fatigue, and inter-shift recovery. Each subscale has five items with 7-point response sets. Adequate psychometric properties, including subscale internal consistencies, have been reported for the OFER-15 (Rutledge et al., 2021; 2022; Winwood et al., 2006).
Data Analysis
The 2017 and 2021 data sets were inspected and cleaned as detailed previously (Rutledge et al., 2021; 2022). Each of those studies focused on specific variables’ ability to predict hospital turnover intention; both showed that the variables of interest for this comparative study were statistically significant predictors of turnover intention. For the current study, each turnover intention risk factor variable was divided into low-risk or high-risk categories using (a) pre-established cut-scores determined by prior research (e.g., MBI-HSS), (b) logical cut-scores agreed upon by the research team (e.g., intention to leave the hospital), or (c) quartiles (e.g., OFER-15, Meaning and Joy at Work). Generational cohorts were determined as detailed above and chi-square tests were performed to determine whether significant differences existed among generations on each predictor. Analyses were conducted in R version 3.6.1 using R Studio.
Results
Table 1 shows the similarity between participants from the two data sets. Nurses were predominantly female (approximately 90%), well-educated (82% baccalaureate or higher), and certified in a specialty (52% or higher). They averaged 18 years of experience in nursing (with an average of 12 years at the study hospital) and worked across all hospital specialty areas. A greater portion of 2021 nurses worked in medical-surgical units (36%) than in the 2017 group (23%) since several units had changed patient allocation due to the pandemic. In 2021, a smaller portion of participants (20%) were Boomers than in 2017 (29%). We believe planned and early retirements due to COVID led to this change, which matches national trends in nurses over 50 (Buerhaus et al., 2022). There were small, corresponding increases among 2017 nurses designated as GenX and Millennials, as demonstrated by the 4-year mean age gain within each generational cohort for the 2021 sample.
Differences in Risk Factors and Turnover Intentions over Time
Table 2 depicts generational differences for each turnover risk factor. Because data on resilience and burnout were unavailable for Study 1, we cannot address 2017 generational differences or changes over time for these measures. By showing no greater than a 5% change, proportions of Boomers with workforce engagement factors pointing to a high likelihood of turnover remains relatively consistent from 2017 to 2021 for all factors. The same can be said for GenX nurses, except for the intention to leave the hospital, which decreased from 16% in 2017 to 6.5% in 2021. However, Millennial nurses demonstrate large proportional changes in turnover risk factors from 2017 to 2021, with increases in low meaning and joy in work (35.5% to 50.9%) and high acute fatigue (26.2% to 36.4%). Slightly higher proportions of nurses experienced low inter-shift recovery and high chronic fatigue in 2021 than in 2017. Millennials showed smaller changes in proportions reporting intention to leave the hospital or nursing (<5%).
Generational Differences for Turnover Risk Factors and Turnover Intentions
Table 2 shows whether changes in proportions of nurses by generation differed significantly by risk factor for each study. Generational differences in meaning and joy in work were significant in 2021 but not in 2017; 20-24% more 2021 Millennial nurses were experiencing low meaning and joy in work than were Boomers or GenX nurses. In 2021, significantly more Millennials experienced low resilience than Boomers or GenX nurses. High acute fatigue and low inter-shift recovery mimicked these relationships: significantly more Millennial nurses reported these than other nurse generations. However, no significant generational differences were found for high chronic fatigue in either year.
Two burnout measures differed significantly by generation, as seen in Table 2 (Study 2 only). High depersonalization was experienced by few Boomers (2%), by 11% of GenX nurses, and by 26% of Millennials. This same generational pattern was found with the overall burnout measure (high emotional exhaustion + high depersonalization). Millennials are six times as likely to have overall burnout than Boomers and three times as likely as GenX nurses. High emotional exhaustion was not experienced significantly differently across generations, although almost twice as many Millennials (38.2%) experienced this as did Boomers (20.0%).
Turnover intention differed significantly by generation for leaving the hospital and only for 2017 participants (see Table 2). Fewer 2017 Boomers (6.6%) intended to leave the hospital than did GenX nurses (16.0%) and Millennials (19.1%). In 2021, the proportion of Millennials indicating intent to leave the hospital in 6-12 months (14.6%) was two times greater than GenX (6.5%) and four times greater than Boomers (3.3%).
