Significant literature exists that focuses on cultural competence at the individual level, while cultural competence at the organizational level is rarely addressed. In addition, there is extensive literature separating and distinguishing cultural competence from cultural humility. The lack of intersectionality between individuals and organizations and the perceived division between cultural competence and cultural humility impedes the delivery of quality and equitable services. Part II of this two-part series on cultural competemility applies an intersectionality approach to the process of cultural competemility and offer strategies for nurses to actively challenge and address inequalities in their journey towards cultural competemility. In Part II the authors discuss the problem of silo thinking, after which they present an intersectionality perspective of cultural competemility, offer practice, educational, and administrative, and research applications, and conclude that a lens of intersectionality allows healthcare providers to consider new ways to overcome the division between individuals and organizations so as to promote delivery of quality and equitable healthcare services.
Key Words: Cultural competence, cultural diversity, cultural humility, transcultural nursing, healthcare equity, healthcare disparities, social justice, cultural awareness, cultural knowledge, cultural skill, cultural encounters, cultural desire, organizational cultural competence, individual cultural competence, intersectionality, cultural competemility
...healthcare organizations and healthcare professionals continue to ask: "What does it mean to be culturally competent and how do we get there?”Diversity in the United States (US) continues to increase, with all racial and ethnic minorities growing at a faster pace than whites from 2015 to 2016. Non-Hispanic whites remain the only segment of the U.S. population where deaths outpace births. By 2020, more than half of the U.S. children are expected to be part of a minority race or ethnic group. The minority population is projected to rise to 56 percent of the total population by 2060 (Colby & Ortman, 2014). Despite the development of several models of care and service delivery efforts to provide culturally and linguistically responsive services to our ever-growing, diverse world, healthcare organizations and healthcare professionals continue to ask: "What does it mean to be culturally competent and how do we get there?”
According to critical race theory, a cultural competence perspective fails to acknowledge the socio-structural factors and institutional processes that contribute to social injustices as a consequence of cultural differences when compared to the dominant society (Abrams & Moio, 2009). An ongoing debate in the literature argues that a focus on developing a culturally competent healthcare workforce, though well intended, has resulted in an unintentional over-emphasis on shared group characteristics and the undervaluing of unique differences of individuals; yet the debate fails to address the privilege and power imbalances between providers and the clients they serve, as well as between healthcare organizations and the communities they serve (Campinha-Bacote, 2018).
A significant amount of literature focuses on cultural competence at the individual level, with organizational cultural competence playing a secondary role.A significant amount of literature focuses on cultural competence at the individual level, with organizational cultural competence playing a secondary role. In addition, there is extensive literature separating and distinguishing cultural competence from cultural humility. This lack of interface between individuals and organizations and the perceived division between cultural competence and cultural humility continues to impede the delivery of quality and equitable services. In response to this gap, Campinha-Bacote suggests, in this article, a new concept, ‘cultural competemility’ (Campinha-Bacote, 2018). Using an intersectionality approach to cultural competemility, this article offers strategies that nurses and other healthcare professionals (HCPs) in practice, education, administrative, or research positions can use as individuals and within organizations to actively challenge and address inequalities. These actions are essential in the journey towards cultural competemility.
Cultural competence has commanded reputable attention since its introduction in cross-cultural discourse (Campinha-Bacote, 2018 [Part I of this 2-part series]; Danso, 2016; Gallegos, Tindall, & Gallegos, 2008). Danso describes a “smorgasbord” of definitions and conceptualizations which has created intense debate around the construct and questions its ability to address organizational problems. This cynicism has led to calls to replace cultural competence with the concept of cultural humility, which is often seen as an alternative approach to that of cultural competency (Fisher-Borne, Cain & Martin, 2015). Other authors maintain that cultural humility may complement, rather than replace, cultural competence (Alsharif, 2012; Yancu & Farmer, 2017).
Individuals and organizations must engage in the process of becoming culturally competent, while concurrently engaging in the process of being culturally humble.Cultural humility is defined as lifelong process focusing on self-reflection and personal critique (Tervalon and Murray-Garcia, 1998). Campinha-Bacote (2018) has suggested a synergistic relationship between cultural competence and cultural humility resulting in a combined effect greater than the sum of their separate effects. Campinha-Bacote refers to this synergistic relationship as the process of cultural competemility. Cultural competemility is the synergistic process in which cultural humility permeates each of the five components of cultural competence (cultural awareness, cultural knowledge, cultural skill, cultural desire, and cultural encounters). Campinha-Bacote asserts that competemility can be viewed as simultaneously being both a process of becoming and the paradoxical process of being. Individuals and organizations must engage in the process of becoming culturally competent, while concurrently engaging in the process of being culturally humble.
Addressing the Problem: Silo Thinking
Cross, Bazron, Dennis, and Isaac‘s (1989) landmark definition of cultural competence states that: “cultural competence is a set of congruent behaviors, attitudes, and policies that come together in a system, agency or among professionals and enable that system, agency or those professions to work effectively in cross-cultural situations” (p.13). These authors contend that there are five vital elements that contribute to a system's ability to become more culturally competent. The system should: (a) value diversity, (b) have the capacity for cultural self-assessment; (c) be conscious of the dynamics inherent when cultures interact; (d) institutionalize cultural knowledge; and (e) develop programs and services that reflect an understanding of diversity between and within cultures. These five elements must be demonstrated at every level of the service-delivery system and should be reflected in attitudes, structures, policies, and service at both the organizational and individual level.
