In 2020, the COVID-19 pandemic impacted the United States and the global healthcare system. The lack of agency and national stockpiles of personal protection equipment led to rationing and alteration in best infection prevention practices. The lack of resources forced nurses to make decisions based on resources rather than evidence. This article offers a brief review of the tenants of evidence-based practice, and discusses EBP during the COVID-19 pandemic. Presented is information about the concepts important to a resource-based view, and a potential modification of an EBP model that adds the perspective of resource-based practice to include the actual availability of resources to inform clinical decision-making by nurses and other providers.
Key Words: Nurses, Florence Nightingale, evidence-based practice, personal protective equipment, personal protective equipment guidelines, COVID-19, pandemic, CDC, WHO, rationing, resource-based view, resource-based practice
...nurses have found themselves in uncharted waters as providers in the global healthcare system navigate the response to this diseaseThe year 2020 has been designated the “Year of the Nurse and Midwife” to mark 200 years since the birth of Florence Nightingale. Nightingale, while working on the front lines during the Crimean War, used evidence to make practice decisions that solidified her role as one of the first nurse researchers, and arguably, one of the early disaster epidemiologists (Aravind & Chung, 2010). The role of nurses has been highlighted and challenged significantly in the face of a novel coronavirus (COVID-19) pandemic that unfolded globally. Due to the lack of new knowledge, existing evidence, and lack of recommended resources, nurses have found themselves in uncharted waters as providers in the global healthcare system navigate the response to this disease. Unlike Nightingale, nurses on the front lines of the current COVID-19 pandemic it seems have been providing care not based on best evidence, but instead are making clinical nursing decisions based on available resources.
Late in 2019, COVID-19 emerged in Wuhan, China. The virus transmission was established as human to human respiratory secretions, and it quickly spread throughout the world (Wu & McGoogan, 2020). Thus, nurses around the world entered a time of great uncertainty as they cared for others in a pandemic environment. Treatment and guidelines from the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) have changed rapidly and, at times, were conflicting. As became clear, there was a shortage of personal protective equipment (PPE). Guidelines then shifted from evidence-based practice (EBP) to resource-based view to inform practice.
Guidelines then shifted from evidence-based practice (EBP) to resource-based view to inform practiceMisinformation or conjecture about the virus was broadcast on social media (Harman, 2020; Kulami et al., 2020). Confirmation bias compounded the confusion as healthcare workers searched for information to confirm their own beliefs or disbeliefs about the virus (Garcia-Alamino, 2020). As the global healthcare community begins and continues to test for and collect data on the virus, evidence-based recommendations will start to emerge.
Evidence-Based Practice
The goal of EBP is to use the best evidence to make healthcare decisions and guide interventions to improve patient outcomes. The EBP movement started with the recognition that there was an undesirable knowledge disparity in what we discern and what we do in the care of individuals (Stevens, 2013). Nurses are at the frontline of patient care and in this role are vital to critically evaluate and apply evidence to inform nursing practice. EBP models include steps to find and evaluate the evidence. One frequently used model includes the following five steps: 1) Ask the clinical question; 2) Find the best evidence; 3) Evaluate and critically appraise the evidence; 4) Integrate the evidence with clinical expertise, patient characteristics, patient values, and healthcare resources available; and 5). Assess the effectiveness of the process. Clinical questions are often asked in a structure that includes population, intervention, comparison, and outcomes (PICO); and they occasionally also indicate a timeframe (PICOT) (Melnyk & Fineout-Overholt, 2004; Melnyk et al., 2014).
The COVID-19 pandemic is creating great challenges for nurses and the healthcare systemFor almost two decades, EBP models have been introduced to nurses in the academic setting and also endorsed in clinical practice. Nursing leaders have evaluated nursing practice and evidence, and conscientiously attempted to implement evidence-based care into practice. The COVID-19 pandemic is creating great challenges for nurses and the healthcare system. The nursing community had only minimal evidence about the novel coronavirus and a short time to deploy resources once the first cases arrived in New York. The lack of healthcare resources and the absence of standard protocols further compounded this situation (Kennedy, 2020).
Upon attempting to critically appraise the evidence during the COVID-19 pandemic, several important questions about the use of EBP surfaced. These included:
- What if there is no evidence to review?
- What if the resources and interventions that we know are best practices are not available?
