For over 30 decades, cultural competence has commanded significant attention, being viewed as the cornerstone of fostering cross-cultural communication, reducing health disparities, improving access to better care, increasing health literacy and promoting health equity. However, a medley of definitions and conceptualizations has created intense debate, questioning its true ability to address cross-cultural problems in healthcare delivery. One ongoing debate centers around the relationship between cultural competence and cultural humility. Part I of this two-part series on cultural competemility will revisit this debate by discussing competing views of this relationship. A new paradigm of thought regarding the relationship between cultural competence and cultural humility will be proposed, one necessitating that cultural humility and cultural competence enter into a synergistic relationship. This synergistic relationship is embodied in a term coined "cultural competemility.” This article presents the debate regarding cultural competence verses cultural humility, defines the term cultural competemility, explains the relationship between cultural humility and cultural competence, describes the process of permeation and concludes by proposing a synergistic relationship between cultural competence and cultural humility to create the process of cultural competemility. Part II of this series will apply an intersectionality approach to the process of cultural competemility and offer strategies for nurses to actively challenge and address inequalities.
Key Words: Cultural competence, cultural diversity, ethnically diverse, cultural humility, transcultural healthcare, transcultural nursing, healthcare equity, healthcare disparities, social justice, cultural awareness, cultural knowledge, cultural skill, cultural encounters, cultural desire, cultural competemility
The notion of cultural competence is rooted in the social and political climate of the 1960s and 1970s... For over 30 decades, cultural competence has commanded significant attention and has become ubiquitous in human services' language and settings (Danso, 2016; Gallegos, Tindall, & Gallegos, 2008). Cultural competence has a history of being viewed as the cornerstone of fostering cross-cultural communication, reducing health disparities, improving access to better care, increasing health literacy and promoting health equity (Powell, 2016; Wong, LaVeist, & Sharfstein, 2015; Yancu & Farmer, 2017). The notion of cultural competence is rooted in the social and political climate of the 1960s and 1970s, where civil rights movements demanded respect for cultural diversity and attention to racial and ethnic inequalities in society (Chiarenza, 2012).
The concept first appeared in the social work literature and was referred to as ‘ethnic competence’ (Gallegos, Tindall, & Gallegos, 2008). Chiarenza (2012) has asserted that existing concepts of cultural competence share two basic assumptions, namely that cultural competence is a necessary and sufficient condition for working effectively with differences, and that cultural competence can be taught, learned, trained, and achieved. He added that the underlying assumption of this approach is that the greater the knowledge about another culture, the greater the competence in practice.
A medley of definitions and conceptualizations has created intense discussion around the construct of cultural competence... A medley of definitions and conceptualizations has created intense discussion around the construct of cultural competence, questioning its true ability to address cross-cultural problems in healthcare delivery (Danso, 2016; Harrison & Turner, 2010). One ongoing debate centers around the relationship between cultural competence and cultural humility, a term coined by Melanie Tervalon and Jann Murray-Garcia in 1998 (Tervalon & Murray-Garcia, 1998). This article will revisit this debate and discuss the competing views, maintaining that cultural competence should be either redefined, replaced, augmented, and/or distinguished from cultural humility. The purpose of this article is to introduce a new paradigm of thought regarding the relationship between cultural competence and cultural humility, one that will address the limitations of previous competing views and have a positive impact on the delivery of culturally conscious healthcare services and experiences to the patient, the family, and the community.
The Debate
Those opposing the concept of cultural competence assert that it is an endpoint and assumes that nurses and other healthcare professionals (HCPs) can learn a quantifiable set of attitudes and skills that will allow them to work effectively within the cultural context of the patient (Prasad et al., 2016). Other criticisms of cultural competence include its strong focus on knowledge acquisition; a lack of social justice issues; its understanding as a technical and communication technique; its potential to stereotype cultural groups; and its use of the concept of culture as merely a substitution for minority racial/ethnic group identity. This discussion has led for calls to replace cultural competence with the concept of cultural humility (Fisher-Borne, Cain & Martin, 2015; Tervalon & Murray-Garcia, 1998).