Competemility addresses the importance of merging cultural competence and cultural humility. Cross et al. (1989) referred to individual and institutional perspectives that range from cultural destructiveness to cultural proficiency. While Cross et al. include both the individual and organization in their definition, strategies for achieving cultural competence have continued to separate cultural competence into two silos: individual and organizational. Furthermore, there exists a significant amount of literature focusing on cultural competence and cultural humility at the individual level, whereas cultural competence and cultural humility are secondary at the organizational level. Competemility addresses the importance of merging cultural competence and cultural humility.
Nursing organizations have called for action related to cultural competence in healthcare delivery. In 1986 the American Nurses Association (ANA) issued its first position statement to strengthen cultural diversity programs in nursing (ANA, 1986). Lowe and Archibald (2009) explored cultural diversity progress in nursing and asserted: “Despite the intentions and the efforts made by nursing, progress in the area of cultural diversity has been slow, sporadic, and overdue” (p. 17). In 2010, the Expert Panel for Global Nursing and Health of the American Academy of Nursing (AAN) and members of the Transcultural Nursing Society (TCNS) developed a set of standards for cultural competence in nursing practice (Douglas et al., 2014). The project aim was to define standards for universal application by nurses around the world in the areas of clinical practice, research, education, and administration, especially by nurses involved in direct patient care. Additionally, the guidelines were designed to be adapted to the unique needs of users and be amenable to the sociocultural context and healthcare delivery system where users practice. ANA continues its quest to strengthen cultural diversity in nursing practice, as demonstrated by Standard 8 of the third edition of the Nursing Scope and Standards of Practice which highlights the need for registered nurses to practice in a manner that is congruent with cultural diversity and inclusion principles (ANA, 2015).
Similarly, healthcare and governmental organizations have developed and implemented policies to address issues surrounding the need for cultural competence in healthcare delivery. The Office of Minority Health (OMH) at the U.S. Department of Health and Human Services developed the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care (U.S. Department of Health and Human Services, 2013). The CLAS standards are intended to advance health equity, improve quality, and help eliminate healthcare disparities. As such, the CLAS standards established a blueprint for health and healthcare organizations to provide effective, equitable, understandable, and respectful quality care and services that are responsive to diverse cultural health beliefs and practices, preferred languages, health literacy, and other communication needs.
The Joint Commission has also recognized the importance of culturally competent care, and since 2004 has been studying how healthcare organizations address challenges of providing healthcare to diverse populations. In 2014, The Joint Commission (2014) collaborated with OMH to develop a document comparing the Office of Minority Health’s National CLAS Standards to The Joint Commission’s 2015 Standards for the Ambulatory Health Care Accreditation Program. Additionally, the National Committee for Quality Assurance (2016) published a guide for implementing the CLAS Standards. This guide included a toolkit designed for use by healthcare organizations and their health plans; provider practices and hospitals; states and communities that have decided to improve health equity and implement the National CLAS Standards.
The literature focus is almost exclusively on individual level changes and fails to adequately communicate how individual and organizational changes are interconnected.Despite all the efforts and accomplishments of these nursing, governmental, and healthcare organizations, the gap continues between the intersection of cultural competemility at the individual and organizational level. The literature focus is almost exclusively on individual level changes and fails to adequately communicate how individual and organizational changes are interconnected (Fisher-Borne, Cain, and Martin, 2015). Silo thinking and the lack of interconnection between individuals and organizations impedes the journey of providing quality and equable services to culturally diverse populations. Individuals and organizations do not exist separately from each other but are complexly interwoven. They are each at various levels of cultural awareness, cultural encounters, cultural desire, cultural knowledge, and cultural skills, which affect their ability to effectively render culturally responsive care to culturally diverse patients.
Individual and Organizational Cultural Competemility: An Intersectionality Perspective
During the late 1980s and early 1990s, the concept of intersectionality evolved through both scholarly endeavors and activist engagement.Intersectionality refers to the interaction between gender, race, and other categories of difference in individual lives, social practices, institutional arrangements, and cultural ideologies, and the outcomes of these interactions in terms of power (K. Davis, 2008, p.68). During the late 1980s and early 1990s, the concept of intersectionality evolved through both scholarly endeavors and activist engagement (Caiola, Docherty, Ralf, & Barroso, 2014). Crenshaw (1989), a feminist scholar, coined the term “intersectionality.” Crenshaw’s intent was to use the term to address how the experiences and struggles of women of color were not adequately addressed by either feminist or anti-racist discourse. Crenshaw encouraged feminist theorists to consider gender and race and show how they interacted to shape the experience of Black women. American scholar bell hooks (as cited in Lowens, 2018), who prefers lowercase for her name, powerfully examined the varied perceptions of Black women and the development of feminist identities and eloquently stated: "For people like me, what is important and vital is to keep that education for critical consciousness around intersectionalities, so that people are able to not focus on one thing and blame one group, but be able to look holistically at the way intersectionality informs all of us: whiteness, gender, sexual preferences, etc. Only then can we have a realistic handle on the political and cultural world we live within” (cited in Lowens, 2018, paragraph 32).
