The nursing profession continues to struggle to find the most appropriate approach to credentialing Advanced Practice Registered Nurses (APRNs). One early step in addressing this struggle is determining the incidence of APRN disciplinary actions by boards of nursing. This article presents data from 2003 and 2004 describing the incidence of APRN disciplinary actions by United States boards of nursing. Fifty-one boards of nursing, all members of the National Council of State Boards of Nursing, were asked to report the numbers of APRN discipline cases for 2003 and 2004 which had been resolved, using a tool that differentiated disciplinary cases into four data categories: chemical impairment, exceeding scope of practice, unprofessional conduct, and safety or abuse of patients. Thirty-eight (74.5%) of 51 boards of nursing reported discipline data for a total of 125,882 APRNs showing 688 disciplinary actions were taken during 2003 and 2004. This indicates that APRNs experience a low incidence of discipline related to chemical impairment, exceeding scope of practice, unprofessional conduct, and safety or abuse of patients.
Key Words: advanced practice registered nurse, APRN, boards of nursing, chemical dependence, discipline, patient abuse, regulation, safe practice, scope of practice, unprofessional conduct.
The nursing profession has struggled for some time to find the most appropriate approach to credentialing Advanced Practice Registered Nurses. |
The nursing profession has struggled for some time to find the most appropriate approach to credentialing Advanced Practice Registered Nurses. Yet we still lack clarity regarding the effectiveness of the current system of regulation, including the extent to which APRNs are being disciplined by regulatory boards. Although the literature documents the nursing profession's and patients’ responses to many APRN interventions, it does not document the incidence of APRN discipline by regulatory boards (Carson-Smith & Klein, 2003; Cipher, Hooker, & Sekscenski, 2006; Fanta et al., 2006; Jastremski, 2002; Laurant et al., 2005; Mundinger et al., 2000; National Practitioner Data Bank, 2006; Wortans, Happel, & Johnstone, 2006).
Two viewpoints emerged within the last year related to APRN regulation. One viewpoint was presented by regulators in the form of a draft position paper on the future of APRN regulation (National Council of State Boards of Nursing [NCSBN], 2006a). The second viewpoint was presented by various stakeholder groups in response to that position paper (American Association of Colleges of Nursing, 2006; American Academy of Nurse Practitioners, 2006; American Nurses Credentialing Center, 2006; National Association of Clinical Nurse Specialists, 2006; National Organization of Nurse Practitioner Faculty, 2006). The difference between these two viewpoints centered around the need for APRNs to hold a second authorization to practice. Regulators contended that APRNs have a different scope of practice than a registered nurse and therefore require additional testing and authorization to practice, while stakeholder groups saw advanced practice nursing as a component of the continuum of nursing, and therefore within the overall scope of registered nursing practice. During these discussions, regulators were challenged to produce evidence that related to the amount and kind of APRN disciplinary problems addressed by boards of nursing. The regulators were able to cite only one relevant study on this matter, a study which reported that APRNs have similar public safety issues as licensed practical and registered nurses (Apple, 2004). These discussions at the National Council of State Boards of Nursing (NCSBN) APRN Roundtable questioning the incidence of APRN disciplinary issues addressed by boards of nursing served as the impetus for this survey. Stimulated by the challenge to document the volume of disciplinary actions taken by boards of nursing against APRNs, the survey described below was undertaken through the Institute of Regulatory Excellence sponsored by the NCSBN (2006b).
Survey Method
Time Frame
To answer the survey question, namely what is the number of APRN disciplinary cases in each of four discipline subject (data) categories during 2003 and 2004, data was requested from 51 boards of nursing in the United States (US), including the District of Columbia. These years were chosen because the data collection time of fall 2005 and spring 2006 allowed sufficient time for nursing boards to effectively resolve cases for the preceding two years and have the most current data to report.
Procedure
Boards were asked to use a survey data collection tool, distributed in both electronic and hard copy formats, to report all resolved complaints resulting in actions against an APRN’s license or practice authorization in 2003 and 2004. APRNs included
...each state has the constitutional right to establish its own health-related laws, rules, and regulations. |
certified registered nurse anesthetists (CRNAs), nurse practitioners (NPs), certified nurse midwives (CNMs), and clinical nurse specialists (CNSs). This data can be obtained for review from all boards of nursing, although there is variation from state to state on complaint investigation management procedures and the disciplinary process. This variation occurs because each state has the constitutional right to establish its own health-related laws, rules, and regulations. In all states, the APRN has the right to legal representation and the rights of the individual being investigated must be protected under due process (Nester, 2003).