Table 2. Workforce Engagement Risk Factors for Turnover and Turnover Intentions: Percentage of Nurses by Generation (2017, 2021)
|
|
Study 1 2017 (N = 410) |
Study 2 2021 (N = 147) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Risk Factor |
Cut-score |
Boomer |
GenX |
Millennial |
p-value |
Cut-score |
Boomer |
GenX |
Millennial |
p-value |
|
Low MJW |
≤ 4 |
23.1 |
33.7 |
35.5 |
ns |
≤ 4 |
23.3 |
30.7 |
50.9 |
0.018 |
|
Low RAW |
- |
- |
- |
- |
- |
≤ 5.05 |
23.3 |
16.1 |
38.2 |
0.023 |
|
High AF |
≥ 83.3 |
13.2 |
20.3 |
26.2 |
0.039 |
≥ 76.7 |
13.3 |
19.4 |
36.4 |
0.029 |
|
Low IR |
≤ 40 |
18.2 |
22.1 |
38.1 |
0.001 |
≤ 40 |
20.0 |
17.7 |
43.6 |
0.004 |
|
High CF |
≥ 63.3 |
21.5 |
23.3 |
20.6 |
ns |
≥ 66.7 |
26.7 |
22.6 |
23.6 |
ns |
|
Burnout |
|
|
|
|
|
|
|
|
|
|
|
High EE |
- |
- |
- |
- |
- |
≥27 |
20.0 |
24.6 |
38.2 |
ns |
|
High DP |
- |
- |
- |
- |
- |
≥13 |
1.5 |
10.8 |
25.5 |
0.014 |
|
High EE + DP |
- |
- |
- |
- |
- |
- |
3.3 |
6.2 |
20.0 |
0.021 |
|
Turnover intention |
|
|
|
|
|
|
|
|
|
|
|
Leave hospital |
≥4 |
6.6 |
16.0 |
19.1 |
0.014 |
≥4 |
3.3 |
6.5 |
14.6 |
ns |
|
Leave nursing |
≥4 |
4.1 |
3.1 |
8.7 |
ns |
≥4 |
6.7 |
4.8 |
5.5 |
ns |
Note. MJW = meaning and joy in work; RAW = resilience at work; AF = acute fatigue; IR = inter-shift recovery; DP = depersonalization; EE = emotional exhaustion. Quartile calculations were used to determine cut scores for MJW, AF, IR, and CF. Scores at or above (below) the “Cut Score” are coded as “High” (“Low”) for each variable. Burnout factor cut scores were determined using the scoring guidelines recommended by MindGarden with overall Burnout (yes) assigned when both EE and DP were high. Turnover intention cut scores were determined as a score of 4 or 5 indicating intent to leave.
Figure 1 depicts study data for turnover risk factors that indicated significant generational differences. The 2017 data demonstrates that nurse generation differs for high acute fatigue and low inter-shift recovery, with Boomers being the least affected. Boomers were the least likely to report being likely to leave the hospital within 6-12 months. However, Study 2 - done 14 months into the coronavirus pandemic – shows a different story: more Millennial nurses exhibited high levels of low meaning and joy in work, low resilience, high acute fatigue, low inter-shift recovery, and high burnout. They are the most likely generation (although not significantly different) to report the intention to leave the hospital.