The sociology of science (Clarke & McCall, 2013; K. Davis, 2008; & Merton, 1973) has examined the relationship between theories and their audience and how a specific theory or perspective might persuade an audience to view some aspect of the world. K. Davis (2008) suggested that individuals must be understood as whole and complex. Intersectionality purports that people simultaneously occupy multiple positionalities within the socio-cultural-political and structural fabric of society (Hernandez & McDowell, 2010; Muntinga, Krajenbrink, Peerdeman, Croiset & Verdonk, 2016; Ortega & Faller, 2011). Intersectionality challenges the concept of culture as static and disrupts the idea of social identities as operating in isolation (Fisher-Borne, Cain, and Martin, 2015). Positionality refers to one's social location and worldview which influences how one responds to power differentials in various contexts. Positionality is important for social work and other healthcare providers for it impacts how one approaches work with clients, community engagement, and policy-making (Klawetter, 2016).
This understanding cannot be achieved unless both parties are willing to be open and work together.The child welfare literature also argues that intersecting group memberships influence people’s expectations, quality of life, capacities, and even their life chances (Ortega & Faller, 2011). This perspective allows healthcare professionals and organizations to assess an individual’s multiple identities and contemplate how social experiences influence one’s worldview. Moreover, this perspective releases the provider from being an expert. The provider is in a learning mode rather than feeling as if he/she must maintain power and control (Tervalon & Murray-Garcia, 1998). Thus, the provider becomes a learner who supports the client as a true partner in the therapeutic alliance. Healthcare professionals and organizations must begin to incorporate an intersectional understanding and analysis of the whole person, with an emphasis on power and privilege differences in relationships. This understanding cannot be achieved unless both parties are willing to be open and work together.
It is from this viewpoint of intersectionality that we can begin the process of closing the gap between healthcare professionals’ and healthcare organizations’ separate attempts at cultural competemility.Intersectionality continues to be an emerging concept; and over the past two decades scholars have debated its potential applications. Roberts and Jesudason (2013) assert that the merit of intersectional analysis is not confined to understanding individual experiences or the ways in which systems of power intersect in individual lives. These authors maintain that intersectionality does not need to apply only to the ways by which identity categories or systems of power intersect in individual lives, nor apply solely to differences within or between identity-based groups. Intersectionality can also be a powerful tool to build more effective alliances between movements so as to make them more effective at organizing for social change (Roberts & Jesudason, 2013, p. 314). These authors further add that using intersectionality for cross movement mobilization reveals that, contrary to criticism for being divisive, attention to intersecting identities has the potential to create cohesion. It is from this viewpoint of intersectionality that we can begin the process of closing the gap between healthcare professionals’ and healthcare organizations’ separate attempts at cultural competemility. An intersectional perspective enables discussion and collaboration among HCPs and organizations that illuminates their similarities and common values in striving towards cultural competemility.
An Intersectionality Approach to Cultural Competemility is a conceptual framework derived from Campinha-Bacote’s models of cultural competence (Campinha-Bacote, 2011, 2013). This approach to healthcare delivery defines an intersectionality approach to cultural competemility as the interconnected process in which healthcare professionals and healthcare organizations work together and continually strive to effectively work within the cultural context of a client, such as a family, an individual or a community (Campinha-Bacote, 2018). In this intersectionality approach to cultural competemility, cultural humility infuses and permeates each of the five constructs of cultural competence (i.e., cultural awareness, cultural knowledge, cultural skill, cultural encounters, and cultural desire) from both an organizational and individual perspective. The figure below depicts the intersectionality approach to the process of cultural competemility.
Figure. An Intersectionality Approach to the Process of Cultural Competemility
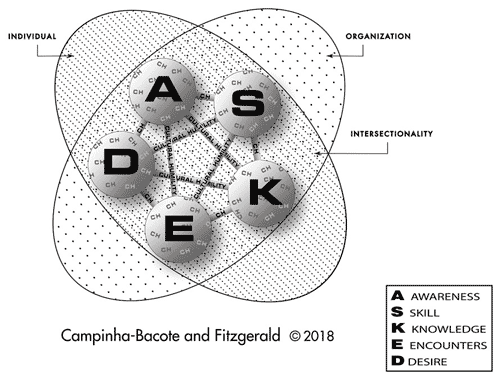
Cultural awareness is the process of conducting a self-examination and critical reflection of one’s own biases towards other cultures and the in-depth exploration of one’s cultural (organizational and individual) background. Cultural awareness also involves being aware of the existence of documented racism and other “isms” in healthcare delivery and acknowledging the privilege and power inherent in one’s position. Cultural knowledge is defined as the process in which the healthcare professional and the healthcare organization interconnect to seek and obtain a sound educational base about culturally diverse groups. Cultural skill is the ability to conduct a cultural assessment to collect relevant cultural data regarding one’s organization and the clients and employees they serve. Cultural encounters encourage healthcare professionals and organizations to directly engage in face-to-face interactions and other types of encounters with clients and employees from culturally diverse backgrounds to modify existing beliefs about a cultural group and to prevent possible stereotyping. Cultural desire is the motivation needed to seek cultural encounters and further the process of becoming culturally aware, culturally knowledgeable, and culturally skillful. Organizations and individuals cannot engage in cultural awareness, cultural encounters, cultural knowledge, cultural skill, and cultural knowledge without operating from a cultural humility lens that is continuously being infused throughout each one of these five constructs (See Figure).