- What if the credible authorities' guidelines contraindicate the best evidence?
These questions gave leaders in the healthcare community a great pause, and have created unrest and fear. It is also notable to acknowledge that the current generation of Americans has not experienced national level rations in their lifetime. There are examples of rationing of insufficient PPE has been repeatedly noted in novel virus outbreaks in areas outside of the United States (U.S.), such as: SARS-CoV in China (2002-2003); MERS-CoV in Saudi Arabia (2012) and Ebola in Sierra Leone (2014) (Kermode et al., 2005; Kilmarx et al., 2014; Murphy, 2006; Rebmann & Carrico, 2017). Unavailability of tangible resources in the United States is a foreign concept, but is paving the way for healthcare reform and re-evaluation of agency preparedness and the Strategic National Stockpile of PPE in the United States.
Unavailability of tangible resources in the United States is a foreign concept...Melnyk and Fineout-Overholt (2011) clearly described the EBP culture and environment to include: research evidence and evidence-based theories; patient preferences and values; clinical expertise; evidence from the assessment of the patient history/condition; and healthcare resources to inform clinical decision making. Healthcare resources are included in the EBP model, yet this criterion has not been a primary focus. Instead, the focus highlighted the best evidence. The focus quickly changed to emphasize healthcare resources as the world faced the pandemic. The U.S. healthcare infrastructure promptly became overwhelmed in New York City (Chokshi & Katz, 2020).
Healthcare resources are included in the EBP model, yet this criterion has not been a primary focusHealthcare resources include healthcare personnel, space, equipment, ventilators, and PPE, all of which became limited during the COVID-19 pandemic. The healthcare community had ample reason to be fearful about the lack of PPE as reports from China, Italy, Spain, and the United States indicated that frontline healthcare providers were becoming infected, and in some cases, suffered fatalities (CDC, 2020, April 2017; European Centre for Disease Prevention and Control, 2020; Remuzzi & Remuzzi, 2020; Zhan et al., 2020).
EBP during the COVID-19 Pandemic
In January 2020, the first patient diagnosed in Washington State moved the pandemic to the domestic ground on both coasts of the United States (Goldstein & McKinley, 2020; Holshue et al., 2020). At the same time, reports of healthcare workers becoming infected became evident. PPE supplies became scarce with healthcare agencies and the public competing to purchase equipment. Non-medical respirator masks, disinfectants, gloves, gowns, and hand sanitizers also became scarce (Beradi et al, 2020). All of these factors created a perfect storm once it became apparent that the virus became a domestic infection control issue in the United States.
With novel diseases, the mode of transmission is often unknownHealthcare providers were acutely aware of the WHO guidelines and recommendations for novel acute respiratory infections to prevent and control pandemic-prone acute respiratory infections. With novel diseases, the mode of transmission is often unknown. Best practice endorsed by the CDC and WHO indicated implementation of the highest level of infection control measures until the identification of the mode of transmission, resulting in improved understanding of the situation. Thus, until the current pandemic, the N95 respirator was recommended for healthcare workers working with patients who had suspected novel viruses (WHO, 2014).
In February 2020, COVID 19 was identified as SARS-CoV-2; this novel virus had sequence similarity to SARS-CoV (77.5%) and MERS-CoV (50%) (Kim et al., 2020). The WHO declared COVID 19 a public health emergency, and then a pandemic. It was established quickly that, much like MERS and SARS, persons in contact with symptomatic individuals were the most susceptible to the novel coronavirus COVID-19. Thus, it was determined that healthcare providers were in particular need of PPE. Shortages of masks, PPE, and the lack of precise testing supplies and processes left healthcare workers vulnerable as the recommended equipment was not available. Also complicating the situation was a lack of concrete knowledge about how the virus was transmitted.
To date, COVID-19 is known to be spread by inhalation of respiratory droplets typically by close contact of less than 6 feet with individuals positive for the virus, and contact with surfaces/fomites that contain the virus with subsequent cross-contamination with the mucous membranes (CDC, 2020, August 4; WHO, 2020, March 29). There is also ongoing investigation about whether COVID-19 leads to intestinal infection and lives in air samples (Zhang et al., 2020).