Survey Data Collection Tool
Four discipline (data) categories, specifically (a) chemical impairment, (b) exceeding the scope of practice, (c) unprofessional conduct and (d) patient abuse or unsafe acts, were chosen for study because they represent the most commonly disciplined areas across all board of nursing jurisdictions. All boards discipline for chemical impairment, although other terms such as diversion, drug and alcohol use, and narcotic use may be used, as well as scope of practice and patient abuse/neglect/endangerment. States vary, however, in what they choose to classify as unprofessional conduct. Some states require that misdemeanor and felony convictions impact the nursing license while other states allow boards of nursing to give individual consideration of the circumstances. The objective of this survey was to report all APRN discipline for all states, including the District of Columbia, in a way which would capture as many discipline actions as possible considering the state-to-state variability which exists. Hence, definitions of discipline categories were crafted in this survey to include as many state-specific variations as possible. The tool, developed for this survey, provided specific definitions for, and examples of discipline in the four categories as described below.
Discipline. Discipline was defined as a formal action taken by a board of nursing or a court, whereby an APRN received a formal letter of reprimand, a restriction placed on an active license or certification, such as a prohibition against narcotic access, restriction from participating in the multi-state licensure compact, suspension with or without a stay, a suspension or probation with remedial conditions which might include civil penalties, or a revocation which might include civil penalties. In the remainder of this article, a restriction on either an active license or authorization to practice as an APRN will be referred to as a restriction on authorization.
Chemical impairment. Chemical impairment discipline was based either on admission and negotiated settlement or conviction of drug use, drug diversion, or alcohol use. Examples of discipline that fell within this category were diverting drugs ordered for a patient for self use, calling in an unauthorized prescription for oneself or a family member with the intent of using the medication for oneself, stealing medications, unauthorized use of sample medications, driving under the influence (DUI) conviction, violation of a court-ordered probation related to chemical dependence, or violation of a recovery program contract resulting in board action. In this category, APRNs who voluntarily surrendered their license or authorization and entered into a board-approved treatment program without a formal disciplinary process were not included in the disciplinary total because voluntary surrender of a license did not fall within the legal definition of a disciplinary process.
Exceeding scope of practice. Exceeding scope of practice discipline included participating in those activities not generally recognized to be acceptable or customarily performed by others within the same licensure or authorization role and category and who had similar educational preparation and experience. Specifics for this disciplinary category differed from state-to-state, depending on individual state statute.
Since the 1995 Social Policy Statement by the American Nurse’s Association (ANA) defining the expansion of advanced practice nursing (ANA, 1995), many states have modified nurse practice act statute language to change or delete required APRN supervision by physicians (Pearson, 2003; Phillips, 2006; Rollet, 2004). Many states have also more broadly defined APRN scopes of practice, meaning that authorization for the roles of nurse practitioner, nurse midwife, nurse anesthetist, and clinical nurse specialist is more common than more restrictive authorization to a category within a role, such as being authorized to practice as an emergency room nurse practitioner, a school nurse practitioner, or an oncology clinical nurse specialist (Idaho Board of Nursing, 2006). This more restrictive authorization could lead to scope of practice violation by an APRN if, for example, the APRN was authorized to practice as an emergency nurse practitioner; but, due to lack of job opportunity, began employment as a primary care nurse practitioner in a family practice setting or as a women's health nurse practitioner in a clinic. These new practices would not be within the scope of practice of an emergency nurse practitioner, unless the nurse practitioner obtained more formal education in the new category and completed the regulatory requirements to expand his/her practice (Klein, 2004; Texas Board of Nurse Examiners, 2006).