Practice, Education, Administration and Research Applications
Structured and intentional interventions, in which both the organization and healthcare professional are jointly held accountable and responsible, are important...in the journey towards an intersectionality approach to cultural competemility.Structured and intentional interventions, in which both the organization and healthcare professional are jointly held accountable and responsible, are important to develop the needed practice, educational, research, and administrative changes in the journey towards an intersectionality approach to cultural competemility. As stated by Fisher-Borne, Cain, and Martin (2015), accountability differs significantly from a sense of mastery, for it implies a commitment to self-reflection that is active and responsible. These authors add that healthcare organizations must critically reflect on the following issues: a) policies and procedures that actively address inequalities; b) existing structures that encourage action to address inequalities; c) current training and professional development opportunities addressing inequalities and inspiring active self-reflection about power and privilege; d) commitment to a diverse staff and leadership; and e) the monitoring, hiring, recruitment, and retention of diverse staff (p. 176). These questions and critical reflections must be done in concert with healthcare professionals addressing questions and reflecting on their initial reactions to culturally diverse clients; how much they value input from their clients; and how they extend their responsibility beyond individual clients and advocate for changes in local, state, and national policies and practices (Fisher-Borne, Cain, and Martin, 2015, p. 176).
Application in the Practice Setting
Individual members of the leadership team must continuously assess the organization’s environment, policies, procedures, knowledge and skills related to individual worker practices.For clinical practice, Standard 8 provides opportunities for an approach to intersectionality between individuals and organizations (ANA Scope and Standards of Practice, 3rd Edition, 2015). RNs prepared at the graduate level are called to advance organizational policies, programs, services, and practice that reflect respect, equity and values for diversity and inclusion (ANA Scope and Standards of Practice, 3rd Edition, 2015). In the Guidelines for Implementing Culturally Competent Care (Douglas et al., 2014), Guideline 6 focuses on Cultural Competence in Health Care Organizations and Systems and states: “Health care organizations should provide the structure and resources necessary to evaluate and meet the cultural and language needs of their diverse clients” (p. 113). The organization’s leadership is responsible for meeting this guideline. Furthermore, individual members of the organization must participate in strategic planning to develop and maintain the infrastructure that supports culturally congruent and compassionate care to ensure it is reflected in the organization’s mission, vision, and values. Individual members of the leadership team must continuously assess the organization’s environment, policies, procedures, knowledge and skills related to individual worker practices (Ortega & Faller, 2011).
Ortega & Faller (2011) have identified four skills that help healthcare professionals and organizations understand the client’s world view: active listening, reflecting, reserving judgment, and placing oneself in the context of the client’s world. Similarly, Chang, Simon, and Dong (2012) propose the model QIAN (self-questioning, immersion, active listening, and negotiation). Their model is applicable to cultural encounters with employees, patients, families, the healthcare system and the community at large. Chang et al. (2012) suggest that one asks the following questions: “How would I like to be treated today if I were in my patient’s shoes? What could I do to foster respect in our exchange?” (p. 274). Hook, Davis, Owen, Worthington, and Utsey (2013) indicate that "therapists should make hypotheses rather than jump to premature conclusions when working with clients from diverse backgrounds” (p. 354).
An intersectionality approach to cultural competemility can also help guide engagement in activities such as advocacy, outreach, and prevention programs that address social justice issues. Cultural competemility is a part of the much larger picture of social justice (Anderson et al., 2009). Cultural competemility and social justice are interconnected through their shared purpose of removing institutional, systemic, and social oppression, thus ensuring equity for all individuals (Constantine & Sue, 2006). Anderson et al. (2009) contend that nurses at the everyday level of practice, research, administration, and education need to recognize that social justice is not merely an abstract, macro-level concept. These authors add that “nurses at the everyday level of practice, researchers, and educators need to understand that social justice is not just an abstract macrolevel concept; the views that they hold about patients and their everyday interactions with patients and with one another can either contribute to socially just actions or reproduce social injustices" (p. 290). Furthermore, they assert that as social justice advocates, healthcare professionals can facilitate consciousness-raising activities through presentations or workshops; follow-up group discussion would explore actions to reach vulnerable and underserved populations at the individual and organizational levels.
Application in the Educational Setting
Faculty members and organizational leaders can demonstrate cultural competemility by exhibiting an egoless attitude and narratives of examples where they failed.From an educational perspective, intentional class discussions about privilege must occur at the onset of courses, led by faculty and other educators who are culturally knowledgeable and comfortable in such roles (Ross, 2010). Faculty members and organizational leaders can demonstrate cultural competemility by exhibiting an egoless attitude and narratives of examples where they failed (Alsharif, 2012). Educational efforts must address both intrapersonal and interpersonal components (D.E. Davis, Worthington, & Hook, 2010). Benner (2016) encourages students to remain curious and stay open and responsive as they actively listen. These skills can enlarge the student’s understanding of healthcare barriers. In addition, Benner urges faculty to have students compare and contrast the experience of listening with a “judging eye” and “clinical eye” versus a curious, respectful, attentive and open-eyed approach (cited in Martinsen, 2006, p.97). Scaffolding theory (Bruner, 1966; Vygotsky, 1978) identifies the importance of providing students with enough support in the initial stages of learning a new subject. Vygotsky (1978) believed that when a student encounters a task too difficult to master independently, a knowledgeable person providing guidance and encouragement will give the student enough of a 'boost’ to achieve the task.
Cultural competemility is a lifelong process.Cultural competemility is a lifelong process. Thus, it may prove fruitful to scaffold the teaching of concepts, such as cultural competence, cultural humility and competemility from undergraduate through graduate nursing education, as well as during the professional development of the nurse throughout his/her career. Paparella-Pitzel, Eubanks, and Kaplan (2016) propose a framework for mapping cultural humility course content into a coherent educational process that allows for planning educational experiences and assessment. Key components of their framework include creating a culturally safe teaching environment and incorporating the constructs of cultural awareness, cultural skill, cultural encounter, cultural knowledge, and cultural desire into educational experiences (Campinha-Bacote, 2018).