It is hypothesized that COVID 19 is transmitted via the airborne route during aerosol-generating procedures. This may include transmission during such procedures as intubation; cardiopulmonary resuscitation (CPR); bronchoscopy; open suctioning; administration of nebulized medication; manual ventilation before intubation; turning patients to prone position; disconnecting individuals from the ventilator; tracheostomy; and non-invasive positive pressure ventilation (WHO, 2020, April 6). During procedures that generate aerosols, PPE requires much in addition to hand hygiene, a respirator mask, gown, goggles, and gloves.
The CDC statement about the scarcity of PPE, and instructions for healthcare providers to use scarves and bandanas if there are no masks available exemplifies the difference between practice informed by the resource-based view, versus evidence-based practice. The CDC released the following statement:
"in settings where facemasks are not available, HCP might use homemade masks (e.g., bandana, scarf) for the care of patients with COVID-19 as a last resort. However, homemade masks are not considered PPE, since their capability to protect HCP is unknown. Caution should be exercised when considering this option. Homemade masks should ideally be used in combination with a face shield that covers the entire front (that extends to the chin or below) and sides of the face" (CDC, 2020, June 28, para 18)
National and state healthcare agencies worked together to allocate supplies and develop strategies to extend PPE, and started to use PPE contingencies. The CDC (2020, June 28) offered a resource-based recommendation for healthcare providers to extend the use of respirators, facemasks, and. eye protection beyond single-use contact; beyond the manufacturer designated shelf life; and reprocessing of single-use equipment. The WHO (2020, April 6) made a resource-based recommendation for reusing masks after a review of previous studies focused on reprocessing masks from 1978-2020. However, the methodology, randomization, and the number of masks processed were not included in this report.
Many nurses regard PPE as a safety measure for security and protectionTo many nurses, the commodity of PPE serves as a basic need in the delivery of patient care. Many nurses regard PPE as a safety measure for security and protection. When assessing Maslow's (1943) hierarchy of needs after physiologic conditions, safety needs dominate behavior. The feeling of being unsafe is a probable explanation of why the general public and the healthcare community were fearfully motivated because of the shortage of PPE. Quickly, an appraisal of healthcare resources in regard to PPE moved from evidence-based practice to a resource-based view.
Resource-Based View
Although well known in business and management circles, Resource-Based View (RBV) is not formally used to appraisee resources in the healthcare system; instead, it is a tool to identify competitive strategies for sustainable businesses. The RBV examines strategic resources and capabilities, including two sets of routines: performing tasks and coordinating tasks over time and the ability to maintain sustainability (Barney, 1991; Helfat & Petered, 2003). Strategic resources are considered valuable, rare or scarce, difficult to imitate, and non-substitutable.
The RBV assesses resources as tangible or intangible; heterogenous or homogenous; and mobile or immobileThe RBV assesses resources as tangible or intangible; heterogenous or homogenous; and mobile or immobile. Capital and physical attributes, such as building, equipment, land, or mineral reserves, are examples of tangible resources. Intangible resources include individuals, knowledge, technology, reputation, and organization culture. Specialized skills and capabilities represent unique heterogeneous resources that give an organization a strategic edge (Barney, 1991). An example of having homogenous resources is when every organization has the same amount and mix if resources to meet demand all the time. Immobile resources do not move from one company to another company; examples are branding, manufacturing processes, and intellectual property. Although the attributes of resources being heterogeneous and immobile are different goals as compared to the healthcare model, the goal of the RBV model is to acquire a competitive advantage to stand out from competitors. Competition aside, some tenants of this theory may apply to the acquisition of strategic healthcare resources.
Resource-Based Practice
Modifying the resource-based view may allow this model to be applied to healthcareIt is paramount to include the appraisal of healthcare resources, given that access to healthcare resources directly affects clinical decision making. Modifying the resource-based view may allow this model to be applied to healthcare. It makes sense to appraise resources to allow availability of heterogeneous and immobile resources to provide care for a greater number of individuals. Building a healthcare system that is cost-efficient and sustainable is also essential.
Tangible and Intangible Resources
The healthcare system relies on the tangible and intangible resources described above. For almost two decades Americans have ranked the character of nurses, noting their high ethical standards, trust, and honesty (Reinhart, 2020). The culture of caring is a goal of patient-centered care. In the future, classifications of resources, including human resources, must be accounted for and added to the modified model as a separate category for assessment. Human resources, including nurses, embody the healthcare team's capacity for communication, collaboration, and motivation. Figure 1 illustrates the important concepts that include evaluation of available resources to support the healthcare resource-based view and how it can impact patient outcomes.