Cultural humility is often seen as an alternative approach to cultural competence. Cultural humility is often seen as an alternative approach to cultural competence. Cultural humility (Tervalon & Murray-Garcia, 1998) is a dynamic and lifelong process focusing on self-reflection and personal critique. These authors call for healthcare professionals (HCPs) to clearly differentiate cultural humility from cultural competence. The literature reveals many articles that differentiate cultural humility from cultural competence. Specifically, cultural humility requires less emphasis on knowledge and competency; places a greater emphasis on a life-long commitment; encourages nurturing of self-evaluation and critique; addresses power imbalances; promotes interpersonal sensitivity; requires an attitude of openness and egolessness; involves supportive interaction; entails maintaining an interpersonal stance that is other-oriented; necessitates learning from differences (Foronda, Baptiste, Reinhold, & Ousman, 2016; Hook, Davis, Owen, Worthington, & Utsey, 2013; Isaacson, 2014; Shaw, 2016; Tervalon & Murray-Garcia, 1998). However, in a critical reflection on cultural competence and cultural humility, Danso (2016) offered critiques about cultural humility replacing cultural competence. His analysis suggested that semantic appeal does not necessarily give cultural humility a useful edge over the construct it seeks to displace and appears not to add more value to practice than cultural competence.
In lieu of replacing the concept of cultural competence with cultural humility, other authors have taken the position that cultural competence and cultural humility must be viewed as being in apposition (i.e., side-by-side), rather than in opposition, of each other (Alsharif, 2012; Ortega & Faller, 2011; Yancu & Farmer, 2017). Yancu and Farmer (2017) maintained that cultural humility may complement, rather than replace, cultural competence. These authors added that if HCPs desire to interact effectively with a culturally diverse population, they need both process (cultural humility) and product (cultural competence).
Still other authors suggest a redefinition of cultural competence (Chiarenza, 2012; Koehn & Swick, 2006). Chiarenza urged HCPs to modify the way the concept of culture is used in healthcare to include not only ethnicity and race, but also intersections of ethnicity, race, gender, age, class, education, religion, sexual orientation, and physical ability, along with the unequal distribution of power and the existence of social inequities. Furthermore, Koehn and Swick (2016) proposed to redefine cultural competence by expanding it to include a transnational perspective. This broadens the scope of cultural competence by offering five skill domains. These domains are derived from the fields of international relations, specifically, cross-cultural psychology, and intercultural communication, namely analytic, emotional, creative, communicative, and functional.
A paradigm shift that challenges the aforementioned literature and suggests that cultural competence be redefined, replaced with cultural humility, or viewed in apposition to cultural humility, must be explored in an attempt to foster more effective cross-cultural communication, reduce health disparities, improve access to quality care, increase health literacy and promote health equity. This shift necessitates that cultural humility and cultural competence enter into a synergistic relationship, resulting in a combined effect greater than the sum of their separate effects.
The origin of cultural competemility is the deliberate blending of the terms cultural competence (compete) and cultural humility (mility). I have coined the term 'cultural competemility' to describe this synergistic relationship. The origin of cultural competemility is the deliberate blending of the terms cultural competence (compete) and cultural humility (mility). It is my assertion that the coined term 'cultural competemility' has the potential to contribute to positively impacting the delivery of culturally conscious healthcare services and experiences to all patients, families, and the community.
Defining Cultural Competemility
Cultural competemility is a conceptual framework that I have derived from two models of cultural competence: The Process of Cultural Competence in the Delivery of Healthcare Services (Campinha-Bacote, 2011), and A Biblically Based Model of Cultural Competence in the Delivery of Healthcare Services (Campinha-Bacote, 2013). The process model of cultural competence views cultural awareness, cultural knowledge, cultural skill, cultural encounters, and cultural desire as the five constructs of cultural competence. In this model, 'cultural encounters’ is the pivotal construct of cultural competence that provides the energy source and foundation for one’s journey towards cultural competence.
The biblically based model (Campinha-Bacote, 2013) of cultural competence in the delivery of healthcare services adds biblical components, such as humility, compassion, social justice, Imago Dei (image of God), and teachableness in defining the process of cultural competence. Specifically, this model views the process of cultural competence as the interdependent relationship among the following six constructs of cultural competence: imago Dei, cultural desire, cultural awareness, cultural knowledge, cultural skill and cultural encounters. The model also integrates specific intellectual and moral virtues: love, caring, social justice, humility, love of truth, teachableness, intellectual honesty, wisdom, discernment, prudence, attentiveness, studiousness, practical wisdom, understanding, temperance, patience, and compassion into these six constructs. These two frameworks provide the foundation for the synergistic process between cultural humility and cultural competence.