...engaging in conversations confronting one’s biases can be challenging to students.Mastel-Smith and Yarbrough (2017) report that a review of the literature suggested that reflection is a necessary part of developing cultural humility. Reflexivity is a skill that requires teaching and should be viewed as an ongoing learning process throughout one’s career (Schuessler, Wilder, & Byrd, 2012). While reflection discussions are essential, engaging in conversations confronting one’s biases can be challenging to students. Reflexivity and reflective writing must be done in a safe learning environment. It is also important for faculty and organizational leaders to be encouraged to practice reflexivity. Participation in a learning community where one is supported in a safe environment can provide opportunities to grow professionally.
Chávez and Longerbeam (2018) have provided strategies to engage in reflexive cultural learning. These authors contend that professionals from some cultural origins may experience trauma associated with negotiating educational systems and that cross-cultural discussions may trigger emotional flashbacks and distress (e.g., ‘trauma triggers’). Strategies to overcome such triggers include engaging strengths, such as generosity, openness, courage, and persistence, to offer comfort and support to manage the intensity of reflexive cultural learning. These authors advise that one must be willing to be uncomfortable, draw on cultural strengths from each individual, remain intensely present, ask one another directly and respectfully about differences, encourage risk taking and mistake making, and engage one another’s combined strengths to get through trauma triggers. From an intersectionality approach, both faculty and administrators must be convinced that a faculty learning community provides excellent learning, development, and commitment to cultural competemility.
The same processes expected to affect change in healthcare professionals should simultaneously exist in the organization whose agenda is to develop cultural competemility through educational programs (Tervalon & Murray-Garcia, 1998). Tervalon and Murray-Garcia (1998) recommend self-reflection and self-critique questions through the use of the following questions:
- What is the demographic profile of the faculty?
- Is the faculty composition inclusive of members from diverse cultural, racial, ethnic, and sexual orientation backgrounds?
- Are faculty members required to undergo multicultural training as are the youngest students of the profession?
- Does the institutional ethos support inclusion and respectful, substantive discussions of the clinical implications of difference?
- What institutional processes contradict or obstruct the lessons taught and learned in a multicultural curriculum (e.g., if it is taught that practitioners should not use children or other family members as translators, does the institution provide an accessible alternative)?
- What is the history of the health care institution with the surrounding community?
- What present model of relationship between the institution and the community is seen by trainees? (p. 122)
Cultural desire is the fuel necessary to draw one into a personal journey toward cultural competemility.Cultural desire must be cultivated during the educational process of cultural competemility (Campinha-Bacote, 2008). Cultural desire is the fuel necessary to draw one into a personal journey toward cultural competemility. Moore et al. (2017) purport that the objective of cultural competency education is not to achieve a standardized level of cultural competence, but rather to impart a desire to increase one’s own cultural awareness, knowledge, and skills. These authors argue that comprehensive cultural competency education in healthcare must be intentional, highlight the need for a dedicated, course-specific approach, instill a desire to continually cultivate cultural competence, and be pervasive.
Application in Administrative Settings
Administratively, cultural assessment of the organizational environment, policies, procedures, knowledge, and skills connected to healthcare workers’ practices is essential (Ortega & Faller, 2011; Tervalon, Murray-Garcia, 1998). Intentional strategies at the leadership level identify ways in which an intersectionality perspective of cultural competemility is embraced and promoted. Equally, leadership efforts must be made to expose and address barriers and obstacles within the organization that inhibit workers from serving the needs of patients and communities. Upon completion of the assessment, leaders must develop plans, including training and professional development opportunities, and identify organizational support to address power imbalances and develop authentic partnerships (Hinkler, 2012). In addition, leadership must engage in strategic planning that allows the organization to be accountable for change.
The Society of Hospital Medicine has developed the 5 Rs of Cultural Humility, a model that can be adapted to help healthcare professionals and administrators learn cultural competemility (Ansari, 2017). The 5Rs include: reflection, respect, regard, relevance, and resiliency. Their model evolved from a cultural humility work group that was part of a practice management committee. They determined that unconscious bias had to be addressed before providers and administrators could become more openminded and that everyone had to become comfortable with feelings of discomfort for the biases to manifest themselves.
Application in Research Settings
...minimal attention has been directed to researchers regarding the conduct of culturally competent research.Much attention has been given to preparing healthcare professionals to render culturally competent care at the bedside. Yeager and Bauer-Wu (2013) maintain that minimal attention has been directed to researchers regarding the conduct of culturally competent research. An intersectionality approach to cultural competemility encourages researchers, at both individual and organizational levels, to explore and implement more culturally responsive projects to address health disparities. The researcher can begin with cultural awareness, including an in-depth examination of his/her own biases related to cultural differences. The researcher is also encouraged to explore personal beliefs by placing oneself within the experience and considering the meaning to the study participant and the relationship.
Yeager and Bauer-Wu stress the importance of understanding historical influences on vulnerable populations as well as the present existence of health disparities and lack of access to quality healthcare (2013, p. 254), which can impact how research participants view research. These authors call attention to the need to recognize and address the power imbalance between the researcher and the participant and to be mindful of this imbalance through all stages of the research process. Yeager and Bauer-Wu also encourage researchers to reflect on their own values and biases as a way to help investigators implement meaningful and ethical projects that better address health disparities.