Figure 1. Healthcare Resource-based View Impact on Patient Outcomes
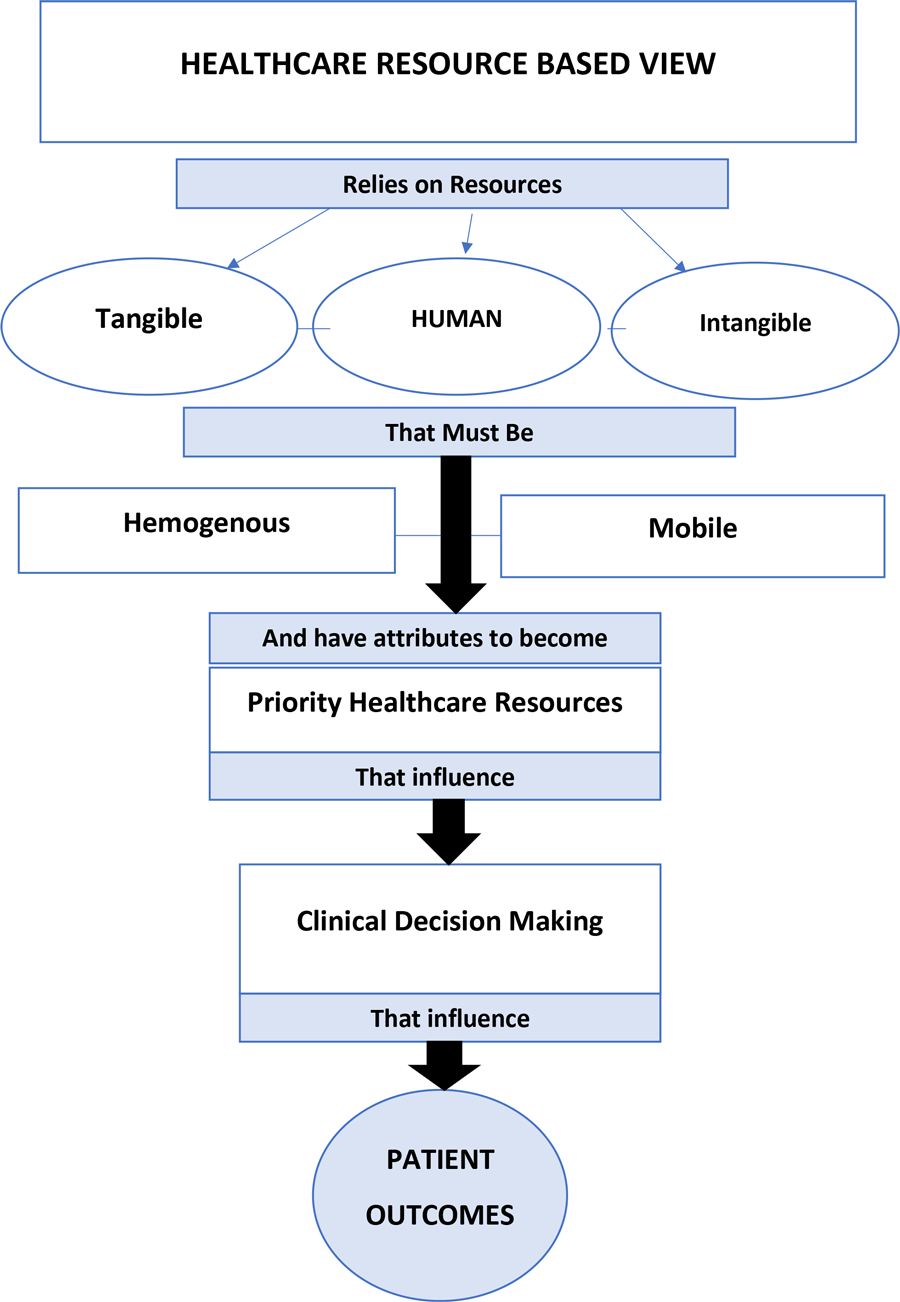
[View full size] (Barney, 1991)
Homogenous and Mobile Resources
Tangible, intangible, and human healthcare resources must also be homogenous and mobile in times of healthcare crisis. Supply and demand can fluctuate rapidly in a crisis and provides another factor inhibiting a homogenous healthcare arena. It is important adequate resources are available to maintain a homogenous healthcare environment and to produce optimal patient outcomes.