Cultural competemility is defined as the synergistic process between cultural humility and cultural competence in which cultural humility permeates each of the five components of cultural competence... Cultural competemility is defined as the synergistic process between cultural humility and cultural competence in which cultural humility permeates each of the five components of cultural competence: cultural awareness, cultural knowledge, cultural skill, cultural desire, and cultural encounters. From this perspective, cultural competemility can be viewed as simultaneously being both a process of becoming and the process of being. Individuals must engage in the process of becoming culturally competent while synchronously being engaged in the process of cultural humility. Cultural competemility requires HCPs to maintain both an attitude and a lens of cultural competence and cultural humility as they engage in cultural encounters, obtain cultural knowledge, demonstrate the cultural skill of conducting a culturally sensitive cultural assessment, and become culturally aware of both their own biases and the presence of “isms” (e.g., racism, sexism, ableism, classism, ageism, anti-Semitism, heterosexism, colorism, ethnocentrism).
To fully comprehend the concept of cultural competemility, HCPs must reframe previous extant views of cultural competence and cultural humility. To fully comprehend the concept of cultural competemility, HCPs must reframe previous extant views of cultural competence and cultural humility. This reframing process necessitates that they step back from what is being said and done in this field of study and consider the alternative lens of a synergistic relationship by which cultural competence and cultural humility become the process of cultural competemility.
As HCPs enter into the process, it is necessary to reframe the concept of humility. While the literature suggests that HCPs operate from a demeanor of humility, there is said to be a paradox in possessing humility. Scholars have asserted that when we become aware of our humility and openly acknowledge it, we’ve lost it (Campinha-Bacote, 2013; Robinson & Alfano 2016). Furthermore, Robinson and Alfano (2016) maintain that humility is fraught with contradiction because one cannot truthfully claim to be humble. Theses authors maintain that by consciously striving to become humble, one might become less so, since humility supposedly is an asset that one can have only by not paying attention to it. From this perspective it begs the question: “Is it possible to seek or learn cultural humility?“ From a cultural competemility framework, it is conceivable.
...by consciously striving to become humble, one might become less so, since humility supposedly is an asset that one can have only by not paying attention to it. Drawing from the field of theology, Ells (n.d.) and Campinha-Bacote (2013) argue that there are theological ways to humble oneself. Ells (n.d.) provides examples which include accepting a lowly place; receiving correction and feedback from others graciously; choosing to serve others; being quick to forgive; cultivating a grateful heart; purposely speaking well of others; and acknowledging wrongdoings to others. Therefore, cultural humility is an attitude of relating to patients; it has more to do with the HCPs' actions and the ends to which they are directed. As eloquently stated by author Rick Warren (2012), “This is true humility: not thinking less of ourselves but thinking of ourselves less” (p. 265).
Reframing cultural competence as an ongoing process is critical in pursuing cultural competemility. As HCPs enter into the process of cultural competemility, it is also necessary to reframe the interpretations found in the literature regarding the meaning of cultural competence. Contrary to the existing literature, cultural competence does not view competence as an endpoint or product; nor does it assume that nurses and other healthcare professionals can learn a quantifiable set of attitudes and skills that will allow them to work effectively within the cultural context of the patient. Reframing cultural competence as an ongoing process is critical in pursuing cultural competemility. Once the HCP has reframed traditional views on competence and humility, it is important to understand the synergistic relationship between these two concepts.
Synergistic Relationship Between Cultural Humility and Cultural Competence
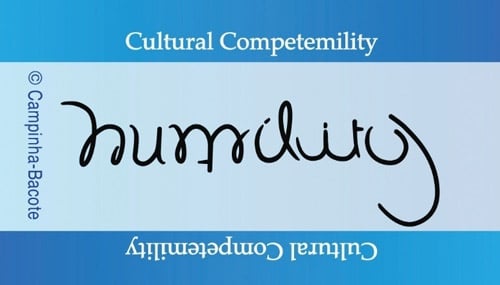
The process of cultural competemility involves the total permeation of cultural humility into the five components of cultural competence. The result of this permeation can be symbolically represented in a rotating ambigram. An ambigram is a word, art form, or other symbolic representation whose elements retain meaning when viewed or interpreted from a different direction, perspective, or orientation. Figure 1 displays an ambigram in which the word competence, when flipped or rotated, spells the word humility (Figure 2). Thus, humility is found in competence and competence is found is humility. To further illuminate the relationship between cultural humility and cultural competence, the permeation and synergistic process of cultural humility into cultural competence will be discussed.