...historically, healthcare research was conducted in the community without the community’s active engagement in framing the research phases.Research applications from an intersectionality approach to cultural competemility also involve an understanding of the cultural and historical factors at play and involving minority groups in creating solutions. To build meaningful relationships with the participant, the researcher first explores the values, beliefs, and biases of the research participant specific to healthcare and research participation (Willis & Allen, 2011; Yeager & Bauer-Wu, 2013). The Tuskegee Syphilis Experiment (Jones, 1993), cited as the most infamous biomedical research study in U.S. history, is an unfortunate landmark example that illustrates the worst of research with vulnerable populations. Chang et al. (2012) remind us that historically, healthcare research was conducted in the community without the community’s active engagement in framing the research phases. Thus, today community groups may have had a negative experience and not trust researchers or the process of research.
Community-based participatory research (CBPR) is a culturally conscious and responsive approach in the researcher’s journey towards cultural competemility. Ross (2010) purports that the use of community-based participatory research is a preferred framework for teaching graduate students and organizations to be culturally humble when conducting research about environmental health and social justice issues within the community. The principles of CBPR include promotion of 'equitable engagement' throughout the research process (Cacari-Stone, Wallerstein, Garcia, & Minkler, 2014, p.1615). In this model, community partners are engaged in problem definition; data collection and analysis; and dissemination and use of findings to help effect change (Israel, Enf, Schulz, & Parker, 2013; Minkler & Wallerstein, 2008; Ross, 2010).
Cacari-Stone et al. (2014) noted the importance of leveraging research to promote health policy and have designed a conceptual model to demonstrate how CBPR can influence health policy to eliminate racial and ethnic health inequities. Their conceptual model stresses the importance of contexts such as history, trust, capacity and readiness. They propose that CBPR processes can be used to influence policy formulation, implementation and evaluation/modification to enable policy change that may improve health outcomes. Cacari-Stone et al. (2014) assert that the likelihood for evidence to be used in policymaking increases if the research is perceived as useful. These authors add that sustained political participation is required and encourage the use of community-academic research networks to alter public opinion and build awareness of the impact of problems in historically marginalized communities. There is also a need for longitudinal studies of community-academic engagement to identify facilitators and barriers to eliciting health equity and social justice through policy change.
Conclusion
Using the lens of intersectionality allows HCPs to consider new ways to overcome the division between individuals and organizations when delivering quality and equitable services.Drawing from our experiences in healthcare settings, we have offered the framework of intersectionality as it relates to cultural competemility. We have also focused on the interaction between gender, race, and other categories of difference in individual lives, social practices, institutional arrangements, cultural ideologies, and on the outcomes of these interactions, in terms of power. Using the lens of intersectionality allows HCPs to consider new ways to overcome the division between individuals and organizations when delivering quality and equitable services. We believe this framework has the potential to produce mutually beneficial collaboration across fields of study and among the healthcare disciplines, thus generating more inclusive solutions to the problems of inequality in healthcare.
We have also provided strategies for using an intersectionality approach to the process of cultural competemility (Campinha-Bacote, 2018) that nurses and other HCPs can use in their practice, educational, research or administrative positions as they actively challenge and address inequalities in the journey toward cultural competemility. Hooks has written, “Dare to look at the intersectionalities. Dare to be holistic….” (Cited in Lowens, 2018, paragraph 34). We encourage you to consider intersectionality in your journey towards cultural competemility.
Authors
Elizabeth Fitzgerald, EdD, APRN-CNS, PMHCNS-BC, CTN-B
Email: fitzgerald.118@osu.edu
Dr. Elizabeth Fitzgerald is an Associate Professor of Clinical Nursing at the Ohio State University and the co-director of the Columbus-Athens Schweitzer Fellowship Program. She is certified by the American Nurses Credential Center as a clinical nurse specialist in child and adolescent psychiatric/mental health nursing. As a Transcultural Nurse Scholar and a Certified Teacher of English as a Foreign Language, she has decades of expertise and experience in community engagement with vulnerable populations to improve access to care and health literacy, and to reduce health disparities in the United States as well as in global settings. She has extensive teaching experience with diverse nursing students in undergraduate and graduate nursing programs at multiple universities.
Josepha Campinha-Bacote, PhD, MAR, PMHCNS-BC, CTN-A, FAAN
Email: meddir@aol.com
Dr. Campinha-Bacote is President of Transcultural C.A.R.E. Associates. She has published extensively on issues concerning transcultural healthcare. Dr. Campinha-Bacote is certified by the Transcultural Nursing Society (TCNS) as an Advanced Certified Transcultural Nurse and has been inducted into the TCNS as a Transcultural Nursing Scholar. She been the recipient of several national and international honors and awards, including the Transcultural Nursing Society Leadership Award, the Ethnic/Racial Minority Fellowship Award from the National Institute of Mental Health, the Lifetime Achievement Diversity Award from the University of Rhode Island, and the Minority Health Knowledge Award from the Ohio Commission on Minority. Dr. Campinha-Bacote, a Fellow of the American Academy of Nursing, has served on the National Advisory Committee to the United States Department of Health and Human Services Office of Minority Health to develop standards for Culturally and Linguistically Appropriate Services in Health Care.
References
Abrams, L. S., & Moio, J. A. (2009). Critical race theory and the cultural competence dilemma in social work education. Journal of Social Work Education, 45(2), 245-259. https://doi.org/10.5175/JSWE.2009.200700109
Alsharif, N. Z. (2012). Cultural humility and interprofessional education and practice: A winning combination. American Journal of Pharmaceutical Education, 76(7), 120. https://dx.doi.org/10.5688%2Fajpe767120
American Nurses Association. (1986). Cultural diversity in nursing. Silver Spring, MD: American Nurses Association House of Delegates.