Homogenous Resources. In business terms, heterogenous means aspiring to have different resources than other organizations to have a competitive edge in the market. Heterogenicity of resources can cause resource inequity between organizations. Additionally, heterogenous resources can affect how organizations cooperate and coordinate to achieve a common goal. Promoting a heterogenous business environment places individual organizational needs as a priority (Barney, 1991) For example, some organizations may have the capacity to contribute to a common community goal yet do not participate in order to maintain a competitive edge over organizations they feel are competing against (Barney, 2001).
...strategic resources that are uniquely heterogeneous and immobile are not favorable traits for healthcare resourcesIn healthcare, we work as a large team, and we have a fragmented resource supply. Resources that are supported by best evidence such as medications and equipment, should be highly prioritized. Access to these resources needs to be homogenous, meaning that the resource is available widely in the healthcare system. One lesson learned from the COVID-19 pandemic is strategic resources are uniquely heterogenous and immobile, which are not favorable traits for healthcare resources. For example, during the COVID-19 pandemic, there was a shortage of fundamental equipment needed in some regions initially hit with the novel virus. Ventilators and personal protective equipment were scarce in some hospitals, yet others had adequate supplies. It became very clear there was a gap between the need and the availability of resources globally (Ranney, Griffeth, & Jha, 2020)
The need for the mobility of resources is exceptional in times of natural disasters and pandemics Mobile Resources. Healthcare providers and resources need to be mobile to offer more quality care outcomes for a greater number of patients. The need for the mobility of resources is exceptional in times of natural disasters and pandemics. The temporary Executive Orders allowing healthcare providers to practice without state borders that typically inhibit them from swiftly mobilizing has increased the healthcare provider capacity in areas hit by the pandemic hardest (National Council of State Boards of Nursing, 2020). One might argue that this should be in place permanently, as all registered nurses and advanced practice nurses must be certified by national boards to practice (Benton et al., 2020). Having each state board of nursing manage licensure may be an expensive and outdated replication of services that all 50 states participate in currently. Another aspect of mobilizing healthcare resources was the quick adaption and implementation of telemedicine (Doshi et al., 2020). Adding long-term geographical and/or technological mobility to the human element of healthcare resources may significantly strengthen our healthcare system, as it did in the COVID-19 pandemic.
Another aspect of mobilizing healthcare resources was the quick adaption and implementation of telemedicine Modifying the EBP Model
The availability of resources plays a vast role in the care that nurses provide. Nurses have identified limited resources as a barrier to evidence-based nursing practice (Alatawi et al., 2020; Alqahtani et al., 2020). For example, Melnyk and Fineout-Overholt (2004) proposed within the context of caring that several aspects moderate clinical decision making. Research evidence and evidence-based theory; clinical expertise that includes evidence from patient assessment, internal evidence, and the use of healthcare resources; and patient preferences guide clinical decision making.
Nurses have identified limited resources as a barrier to evidence-based nursing practiceHowever, Melnyk and Fineout-Overholt's (2004) model, and most other, do not reflect the reality that resources greatly influence clinical decision making as a separate category in the model. A lack of resources has considerable consequences for the quality of patient care that nurses provide. It is clear that lack of healthcare resources is a barrier to implementing evidence-based practice, given the evidence of the early lack of PPE and ventilators during the COVID-19 pandemic (Troug et al., 2020). As healthcare organizations are not uniform in nature, the lack of resources as a barrier to EBP may be an ongoing state, especially in economically depressed and rural areas.
Nurses may want to inform practice with an evidence base but cannot due to the lack of resourcesNurses may want to inform practice with an evidence base but cannot due to the lack of resources. Within the original EBP models, there is typically no other option to make clinical decisions other than by best evidence. In reality, it does not matter what the best evidence is if healthcare resources that the evidence prescribes are not available. Perhaps future refinement of early EBP models needs to allow for contingency plans and alternative healthcare resources required to make clinical decisions.