Additional issues for scope of practice arise when the APRN crosses state borders, resides in a border area and may live in one state and work in another, or in both states, gives telephone advice to patients in another state, participates in telehealth, or telephones prescriptions to a pharmacy in another state that may not recognize APRN authority to prescribe and may require some degree of physician supervision or collaboration. Discipline in this category also includes those instances of writing and issuing a prescription signed by another provider, such as a supervising physician leaving a blank prescription pad for use as needed, in states that do not allow the APRN prescriptive privileges. All of these issues make scope of practice an area that often lacks clarity (Klein, 2004).
Unprofessional conduct. Unprofessional conduct discipline was a broad term chosen to encompasses a wide variety of actions including practice on an expired authorization, presenting oneself as a physician, fraud, dishonorable or unethical conduct, falsification of records, and legally required disciplinary action for conviction of crimes not necessarily related to APRN practice, such as failure to pay child support, robbery, assault, and other misdemeanors and felonies up to and including murder.
Patient abuse and unsafe acts. Patient abuse or safety neglect discipline included any activity that would place a patient in danger or demonstrate blatant disregard for patient safety and wellbeing. Examples are abandonment, boundary violations, sexual misconduct, and improper dispensing or prescribing of medications.
States Included in Survey
Data was collected on a state-to-state basis and participating states were told data would be reported as aggregate data. Thirty-eight of fifty-one (74.5%) Boards of Nursing reported a total of 125,882 active APRN authorizations in the four roles. All thirty-eight states reported disciplinary data indicating action against an APRN authorization holder. Eight boards of nursing (15.7%), Indiana, Kansas, Louisiana, Maine, Montana, New Jersey, Pennsylvania, and Rhode Island, did not provide data and were not included in the study. Five boards of nursing (9.8%), Colorado, Iowa, South Carolina, Tennessee and Virginia, reported they only discipline the RN license, which automatically further impacts the APRN authorization, thus they do not identify separate APRN discipline and could not capture the data without arduous manual review of each case. These five states were also excluded from the study. Ten boards of nursing, Alaska, Connecticut, Florida, Michigan, Mississippi, Nebraska, Nevada, New Hampshire, New York and Utah, representing 26.3% of the 38 boards reporting for this survey and 19.6% of all 51 boards, cited the clinical nurse specialist functions under the RN scope of practice and did not further identify CNSs separately from RNs who were not CNSs. Hence, discipline of these CNSs is found only within the RN discipline numbers.
Survey Findings
Exceeding the scope of practice was the least problematic for APRNs at 137 cases (20%) of all discipline. |
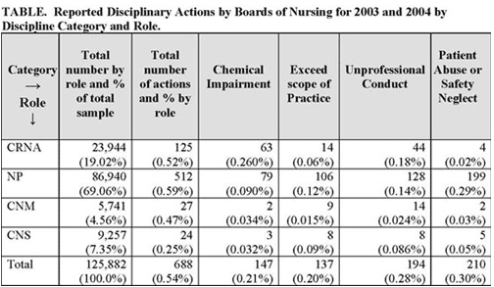
The sum of all actions for all four APRN groups was 688 reported actions, representing action against 0.54% of the 125,882 APRN in the sample. Raw Data for all groups are reported in the Table. Although the sample does not include APRNs from every state, there was a good geographic representation from across the United States. Discipline data reported showed consistently low numbers of discipline across all states, whether they were compared by numbers of authorizations in a state or by geographic region of the United States.
Nurse practitioners were the largest reported APRN role comprising 86,940 (69%) of the 125,882, followed by CRNA at 23,944 (19%). The number of APRNs in this study identified as being in the CNS role, specifically 9,257, speaks to the problem of getting an accurate accounting of CNS numbers and supports earlier concerns that the discipline
...[During data analysis] the author identified the need to separate registered nurse and APRN data in board of nursing reports... |
has a problem because it is not possible to get an accurate handle on the number of CNS in the US (Lyon, 2004). Some CNSs earn a master’s degree yet continue to practice within the RN scope of practice in traditional hospital roles. Others do not feel the need to obtain a second practice authorization, or they cannot because such a practice authorization requires passing a certification exam, and no exam exists for their practice specialty. The government reports that only 16% of nurses prepared at the master’s level as a CNS actually hold a position with the title of CNS (U.S. Department of Health and Human Services [USDHHS], 2004).