American Nurses Association. (2015). Nursing: Scope and standards of practice (3rd ed.). Silver Spring, MD: American Nurses Association.
Anderson, M., Rodney, P., Reimer-Kirkham, S., Browne, A., Khan, K. & Lynam, J. (2009). Inequities in health and healthcare viewed through the ethical lens of critical social justice: Contextual knowledge for the global priorities ahead. Advances in Nursing Science, 32(4), 282-294. doi: 10.1097/ANS.0b013e3181bd6955
Ansari, A. (April 25, 2017). Battling biases with the 5Rs of cultural humility. The Hospitalist. Retrieved from https://www.the-hospitalist.org/hospitalist/article/136529/leadership-training/battling-biases-5-rs-cultural-humility
Benner, P. (2016). Cultural humility: Gaining first-person experience and empathy for the health and life impact of living in poverty. Educating Nurses. Retrieved from https://www.educatingnurses.com/cultural-humility-gaining-first-person-experience-and-empathy-for-the-health-and-life-impact-of-living-in-poverty/
Bruner, J. S. (1966). Toward a theory of instruction. Cambridge, MA: Belkapp Press.
Cacari-Stone, L., Wallerstein, N., Garcia, A., & Minkler, M. (2014). The promise of community-based participatory research for health equity: A conceptual model for bridging evidence with policy. American Journal of Public Health, 104(9), 116-123. doi: 10.2105/AJPH.2014.301961
Caiola, C., Docherty, S., Relf, M., & Barroso, J. (2014). Using an intersectional approach to study the impact of social determinants of health for African-American mothers living with HIV. Advances in Nursing Science, 37(4), 287–298.
Campinha-Bacote, J. (2008). Cultural Desire: ‘Caught’ or ‘taught?’ Contemporary Nurse, 28(1-2), 141-148. doi: 10.5172/conu.673.28.1-2.141
Campinha-Bacote, J. (2011). Coming to know cultural competence: An evolutionary process. International Journal for Human Caring, 15(3), 42-48. doi: 10.20467/1091-5710.15.3.42
Campinha-Bacote. J. (2013). A biblically based model of cultural competence in the delivery of healthcare services: Seeing “Imago Dei” (2nd ed.). Cincinnati, OH: Transcultural C.A.R.E. Associates.
Campinha-Bacote, J. (2018). Cultural competemility: A paradigm shift in the cultural competence versus cultural humility debate - Part I. OJIN: The Online Journal of Issues in Nursing, 24(1). doi: 10.3912/OJIN.Vol24No01PPT20
Chang, E., Simon, M., & Dong, X. (2012). Integrating cultural humility into health care professional education and training. Advances Health Science Education, 17(2), 269-78. doi: 10.1007/s10459-010-9264-1
Chávez, A., & Longerbeam, S. (2018). Reflexivity in cross-cultural collaboration. Diversity and Democracy, 21(1). https://www.aacu.org/diversitydemocracy/2018/winter/chavez
Clarke, A.Y., & McCall, L. (2013). Intersectionality and social explanation in social science research. DuBois Review: Social Science Research on Race, 10(2), 349-363. https://doi.org/10.1017/S1742058X13000325
Colby, S. L., & Ortman, J. M. (2014). Projections of the size and composition of the U.S. population: 2014 to 2060. Washington, DC: U.S. Census Bureau. Retrieved from https://census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf
Constantine, M., & Sue, D. (Eds.). (2006). Addressing racism: Facilitating cultural competence in mental health and educational settings. New York, NY: John Wiley.
Crenshaw, K. (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989(1), 139-167. Retrieved from https://chicagounbound.uchicago.edu/cgi/viewcontent.cgi?article=1052&context=uclf
Cross, T., Bazron, B., Dennis, K., & Isaac, M. (1989). Toward a culturally competent system of care. Washington, DC: CASSP Technical Assistance Center at Georgetown University Child Development Center.
Danso, R. (2016). Cultural competence and cultural humility: A critical reflection on key cultural diversity concepts. Journal of Social Work. 18(4), 410-430. https://doi.org/10.1177/1468017316654341
Davis, D. E., Worthington, E. L., & Hook, J. N. (2010). Humility: Review of measurement strategies and conceptualization as personality judgment. Journal of Positive Psychology, 5(4), 243-52. https://doi.org/10.1080/17439761003791672
Davis, K. (2008). Intersectionality as buzzword. A sociology of science perspective on what makes a feminist theory successful. Feminist Theory, 9(1), 67-85. https://doi.org/10.1177/1464700108086364
Douglas, M., Rosenkoetter, M., Pacquiao, D., Callister, L., Hattar-Pollara, M., Lauderdale,…Purnell, L. (2014). Guidelines for implementing culturally competent nursing care. Journal of Transcultural Nursing, 25(2), 109-121. https://doi.org/10.1177/1043659614520998
Fisher-Borne, M, Cain, J. M., & Martin, S. L. (2015). From mastery to accountability: Cultural humility as an alternative to cultural competence. Social Work Education, 34(2), 165-181. http://dx.doi.org/10.1080/02615479.2014.977244
Gallegos, J., Tindall, C., & Gallegos, S. (2008). The need for advancement in the conceptualization of cultural competence. Advances in Social Work, 9(1), 51-62.