Conclusion
Standards during health emergencies may be changed to respond to the imbalance between demands for care and resource allocationClinical decision making may shift from evidence-based to resource-based when healthcare resources are not available, affordable, or mobile, thus limiting patient and healthcare provider access. Standards during health emergencies may be changed to respond to the imbalance between demands for care and resource allocation. In reality, this occurs more often than not during times that the healthcare system is not in a crisis. For example, resource allocation is scarce at the individual level for the uninsured, homeless, and stateless individuals living in the United States. Additionally, and during disasters like the COVID-19 pandemic, the resource-based practice was evident, and practice guidelines became based on the availability of equipment.
A modified model that includes the availability of resources can offer a framework to direct clinical nursing practice in times of scarce resources...The EBP model discussed in this article, and others, do not provide guidance to address unavailability of resources (Melnyk & Fineout-Overholt, 2004). A modified model that includes the availability of resources can offer a framework to direct clinical nursing practice in times of scarce resources, whether a daily concern or an extreme global health crisis. Embracing implementation research may also help understand the role that resource availability plays in the observed gap between the best research and clinical practice (Zullig et al., 2020). The influence of resources in the process of implementing EBP, and the subsequent effect that the resource-based approach has upon patient outcomes, need further inquiry. To date, we do not know the individual and cumulative effect that resource-based decisions had upon patient outcomes and what risk it posed to the health of healthcare providers. Acknowledging the importance of the acquisition of healthcare resources may help guide the national and global healthcare agenda and also may allow the best evidence to guide practice more efficiently in the future.
Author
Jennifer Klimek Yingling, PhD, RN, FNP-BC, ANP-BC
Email: jaklimek@utica.edu
Dr. Jennifer Klimek Yingling is an Assistant Professor at Utica College. She is an upstate New York resident helping to strengthen the community through practice, academics, and research. Jennifer studied at Mohawk Valley Community College, the State University of New York Institute of Technology and received her Doctorate of Philosophy in Nursing from Rutgers University. A passionate caregiver and a patient advocate, she is a dual boarded Family and Adult Nurse Practitioner. Her more than two decades of nursing experience include experience in medical-surgical, emergency, forensic, occupational, and student health. Dr. Klimek Yingling currently practices clinically weekly, which brings real-life experiences to the classroom. Her research activities include work with breast cancer survivorship, horizontal violence, emergency department throughput, evidence-based practice barriers, and adverse childhood experiences.
References
Alatawi, M., Aljuhani, E., Alsufiany, F., Aleid, K., Rawah, R., Aljanabi, S., & Banakhar, M. (2020). Barriers of implementing evidence-based practice in nursing profession: A literature review. American Journal of Nursing Science, 9(1), 35-42. DOI: 10.11648/j.ajns.20200901.16
Alqahtani, N., Oh, K., Kitsantas, P., & Rodan, M. (2020). Nurses' evidence'based practice knowledge, attitudes, and implementation: A cross'sectional study. Journal of Clinical Nursing, 29(1-2), 274-283. DOI: 10.1111/jocn.15097
Aravind, M., & Chung, K. (2010). Evidence-based medicine and hospital reform: Tracing origins back to Florence Nightingale. Plastic and Reconstructive Surgery, 125(1), 403-409. DOI: 10.1097/PRS.0b013e3181c2bb89
Barney, J. (1991). Firm resources and sustained competitive advantage. Journal of Management, 17(1), 99-120. Retrieved from: https://josephmahoney.web.illinois.edu/BA545_Fall%202019/Barney%20(1991).pdf
Barney, J. (2001). Resource-based theories of competitive advantage: A ten-year retrospective on the resource based view. Journal of Management, 27(6),643-650. DOI: 10.1177/014920630102700602