For the 688 reported APRN discipline cases, patient abuse and safety issues were the most frequent cause for discipline representing 210 cases (30%) of all discipline. Unprofessional conduct represented 194 cases (28%) and chemical impairment 147 cases (21.5%). Exceeding the scope of practice was the least problematic for APRNs at 137 cases (20%) of all discipline.
Limitations of the Survey
A limitation of this survey study is that eight state boards of nursing did not report disciplinary data and five could not differentiate between RN and APRN discipline. Although there are low numbers of disciplinary actions compared to the number of authorizations reviewed, there was no investigation made to determine whether an individual authorized APRN had more than one disciplinary action. There was also no way to identify whether an APRN was authorized in more than one role, such as an APRN who is both a CNS and an NP. Furthermore, the inability to collect data on those who are authorized and who receive letters of warning or caution from boards, which differ from formal letters of reprimand and are not considered formal discipline, and those who voluntarily surrender an authorization and enter a board approved chemical dependency recovery program presents additional limitations. The number of clinical nurse specialists reported as regulated by boards of nursing versus the number educated for the role and considering themselves to be clinical nurse specialists as reported to the USDHHS also limits the data from showing the full picture.
A major limitation to assessing all violations by any regulatory board is that in order for cases to be investigated and brought before a board, violations must first be reported. Reporting remains an ongoing issue because of the caring nature of nurses. Peers and employers, who are in a position to first identify problems, usually move to a “saving” intervention by removing the person from the situation either by reassignment or employment termination. Reporting to a regulatory board is often not considered as a first line option and thus the numbers of reported cases investigated, and those that actually go to a full disciplinary process, cannot be considered to represent a totally inclusive picture of actual APRN behavior.
Conclusion
This survey found that state boards of nursing...report low numbers of APRN discipline cases. |
This survey found that state boards of nursing are consistent in defining areas of discipline and that they report low numbers of APRN discipline cases. These findings suggest the incidence of APRN discipline for chemical impairment, exceeding the accepted scope of practice, unprofessional conduct, and abuse of patients and neglect of their safety is minimal in the United States. During the course of analyzing this data, the author identified the need to separate registered nurse and APRN data in board of nursing reports, to make available on public websites annual summaries of board of nursing disciplinary data, and to obtain an accurate count of the number of clinical nurse specialists within the country.
DISCLAIMER: This study was completed as an independent project through the Institute of Regulatory Excellence Fellowship Program, sponsored by the National Council of State Boards of Nursing, and does not represent any position, official approval, or the views of NCSBN.
The author wishes to thank Charlene Hanson, EdD, FNP and Ann L. O'Sullivan, PhD, CRNP, PNP for editorial and analytical assistance.
Author
Randall Hudspeth, MS, APRN-CNS/NP
Email: randhuds@sarmc.org
Randall Hudspeth, MS, APRN-CNS/NP, received his BSN from Idaho State University and MS as a Clinical Nurse Specialist (CNS) from Syracuse University and Nurse Practitioner (NP) certification from The University of Arizona. He is certified through American Nurses Credentialing Center as a medical/surgical CNS and as an Adult NP; he is also certified in pain management. He is a member of the Idaho State Board of Nursing representing advanced practice and has served two terms as Chairman. He is a fellow in the Institute of Regulatory Excellence sponsored by the NCSBN and is a member of the NCSBN Advanced Practice Advisory Committee. He serves on the editorial boards of Nursing Administration Quarterly and MODRN Nurse Magazine. He is the director of Advanced and Specialty Practice and of the Heart and Vascular Center at Saint Alphonsus Regional Medical Center, Boise, ID.
References
American Academy of Nurse Practitioners. (2006). AANP's comments of the vision paper, the future regulation of advanced practice nursing. Retrieved August 9, 2006 from: www.aanp.org/NR/Publications/AANP+Position+Statements/Position+Statements+and+Papers.asp/ .
American Association of Colleges of Nursing. (2006). AACN's response to the vision paper, the future regulation of advanced practice nursing. Retrieved August 9, 2006 from: www.aacn.nche.edu/education/AACNResp.htm .
American Nurses Association. (1995). Nursing: A social policy statement. Kansas City, MO: Author.
American Nurses Credentialing Center. (2006). Response to the vision paper, the future regulation of advanced practice nursing.