Hernandez, P., & McDowell, T. (2010). Intersectionality, power, and relational safety in context: Key concepts in clinical supervision. Training and Education in Professional Psychology, 4(1), 29-35. http://dx.doi.org/10.1037/a0017064
Hinkler, M. (2012). Community organizing and community building for health and welfare (3rd ed.). New Brunswick, NJ: Rutgers University Press.
Hook, J. N., Davis, D. E., Owen, J., Worthington, E. L., & Utsey, S. O. (2013). Cultural humility: Measuring openness to diverse clients. Journal of Counseling Psychology, 60(3), 353-366. doi: 10.1037/a0032595
Israel, B. A., Enf, E., Schulz, A. J., & Parker, E. A. (2013). Methods in community based participatory research for health (2nd ed.). San Francisco, CA: Jossey-Bass.
The Joint Commission. (2014). A crosswalk of the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in health and health care to The Joint Commission Hospital Accreditation Standards. Retrieved from The Joint Commission website https://www.jointcommission.org/assets/1/6/Crosswalk-_CLAS_-20140718.pdf
Jones, J. (1993). Bad blood: The Tuskegee syphilis experiment. New York: The Free Press.
Klawetter, S. (2016). MSW students’ experiences and understanding of social location: The development of a positionality measure. Paper presented at the Society for Social Work and Research 20th Annual Conference - Grand Challenges for Social Work: Setting a Research Agenda for the Future. Abstract retrieved from https://sswr.confex.com/sswr/2016/webprogram/Paper25933.html
Lowe, J., & Archibald, C. (2009). Cultural diversity: The intention of nursing. Nursing Forum, 44(1), 11-18. doi: 10.1111/j.1744-6198.2009.00122.x
Lowens, R. (2018, February 14). How do you practice intersectionalism? An interview with bell hooks [Blog post]. Retrieved from: http://blackrosefed.org/intersectionalism-bell-hooks-interview/
Martinsen, K. (2006). Care and vulnerability. Oslo, Norway: Akribe forlag.
Mastel-Smith, B., & Yarbrough, S. (2017). A reflexive exercise to promote cultural humility among doctoral nursing students. Journal of Nursing Education and Practice, 7(5), 68-75. https://doi.org/10.5430/jnep.v7n5p68
Merton, R. K. (1973). The sociology of science: Theoretical and empirical investigations. Chicago, IL: University of Chicago Press.
Minkler, M., Wallerstein, N. (2008). Community based participatory research for health: From process to outcomes (2nd ed.). San Francisco, CA: Jossey-Bass.
Moore, T., Cassidy, R., Cortes, C., Davey, K., Stoltzfus, K., Terry, P., & Robertson, A. (2017). An interprofessional review of cultural competency education: Approaches to strengthen healthcare management education in preparing culturally competent healthcare managers. Journal of Health Administration Education, 34(2), 319-343.
Muntinga, M., Krajenbrink, V., Peerdeman, S., Croiset, G. & Verdonk, P. (2016). Toward diversity-responsive medical education: Taking an intersectionality-based approach to a curriculum evaluation. Advances in Health Science Education, 21(3), 541–559. doi: 10.1007/s10459-015-9650-9
National Committee for Quality Assurance. (2016). A practical guide to implementing the national CLAS standards: For racial, ethnic and linguistic minorities, people with disabilities and sexual and gender minorities. National Committee for Quality Assurance: Washington, DC.
Ortega, R. M, & Faller, K. C. (2011). Training child welfare workers from an intersectional cultural humility perspective: A paradigm shift. Child Welfare, 90(5), 27-49.
Paparella-Pitzel, S., Eubanks, R., & Kaplan, S. L. (2016). Comparison of teaching strategies for cultural humility in physical therapy. Journal of Allied Health, 45(2), 139-146.
Roberts, D., & Jesudason, S. (2013). Movement intersectionality: The case of race, gender, disability, and genetic technologies. Du Bois Review, 10(2), 313-328. https://doi.org/10.1017/S1742058X13000210
Ross, L. (2010). Notes from the field: Learning cultural humility through critical incidents and central challenges in community-based participatory research. Journal of Community Practice, 18, 315-335. doi: 1070-5422 print/1543-3706
Schuessler, J. B., Wilder, B., & Byrd, L. W. (2012). Reflective journaling and development of cultural humility in students. Nursing Education Perspectives, 33(2), 96-99.
Tervalon, M., & Murray-Garcia, J. (1998). Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. Journal of Health Care for the Poor and Underserved, 9(2), 117-25.
U.S. Department of Health and Human Services, Office of Minority Health. (2013). National standards for culturally and linguistically appropriate services (CLAS) in health and health care: A blueprint for advancing and sustaining CLAS policy and practice. Retrieved from https://www.thinkculturalhealth.hhs.gov/pdfs/EnhancedCLASStandardsBlueprint.pdf
Vygotsky, L. S. (1978). Mind in society: The development of higher psychological processes. Cambridge, MA: Harvard University Press.
Willis, A., & Allen, B. (2011). The importance of cultural humility in cross cultural research. International Journal of Innovative Interdisciplinary Research, 1(1), 111-119.
Yancu, C., & Farmer, D. (2017). Product or process: Cultural competence or cultural humility? Palliative Medicine and Hospice Care Open Journal, 3(1), e1-e4. http://dx.doi.org/10.17140/PMHCOJ-3-e005
Yeager, K., & Bauer-Wu, S. (2013). Cultural humility: Essential foundation for clinical researchers. Applied Nursing Research, 26(4), 251-6. doi: 10.1016/j.apnr.2013.06.008