Figure 1. Turnover risk factors by generation (2017, 2021)
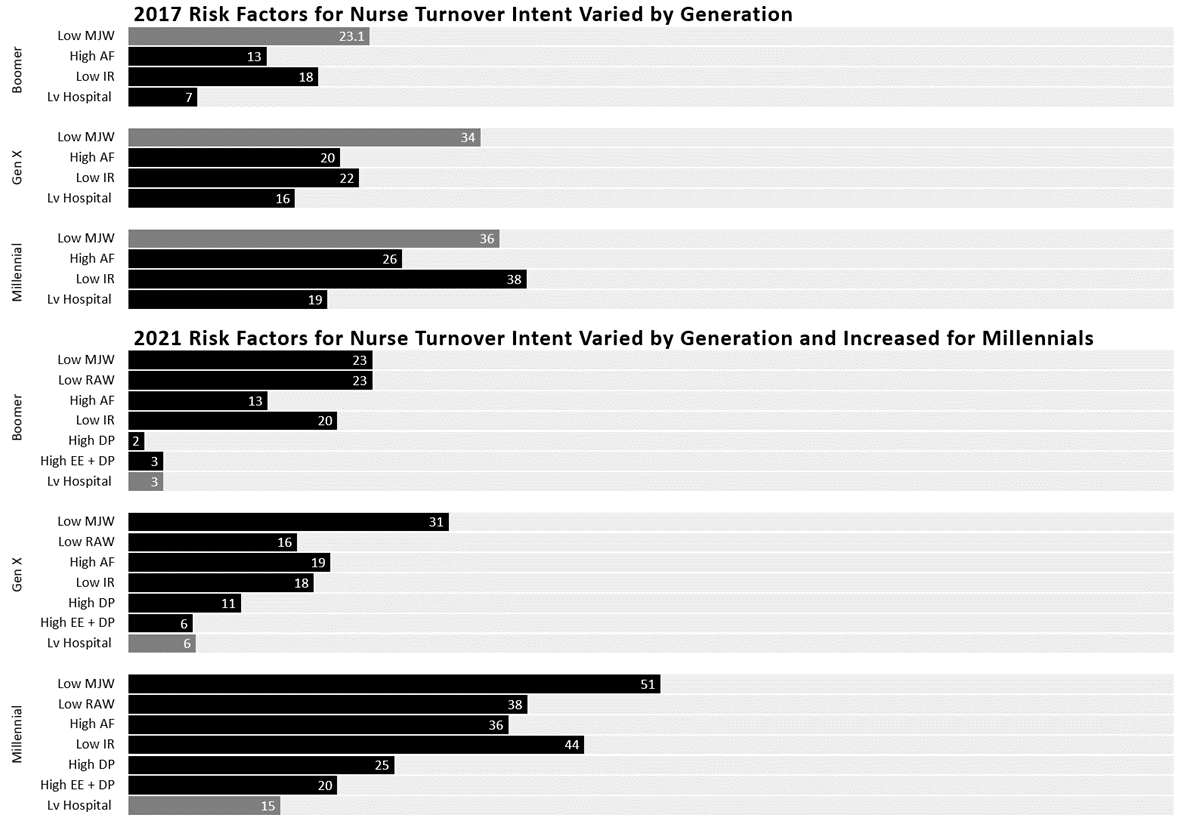
Note. MJW = meaning and joy in work; AF = acute fatigue; IR = inter-shift recovery; RAW = resilience at work; DP = depersonalization; EE = emotional exhaustion Dark bars represent percentage of each cohort that scored at or above (below) each cut score. Only risk factors that showed statistically significant (p < .05) differences among generations in at least one study are displayed. For instance, chronic fatigue (CF) is not shown because, although it was a significant predictor of intent to leave, there was no difference in CF among generations in either study year. Bars are shaded lighter when there were not statistically significant (p < .05) differences among generations in that study year.
Discussion
Our findings also show continued differences in levels of high acute fatigue and low inter-shift recovery across generations, with alarmingly high levels among Millennial nurses
This is the first known study to examine whether hospital nurses of varying generations differ on workforce engagement factors linked with turnover intention and to compare findings before and during the coronavirus pandemic. The American Nurses Foundation is conducting an ongoing series of surveys to determine the impact of the pandemic on nurses (American Nurses Association, 2022). Table 3 compares specific findings from this national dataset (collected through January 2022) among available age groups. This national survey and extant literature (Fernandez et al., 2020) support our findings in documenting the negative impact of working during the pandemic on hospital-based Millennial nurses. Our findings also show continued differences in levels of high acute fatigue and low inter-shift recovery across generations, with alarmingly high levels among Millennial nurses, which have increased from 2017 (pre-pandemic) to 2021 (during the pandemic). This documents what many nurse leaders already know: frontline nurses are predominantly younger, providing demanding, hospital-based care and they are suffering.
Table 3. Pertinent Factors among Hospital/Psychiatric Facility Nurses from 2022 American Nurses Association National Survey: Percentage by Age Groups Available (American Nurses Association, 2022)
|
Factor |
25-44 yrs N = 2793 |
45-54 yrs N = 1640 |
55+ yrs N = 1792 |
|---|---|---|---|
|
Feeling exhausted |
79% |
69% |
57% |
|
Feeling burnout |
68 |
53 |
38 |
|
Feeling unsupported |
53 |
48 |
37 |
|
Sought mental health support |
42 |
30 |
20 |
|
Intent to leave position next 6 months |
Yes 30 Maybe 32 |
Yes 22 Maybe 33 |
Yes 21 Maybe 26 |
|
Reasons for turnover intention Inadequate staffing Work negatively affecting personal well-being Lack of support from employer during pandemic |
66 60 48 |
62 53 44 |
50 47 36 |
|
What organization could do to increase work satisfaction Increase salary, wages, bonuses Increase number of nurses or support staff |
76 66 |
64 61 |
57 55 |
The pandemic may have disproportionately worsened the work experience for Millennial hospital nurses, as Figure 1 shows. In 2017, Millennials reported slightly higher turnover risk factors than other generational groups, perhaps because they were newer to the profession (presumably like the Boomers and GenX nurses who were unhappy and left their cohort years ago when they were the same age Millennials were in 2017). There will be some people who will leave any profession that is not right for them. However, the 2021 data shows that Boomers and GenX nurses remain relatively constant in their experiences with turnover risk, while turnover risk factors for Millennials demonstrate that more nurses experience poor work engagement and, thus, a higher risk of leaving the hospital setting.