Apple, K., (2004). Letter to the editor. Clinical Nurse Specialist, 18(3), 103-106.
Carson-Smith, W., & Klein, C., (2003). Nurse practitioner errors lead to litigation. Nurse Practitioner, 28(3), 52, 55-57.
Cipher, D.J., Hooker, R.S., & Sekscenski, E. (2006). Are older patients satisfied with physician assistants and nurse practitioners? Journal of the American Association of Physician Assistants, 9(1), 36, 39-40, 42-44.
Fanta, K., Cook, B., Falcone, R.A. Jr., Rickets, C., Schweer, L., & Brown, R.L., (2006). Pediatric trauma nurse practitioners provide excellent care with superior patient satisfaction for injured children. Journal of Pediatric Surgery, 41(1), 277-281.
Idaho State Board of Nursing. (2006). Administrative rules of the board of nursing, scope of practice of advanced practice professional nurse. Retrieved November 10, 2006 from: www.adm.idaho.gov/adminrules/rules/idapa23/0101.pdf .
Jastremski, C.A. (2002). Using outcomes research to validate the advanced practice nursing role administratively. Critical Care Nursing Clinics of North America, 14(3), 275-280.
Klein, T. (2004). Scope of practice and the nurse practitioner: Regulation, competency, expansion, and evolution. Topics in Advanced Practice Nursing eJournal. Retrieved November 10, 2006 from: www.medscape.com/viewarticle/495161.
Laurant, M., Reeves, D., Hermens, R., Braspenning, J., Grol, R., & Sibbald, B. (2005). Substitution of doctors by nurses in primary care. Retrieved September 5, 2006 from: www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001271/frame.html .
Lyon, B. (2004). The CNS regulatory quagmire, We need clarity about advanced nursing practice. Clinical Nurse Specialist, 18(1), 9-13.
Mundinger, M., Kane, R., Lenz, E., Totten, A., Tsai, W., et al. (2000). Primary care outcomes in patients treated by nurse practitioners or physicians. Journal of the American Medical Association, 283(1), 59-68.
National Association of Clinical Nurse Specialists. (2006). NACNS talking points on NCSBN vision statement. Retrieved July 17, 2006 from: www.nacns.org/papers.shtml .
National Council of State Boards of Nursing. (2006a). APRN vision paper, the future regulation of advanced practice nursing. Retrieved August 9, 2006 from: https://www.ncsbn.org/Draft_APRN_Vision_Paper.pdf .
National Council of State Boards of Nursing, (2006b). NCSBN institute of regulatory excellence fellowship program. Retrieved November 10, 2006 from: www.ncsbn.org .
National practitioner data bank. (2006). Retrieved August 9, 2006 from: www.npdb-hipdb.com/npdb.html .
National Organization of Nurse Practitioner Faculty. (2006). NONPF response to vision paper, he future regulation of advanced practice nursing. Retrieved November 10, 2006 from: www.nonpf.com.
Nester, M.A., (2003). Defending yourself against a board of nursing complaint. Advanced Nursing Practice, 11(8), 22.
Pearson, L., (2003). Fifteenth annual update: How each state stands on legislative issues affecting advanced nursing practice. Nurse Practitioner, 28(1), 26-27, 31-32.
Phillips, S. (2006). A comprehensive look at the legislative issues affecting advanced nursing practice. The Nurse Practitioner, 30(1), 14-47.
Rollet, J. (2004). Annual legislative update. State initiatives in 2004. Advanced Nursing Practice, 12(12), 51-53.
Texas Board of Nurse Examiners. (2006). Guidelines for determining APN scope of practice. Retrieved November 10, 2006 from: ftp://www.bne.state.tx.us/apn-scope.pdf .
U.S. Department of Health and Human Services. (2004). Preliminary findings: 2004 national sample survey of registered nurses. Retrieved November 10, 2006 from: http://bhpr.hrsa.gov/healthworkforce/reports/rnpopulation/preliminaryfindings.htm.
Wortans, J., Happel, B., & Johnstone, H., (2006). The role of the nurse practitioner in psychiatric mental health nursing: Exploring consumer satisfaction. Journal of Psychiatric Mental Health Nursing, 12(1), 78-84.