Benton, D., Alexander, M., Fotsch, R., & Livanos, N. (2020). Lessons learned and insights gained: A regulatory analysis of the impacts, challenges, and responses to COVID-19. The Online Journal of Issues in Nursing, 25(3). DOI: 10.3912/OJIN.Vol25No03PPT51
Berardi, A., Perinelli, D., Merchant, H., Bisharat, L., Basheti, I., Bonacucina, Cespi, M., & Palmieri, G. (2020). Hand sanitisers amid CoViD-19: A critical review of alcohol-based products on the market and formulation approaches to respond to increasing demand. International journal of pharmaceutics, 584, 119431. DOI: 10.1016/j.ijpharm.2020.119431
Centers for Disease Control. (2020, April 17). Characteristics of Health Care Personnel with COVID-19 — United States. MMWR Morbidity and Mortality Weekly Report, 69(15), 477-481. DOI: 10.15585/mmwr.mm6915e6
Centers for Disease Control (2020, June 28). Strategies for optimizing supply of facemasks. Coronavirus Disease 2019 (COVID-2019). Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face-masks.html#crisis-capacity
Centers for Disease Control and Prevention. (2020, October 5). Clinical questions about COVID-19. Coronavirus Disease 2019 (COVID19). Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/hcp/faq.html
Chokshi, D., & Katz, M. (2020). Emerging lessons from COVID-19 response in New York City. Journal of American Medical Association Health Forum. DOI:10.1001/jamahealthforum.2020.0487
Doshi, A., Platt, Y., Dressen, J., Mathews, B., & Siy, J.(2020) Keep clam and log on: Telemedicine for COVID-19 pandemic response. Journal of Hospital Medicine, 15(5),302-304. DOI: 10.12788/jhm.3419
European Centre For Disease Prevention and Control. (2020, April 8). Rapid risk assessment: Coronavirus disease 2019 (COVID-19) pandemic: Increased transmission in the EU/EEA and the UK, 8th update. Retrieved from https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-coronavirus-disease-2019-covid-19-eueea-and-uk-eleventh
Garcia-Alamino, J. (2020). Human biases and the SARS-CoV-2 pandemic. Intensive and Critical Care Nursing, 58, 1-2. DOI: 10.1016/j.iccn.2020.102861
Goldstein, J. & McKinley, J. (2020, March 1). Coronavirus in NY: Manhattan woman is the first confirmed case in the state. New York Times. Retrieved from https://www.nytimes.com/2020/03/01/nyregion/new-york-coronvirus-confirmed.html
Harman, S. (2020). The danger of stories in global health. Lancet, 395(10226), 776-777. DOI: 10.1016/S0140-6736(20)30427-X
Helfat, C. & Peteref, M. (2003). The dynamic resource-based view: Capability lifecycles. Strategic Management Journal, 24(10), 997-1010. DOI: 10.1002/smj.332
Holshue, M., DeBolt, C., Lindquist, S., Lofy, K., Wiesman, J., Bruce, H., Spitters, C., Ericson, K., Wilkerson, S., Tural, A., Diaz, G., Cohn, A., Fox, L., Patel, A., Gerber, S., Kim, L., Tong, S., Lu, X., Lindstrom, S…Pillai, S. (2020). First case of 2019 Novel Coronavirus in the United States. New England Journal of Medicine, 382, 929-936. DOI: 10.1056/NEJMoa2001191
Kennedy, M. (2020). Life, interrupted. American Journal of Nursing, 120(5), 5-7. DOI: 10.1097/01.NAJ.0000662716.18546.d0
Kermode, M., Jolley, D., Langkham, B., Thomas, m., Holmes, W., & Gifford, S. (2005) Compliance with universal/standard precautions among health care workers in rural north India. American Journal of Infection Control, 33(1), 27-33. DOI: 10.1016/j.ajic.2004.07.014
Kilmarx, P., Clarke, K., Dietz, P., Hamel, M., Husain, F., McFadden, J., Park, B., Sugerman, D., Bresee, J., Mermin, J., McAuley, J., & Jambai, A. (2014, December 12) Ebola virus in healthcare workers-Sierra Leone, 2014. MMWR Morbidity and Mortality Weekly Reports, 63(49), 1168-1171. Retrieved from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6349a6.htm
Kim, J., Chung, Y., Jo, H., Lee, N., Kim, M., Woo, S., Park, S., Kim, J., Kim, H., & Han, M. (2020). Identification of Coronavirus isolated from a patient in Korea with COVID-19. Osong Public Health Research Perspective, 11(1), 3-7. DOI: 10.24171%2Fj.phrp.2020.11.1.02
Kulami, P., Prabhu, S., Kumar, S., & Ramraj, B. (2020). COVID-19-Infodemic overtaking pandemic? Time to disseminate facts over fear. Indian Journal of Community Health, 32(2), 264-268. Retrieved from: https://www.iapsmupuk.org/journal/index.php/IJCH/article/view/1455
Maslow, A. (1943). A theory of human motivation. Psychological Review, 50(4), 370-396.