Chronic fatigue has predicted turnover intentions among nurses pre- and post-pandemic (American Nurses Association, 2021, 2022; Lavoie-Tremblay et al., 2022; Lee & Jang, 2020; Rutledge et al., 2021; 2022). While chronic occupational fatigue did not differ among generations in our study, precursors to chronic or persistent fatigue -- acute fatigue and inter-shift recovery (Winwood et al., 2005; 2006) -- were significantly greater among Millennial nurses before and during the pandemic. These nurses may be working until acutely fatigued and returning to work unrested (low inter-shift recovery). Thus, they are more vulnerable to the detrimental consequences of stress at work (Smith-Miller et al., 2014; Winwood et al., 2013). Hospital leaders are encouraged to monitor occupational fatigue and implement interventions to maximize fatigue amelioration among Millennials and other nurses experiencing high acute fatigue and low inter-shift recovery. In a scoping review of strategies to address retention of Millennial nurses, authors suggest the following ways to ameliorate professional fatigue: promote safety and proper allocation of resources, provide adequate support for Millennials to perform their jobs, and address the continuous change that exists in many hospital settings (McClain, Arnold, Palokas, & Christian, 2021). Considering that acute fatigue and inter-shift recovery may lead to chronic fatigue (Winwood et al., 2006) and that chronic fatigue predicts nurse turnover intentions (Rutledge et al., 2021; 2022), monitoring occupational fatigue and using evidence-based strategies to prevent and combat fatigue among nurses are warranted (National Institute for Occupational Safety and Health; Redeker et al., 2019). Specific strategies to ameliorate occupational fatigue include nap-at-work programs and scheduling policies that prevent excessive work hours.
Our findings about burnout come only from the 2021 sample (during the pandemic) and point to the presence of troubled Millennial nurses, consistent with extant literature (National Academies of Science, 2019). In our study, more Millennials had high levels of depersonalization than other generations, indicating a risk of exhibiting impersonal responses toward patients (Maslach et al., 2018). In our prior analysis (Rutledge et al., 2022), depersonalization had a small but significant correlation with working on coronavirus units (r = .22, p < .01), and nurse age and percent of time spent on coronavirus units were inversely related (r = -.33, p < .01), indicating that younger nurses were spending significantly more time on these “hot” units. Compared with older nurses, female Japanese nurses younger than 40 had significantly higher work- and personal burnout levels and were more likely to report the intention to leave their positions (Minamizono et al., 2019). In that sample, perceptions of job support were protective against turnover intentions. Given the potential effect of burnout on turnover intention, the percentage of Millennials experiencing high levels of overall burnout found in our study is concerning due to the likely detrimental effect on patient care delivery and organizational stability.
The protective factors against turnover and turnover intention examined in this study indicate possible problems retaining millennial nurses. In this study, over half of Millennial nurses working during the pandemic experienced low meaning and joy in work, and almost 40% experienced low resilience at work. An earlier study found that meaning and joy in work mediated the impact of chronic occupational fatigue on turnover intention among hospital nurses (Rutledge et al., 2021). Rushton et al. (2015) found resilience and burnout inversely related among critical care and medical-surgical nurses. Yu et al. (2019) concluded that resilience is negatively associated with job demands (e.g., burnout) and positively associated with job resources (e.g., wellbeing). With low levels of perceived meaning and joy and resilience in work and high levels of depersonalization, Millennial nurses working during the pandemic may be at great risk for inadequate patient care as well as leaving their jobs and perhaps leaving nursing (Muir, Wanchek, Lobo, & Keim-Malpass, 2021).
Mentorship, empowerment, and allowing others to be empowered give nurse managers meaning and joy (Hahn et al., 2021), but no evidence identifies what enhances meaning and joy in work for Millennials. However, a recent concept analysis found that Millennials “place more importance than previous generations on areas such as pay, time off, personal work interactions, self-benefits of work and support of their managers/leaders” (p. 935) and want personal attention from their leaders (Campbell & Patrician, 2020). In a cost-consequence analysis, Muir et al. (2021) found that the burnout costs for newly hired nurses are higher in a control hospital than those in a hospital that uses salary increases to enhance retention. Organizational leadership is encouraged to offer Millennial nurses personal attention and self-scheduling when possible.
Nurse turnover is a complex issue, complicated by the pandemic, that is not amenable to any single solution. While differences in nurse reactions to working during the pandemic across countries and regions are likely (Holton et al., 2021; Şanlıtürk, 2021), given the severity of burnout and suffering reported by Millennial and GenX hospital nurses, hospital leaders must enhance their awareness of potential preventive and treatment strategies for poor work engagement. A large cross-sectional study with pre-pandemic data found that about a third of nurses who had left their jobs in the past year (or intended to leave in the next year) attributed their decision to burnout, particularly related to stressful work environments without adequate staffing (Shah et al., 2021). Maslach and Leiter suggest that “initiatives to moderate workload demands complemented by improvements in recovery strategies through better sleep, exercise, and nutrition have direct relevance to the exhaustion component of burnout” (2016, p. 109). Finally, understanding the reward value of Millennial nurses may impact burnout and turnover intention. Millennials value recognition, sustained experience with committed leaders, professional growth opportunities (e.g., tuition reimbursement), alignment of organizational core values with their own, good coworker relations, and optimal technology (Keith et al., 2021; Littzen, 2021; McClain et al., 2021; Waltz et al., 2020). Table 4 lists nurse-focused offerings that may assist hospitals with their initiatives to enhance nurse retention.
Table 4. Select Offerings Available to Assist with Nurse Retention (may require membership to obtain specific resources)
|
Offering |
Sponsoring Organization |
Access URL |
|---|---|---|
|
2022 Healthcare Workforce Rescue Package |
National Academy of Medicine and content experts |
|
|
The Well -Being Initiative |
Partners: American Association of Critical Care Nurses, American Nurses Foundation, American Nurses Association, American Psychiatric Nurses Association, Emergency Nurses Association |
|
|
Staff Retention Tool Kit for Nurse Executives |
American Nurses Association |
Nurse Retention Tool Kit - American Nurse (myamericannurse.com) |
|
PODCAST Episode 187: The Critical Need for Well-Being and Resiliency and How to Practice |
Oncology Nursing Society |
Episode 187: The Critical Need for Well-Being and Resiliency and How to Practice | ONS |
|
Career Coaching |
Association of periOperative Registered Nurses |
AORN Career Center | Career Coaching Services - Dr. Phyllis Quinlan |
|
Find Your Forward: Resources for Advocacy and Strength (sample topics: Meaningful recognition, overcoming burnout, providing self-care and finding harmony |
Sigma Theta Tau International |
|
|
Burnout Prevention Program |
May be free to American Nurses Association members |
https://www.sehealthcarequalityconsulting.com/nurse-burnout-prevention-program/ |
Limitations
Study findings come from a single Southwestern U.S. hospital with Magnet designation, limiting generalizability to similar settings. Data came from self-report and may be influenced by response bias. Data from Studies 1 and 2 were not linked by individual participants, disallowing strong parametric testing; however, samples were similar in major characteristics. Our sample size in 2021 was insufficient to categorize generational data by nurse role, which might have given information about the intersection of generation with clinical (or patient-facing) nursing roles compared to non-clinical roles. However, these findings offer insight into the phenomenon.
Conclusion
The pandemic has created an international crisis for nurse leaders regarding how to retain nurses. Understanding turnover risk factors among nurses is vital. This study adds information about the potential impact of nurse generation on protective and negative workforce engagement factors among hospital nurses before and during the coronavirus pandemic. In responding to potential turnover problems, nurse leaders might consider whether Millennial nurses have carried a disproportionate share of the care burden during the pandemic and how to mitigate its impacts moving forward.
Authors
Dana Rutledge
Email: Dana.Rutledge@stjoe.org
Dr. Dana Rutledge is experienced in designing and facilitating research and evidence-basedprojects on various topics and has authored/co-authored more than 70 publications. Dr. Rutledge recently retired from California State University Fullerton, where she worked with Doctor of Nursing Practice students. She has been a nursing research consultant at St. Joseph Hospital (Orange, CA) since 2007.