Melnyk, B. & Fineout-Overholt, E. (2004). Making a case for evidence-based practice. In B. Melnyk & E. Fineout-Overholt (Eds.), Evidence based practice in nursing and healthcare (pp. 3-24). Lippincott, Williams & Wilkins.
Melnyk, B., & Fineout-Overholt, E. (2011). Evidence-based practice in nursing and healthcare. A guide to best practice. Lippincott.
Melnyk, B., Gallagher-Ford, L., Long, L., & Fineout-Overholt, E. (2014). The establishment of evidence-based practice competencies for practicing registered nurses and advanced practice nurses in real-world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes and costs. Worldviews on Evidence-Based Nursing, 11(1), 5-15. DOI: 10.1111/wvn.12021
Murphy, C. (2006) The 2003 SARS outbreak: Global challenges and innovative infection control measures. OJIN: The Online Journal of Issues in Nursing, 11(1), Manuscript 5. DOI: 10.3912/OJIN.Vol11No01Man05
National Council of State Boards of Nursing. (2020). State Response to COVID-19 (APRNs). National Council of State Boards of Nursing. Retrieved from: https://www.ncsbn.org/APRNState_COVID-19_Response_4_30.pdf
Ranney, M., Griffeth, V., & Jha, A. (2020). Critical supply shortages: The need for ventilators and personal protective equipment during COVID-19 pandemic. New England Journal of Medicine,382, e41. DOI: 10.1056/NEJMp2006141
Rebmann, T. & Carrico, R. (2017). Consistent infection prevention: Vital during routine and emerging infectious diseases care, OJIN: The Online Journal of Issues in Nursing, 22(1), Manuscript 1. DOI:10.3912/OJIN.Vol22No01Man01
Reinhart, R. (2020, January 6). Nurses continue to rate highest in honesty, ethics. Gallup. Retrieved from: https://news.gallup.com/poll/274673/nurses-continue-rate-highest-honesty-ethics.aspx
Remuzzi, A. & Remuzzi, G. (2020). COVID-19 and Italy: What next? The Lancet, 395, 1225-1228. DOI: 10.1016/S0140-6736(20)30627-9
Stevens, K. (2013). The impact of evidence-based practice in nursing and the next big ideas. The Online Journal of Issues in Nursing, 18(2), Manuscript 4. DOI: 10.3912/OJIN.Vol18No02Man04
Troug, R., Mitchell, C., & Daley, G. (2020). The toughest triage-Allocating ventilators in a pandemic. The New England Journal of Medicine, 382, 1973-1975. DOI: 10.1056/NEJMp2005689
World Health Organization [WHO]. (2014). Infection prevention and control of epidemic- and pandemic-prone acute respiratory infections in health care (xix, 133p.).World Health Organization. Retrieved from https://apps.who.int/iris/handle/10665/112656
World Health Organization. (2020, March 29). Modes of transmission of virus causing COVID-19: Implications for IPC precaution recommendations: Scientific brief. WHO. Retrieved from https://apps.who.int/iris/handle/10665/331616
World Health Organization. (2020). Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. WHO. Retrieved https://www.who.int/publications-detail/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages
Wu, Z. & McGoogan, J. (2020). Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19). Journal of the American Medical Association, 323(13), 1239-1242. DOI:10.1001/jama.2020.2648
Zhan, M., Qin, Y., Xue, X., & Zhu, S. (2020, June 4). Death from Covid-19 of 23 health care workers in China. The New England Journal of Medicine. DOI: 10.1056/NEJMc2005696
Zhang, Y., Chen, C., Zhu, S., Shu, C., Wang, D., Song, J., Song, Y., Zhen, W., Feng, Z., Wu, G., Xu, J., & Xu, W. (2020). Isolation of 2019-nCoV from a stool specimen of a laboratory-confirmed case of the coronavirus disease 2019 (COVID-19). China CDC Weekly, 2(8), 123-124. DOI: 10.46234/ccdcw2020.033
Zullig, L., Deschodt, M., & De Geest, S. (2020). Embracing implementation science: A paradigm shift for nursing research. Journal of Nursing Scholarship, 52(1), 3-5. DOI: 10.1111/jnu.12507