Sarah Douville
Email: sarah.douville@cgu.edu
Sarah Douville has a business management and finance background with 20 years of experience in data analysis and program evaluation in healthcare education. She manages a softwarecompany that tracks student academic progress, and she is completing a PhD focused on program evaluation at Claremont Graduate University.
Elizabeth Winokur
Email: ewinoku2@calstatela.edu
Dr. Elizabeth Winokur is a leader in nursing education and research/evidence-based practice. Dr. Winokur has over 40 years of experience in emergency and critical care nursing in diverse roles, including department educator and director. She has additional clinical expertise in burn nursing, sexual assault, and child abuse. Dr. Winokur is the Acting Director and Associate Professor of Nursing at California State University, Los Angeles, and a Nursing Research Facilitator at St. Joseph Hospital, Orange, CA.
References
American Nurses Association. (2021). Year One COVID-19 Impact Assessment Survey https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/year-one-covid-19-impact-assessment-survey/
American Nurses Association. (2022). COVID-19 Survey Series: Two-Year Impact Assessment. https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/covid-19-impact-assessment-survey---the-second-year/
Buerhaus, P. I., Staiger, D. O., Auerbach, D. I., Yates, M. C., & Donelan, K. (2022). Nurse employment during the first fifteen months of the COVID-19 pandemic. Health Affairs (Millwood), 41, 79-85. https://doi.org/10.1377/hlthaff.2021.01289
Campbell, C. M., & Patrician, P. A. (2020). Generational preferences in the nursing work environment: A dimensional concept analysis. Journal of Nursing Management, 28, 927-937. https://doi.org/10.1111/jonm.13024
Dimock, M. (2019, January 17). Defining generations: Where milennials end and Generation Z begins. Pew Research Center Facttank. https://www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins/
Fernandez, R., Lord, H., Halcomb, E., Moxham, L., Middleton, R., Alananzeh, I., & Ellwood, L. (2020). Implications for COVID-19: A systematic review of nurses' experiences of working in acute care hospital settings during a respiratory pandemic. International Journal of Nursing Studies, 111, 103637. https://doi.org/10.1016/j.ijnurstu.2020.103637
Giorgi, G., Lecca, L. I., Alessio, F., Finstad, G. L., Bondanini, G., Lulli, L. G., Arcangeli, G., & Mucci, N. (2020). COVID-19-related mental health effects in the workplace: A narrative review. International Journal of Environmental Research & Public Health, 17(21). https://doi.org/10.3390/ijerph17217857
Hahn, J., Galuska, L., Polifroni, E. C., & Dunnack, H. (2021). Joy and meaning in nurse manager practice: A narrative analysis. Journal of Nursing Administration, 51, 38-42. https://doi.org/10.1097/nna.0000000000000964
Holton, S., Wynter, K., Rothmann, M. J., Skjoeth, M. M., Considine, J., Street, M., Hutchinson, A., Khaw, D., Hutchinson, A. M., Ockerby, C., Crowe, S., Trueman, M., Sweeney, S., Bruce, S., & Rasmussen, B. (2021). Australian and Danish nurses' and midwives' wellbeing during COVID-19: A comparison study. Collegian. https://doi.org/10.1016/j.colegn.2021.10.010
International Council of Nurses (ICN). (2021). Policy brief: The global nursing shortage and nurse retention. https://www.icn.ch/sites/default/files/inline-files/ICN%20Policy%20Brief_Nurse%20Shortage%20and%20Retention.pdf
Keith, A. C., Warshawsky, N., & Talbert, S. (2021). Factors that influence millennial generation nurses' intention to stay: An integrated literature review. Journal of Nursing Administration, 51, 220-226. https://doi.org/10.1097/nna.0000000000001001
Kelly, L. A., Gee, P. M., & Butler, R. J. (2021). Impact of nurse burnout on organizational and position turnover. Nursing Outlook, 69, 96-102. https://doi.org/10.1016/j.outlook.2020.06.008
Koppel, J., Deline, M., & Virkstis, K. (2017). The case for focusing on millennial retention. Journal of Nursing Administration, 47(7-8), 361-363. https://doi.org/10.1097/nna.0000000000000495
Lavoie-Tremblay, M., Gélinas, C., Aubé, T., Tchouaket, E., Tremblay, D., Gagnon, M. P., & Côté, J. (2022). Influence of caring for COVID-19 patients on nurse's turnover, work satisfaction and quality of care. Journal of Nursing Management, 30, 33-43. https://doi.org/10.1111/jonm.13462
Lee, E., & Jang, I. (2020). Nurses' fatigue, job stress, organizational culture, and turnover intention: A culture-work-health model. Western Journal of Nursing Research, 42, 108-116. https://doi.org/10.1177/0193945919839189
Littzen, C. O. R. (2021). Young adult nurse work-related well-being, contemporary practice worldview, resilience, and co-worker support during the covid-19 pandemic [Dissertation] https://repository.arizona.edu/bitstream/handle/10150/660275/azu_etd_18756_sip1_m.pdf?sequence=1&isAllowed=y
Manzano García, G., & Ayala Calvo, J. C. (2021). The threat of COVID-19 and its influence on nursing staff burnout. Journal of Advanced Nursing, 77, 832-844. https://doi.org/10.1111/jan.14642
Maslach, C., Jackson, S. E., & Leiter, M. P. (2018). Maslach Burnout Inventory Manual (4th ed.) www.mindgarden.com
Maslach, C., & Leiter, M. P. (2016). Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry, 15(2), 103-111. https://doi.org/10.1002/wps.20311
McClain, A. R., Arnold, A., Palokas, M., & Christian, R. (2021). Retention strategies and barriers for millennial nurses: A scoping review protocol. JBI Evid Synth, 19(4), 867-873. https://doi.org/10.11124/jbies-20-00091
Membrive-Jiménez, M. J., Pradas-Hernández, L., Suleiman-Martos, N., Vargas-Román, K., Cañadas-De la Fuente, G. A., Gomez-Urquiza, J. L., & De la Fuente-Solana, E. I. (2020). Burnout in nursing managers: A systematic review and meta-analysis of related factors, levels and prevalence. International Journal of Environmental Research & Public Health, 17(11). https://doi.org/10.3390/ijerph17113983
Minamizono, S., Nomura, K., Inoue, Y., Hiraike, H., Tsuchiya, A., Okinaga, H., & Illing, J. (2019). Gender division of labor, burnout, and intention to leave work among young female nurses in japan: A cross-sectional study. . International Journal of Environmental Research & Public Health, 16(12). https://doi.org/10.3390/ijerph16122201
Muir, K. J., Wanchek, T. N., Lobo, J. M., & Keim-Malpass, J. (2021). Evaluating the costs of nurse burnout-attributed turnover. A Markov modeling approach. J Patient Saf, 1-7. https://doi.org/10.1097/PTS.0000000000000920
National Academies of Science, E. M. (2019). Taking action against clinician burnout: A systems approach to professional well-being. The National Academies Press.
National Institute for Occupational Safety and Health. NIOSH training for nurses on shift work and long work hours. Retrieved July 4, 2021 from https://www.cdc.gov/niosh/work-hour-training-for-nurses/default.html
Odom-Forren, J. (2020). Nursing resilience in the world of COVID-19. Journal of PeriAnesthesia Nursing, 35, 555-556. https://doi.org/10.1016/j.jopan.2020.10.005
Pfefferbaum, B., & North, C. S. (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383, 510-512. https://doi.org/10.1056/NEJMp2008017
Redeker, N. S., Caruso, C. C., Hashmi, S. D., Mullington, J. M., Grandner, M., & Morgenthaler, T. I. (2019). Workplace interventions to promote sleep health and an alert, healthy workforce. Journal of Clinical Sleep Medicine, 15, 649-657. https://doi.org/10.5664/jcsm.7734
Rushton, C. H., Batcheller, J., Schroeder, K., & Donohue, P. (2015). Burnout and resilience among nurses practicing in high-intensity settings. American Journal of Critical Care, 24, 412-420. https://doi.org/10.4037/ajcc2015291
Rutledge, D. N., Douville, S., Winokur, E., Drake, D., & Niedzela, D. (2021). Impact of engagement factors on nurses’ intention to leave hospital employment. Journal of Nursing Management, 29, 1554-1564. https://doi.org/10.1111/jonm.13287
Rutledge, D. N., Douville, S., & Winokur, E. J. (2022). Chronic fatigue predicts hospital nurse turnover intentions. Journal of Nursing Administration, 52. https://doi.org/10.1097/NNA.0000000000001139
Rutledge, D. N., Wickman, M., & Winokur, E. (2018). Instrument validation: Hospital nurse perceptions of meaning and joy in work. Journal of Nursing Measurement, 26(33), 579-588. https://doi.org/10.1891/1061-3749.26.3.579
Sagherian, K., Clinton, M. E., Abu-Saad Huijer, H., & Geiger-Brown, J. (2017). Fatigue, work schedules, and perceived performance in bedside care nurses. Workplace & Health Safety, 65, 304-312. https://doi.org/10.1177/2165079916665398
Sanghera, J., Pattani, N., Hashmi, Y., Varley, K. F., Cheruvu, M. S., Bradley, A., & Burke, J. R. (2020). The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting-A systematic review. Journal of Occupational Health, 62(1), e12175. https://doi.org/10.1002/1348-9585.12175
Şanlıtürk, D. (2021). Perceived and sources of occupational stress in intensive care nurses during the COVID-19 pandemic. Intensive & Critical Care Nursing, 67, 103107. https://doi.org/10.1016/j.iccn.2021.103107
Schnell, T., & Krampe, H. (2020). Meaning in life and self-control buffer stress in times of COVID-19: Moderating and mediating effects with regard to mental distress. Frontiers of Psychiatry, 11, 582352. https://doi.org/10.3389/fpsyt.2020.582352
Shah, M. K., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469. https://doi.org/10.1001/jamanetworkopen.2020.36469
Smith-Miller, C. A., Shaw-Kokot, J., Curro, B., & Jones, C. B. (2014). An integrative review: fatigue among nurses in acute care settings. Journal of Nursing Administration, 44, 487-494. https://doi.org/10.1097/nna.0000000000000104
Steege, L. M., & Rainbow, J. G. (2017). Fatigue in hospital nurses — ‘Supernurse’ culture is a barrier to addressing problems: A qualitative interview study. International Journal of Nursing Studies, 67, 20-28. https://doi.org/https://doi.org/10.1016/j.ijnurstu.2016.11.014
Stevanin, S., Palese, A., Bressan, V., Vehviläinen-Julkunen, K., & Kvist, T. (2018). Workplace-related generational characteristics of nurses: A mixed-method systematic review. Journal of Advanced Nursing, 74, 1245-1263. https://doi.org/10.1111/jan.13538
Tyndall, D. E., Scott, E. S., Jones, L. R., & Cook, K. J. (2019). Changing new graduate nurse profiles and retention recommendations for nurse leaders. Journal of Nursing Administration, 49, 93-98. https://doi.org/10.1097/nna.0000000000000716
Van Der Feltz-Cornelis, C. M., Varley, D., Allgar, V. L., & de Beurs, E. (2020). Workplace stress, presenteeism, absenteeism, and resilience amongst university staff and students in the COVID-19 lockdown. Frontiers of Psychiatry, 11, 588803. https://doi.org/10.3389/fpsyt.2020.588803
Waltz, L. A., Muñoz, L., Weber Johnson, H., & Rodriguez, T. (2020). Exploring job satisfaction and workplace engagement in millennial nurses. Journal of Nursing Management, 28, 673-681. https://doi.org/10.1111/jonm.12981
Winwood, P. C., Colon, R., & McEwen, K. (2013). A practical measure of workplace resilience: developing the resilience at work scale. Journal of Occupational & Environmental Medicine, 55(10), 1205-1212. https://doi.org/10.1097/JOM.0b013e3182a2a60a
Winwood, P. C., Lushington, K., & Winefield, A. H. (2006). Further development and validation of the Occupational Fatigue Exhaustion Recovery (OFER) scale. Journal of Occupational & Environmental Medicine, 48, 381-389. https://doi.org/10.1097/01.jom.0000194164.14081.06
Winwood, P. C., Winefield, A. H., Dawson, D., & Lushington, K. (2005). Development and validation of a scale to measure work-related fatigue and recovery: the Occupational Fatigue Exhaustion/Recovery Scale (OFER). Journal of Occupational & Environmental Medicine, 47, 594-606.
Woo, T., Ho, R., Tang, A., & Tam, W. (2020). Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. Journal of Psychiatric Research, 123, 9-20. https://doi.org/10.1016/j.jpsychires.2019.12.015
Yu, F., Raphael, D., Mackay, L., Smith, M., & King, A. (2019). Personal and work-related factors associated with nurse resilience: A systematic review. International Journal of Nursing Studies, 93, 129-140. https://doi.org/10.1016/j.ijnurstu.2019.02.014