Figure 1: Competence/Humility Ambigram

Figure 2. Humility/Competence Ambigram
Unconscious impermeability is being totally unaware that cultural humility is required during the process of becoming culturally aware and culturally knowledgeable... The total permeation of cultural humility into cultural awareness, cultural encounters, cultural skill, cultural desire, and cultural knowledge can be viewed as a process that exists along a continuum ranging from unconscious impermeability to unconscious permeability. Unconscious impermeability is being totally unaware that cultural humility is required during the process of becoming culturally aware and culturally knowledgeable, obtaining cultural skill and cultural desire, as well as entering into cultural encounters. In this stage, the HCP is totally unaware and unconcerned regarding the power imbalances that exist during the clinical encounters, or the social inequities that culturally and ethnically diverse patients experience.
In contrast, conscious impermeability is the awareness that cultural humility must be exhibited during the clinical encounter; however, the HCP is unable to successfully display the cultural lens and demeanor of culturally humility. Here, the HCP becomes keenly aware of the need for cultural humility by attending a workshop, reading an article or book on the topic, or discussing the topic with colleagues, but is not able to grasp the concept of how to personally demonstrate cultural humility. Conscious permeability, however, is the mindful act of learning how to become culturally humble and to let this cultural lens pervade the entire cultural encounter with the patient.
Conscious permeability... is the mindful act of learning how to become culturally humble...Finally, unconscious permeability is the ability of the HCP to spontaneously operate from a place of cultural humility when pursuing cultural awareness, cultural knowledge, and obtaining cultural skill and cultural desire, as well as entering into cultural encounters. In other words, the healthcare professional does not rely on specific rules to maintain a humble attitude, but rather has developed an intuitive grasp of needed interactions and behaviors that demonstrate cultural humility to the patient. From a continuum perspective, cultural competemility can be regarded as the ongoing process of moving from a position of unconscious impermeability to unconscious permeability when cultural awareness, cultural knowledge, cultural skill, cultural encounters, and cultural desire are being pursued. Below, each of these five components of cultural competence will be defined and strategies on how to allow cultural humility to permeate each component will be discussed.
The Process of Permeation
The conscious infusion of cultural humility into the construct of cultural awareness involves the commitment of personal sacrifice. Cultural awareness involves the process of conducting a self-examination and critical reflection of one’s own biases towards other cultures and also an in-depth exploration of one’s cultural background (Campinha-Bacote, 2011). Cultural awareness also involves being aware of the existence of documented racism and other “isms” in healthcare delivery. The HCP can allow cultural humility to permeate cultural awareness by intentionally and mindfully acknowledging the privilege and power inherent in their clinician role. The conscious infusion of cultural humility into the construct of cultural awareness involves the commitment of personal sacrifice. Sacrifice is an expression of biblical kindness, for it involves denying ourselves something (Campinha-Bacote, 2013). Healthcare professionals must be willing to sacrifice their prejudices and biases toward culturally different patients in order to develop cultural competemility. Howard (2003) states that we must sacrifice our “proprietary assumptions of our own rightness and our unreflective grip on our own certainty” (p. 2). This type of sacrifice involves the moral commitment to serve all patients, regardless of their cultural values, beliefs, or practices.
Cultural knowledge is defined as the process in which the HCP seeks and obtains a sound educational base about culturally diverse groups (Campinha-Bacote, 2011). Additionally, cultural knowledge includes the integration of three areas: a) health-related beliefs, practices, and cultural values of culturally and ethnically diverse populations; b) disease incidence and prevalence among culturally and ethnically diverse populations; and c) treatment efficacy among culturally and ethnically diverse populations (Lavizzo-Mourey, 1996). The most serious barrier to cultural competemility is not a lack of knowledge of the details of any given cultural orientation, but rather the potential to stereotype individuals. The concept of intra-cultural variation is critical to remember when gaining cultural knowledge to prevent the stereotyping of patients from different cultural groups.
The most serious barrier to cultural competemility is not a lack of knowledge of the details of any given cultural orientation, but rather the potential to stereotype individuals. Intra-cultural variation refers to the variation that is noted within cultural groups, as well as the expected variation that exists across cultural groups. No individual is a stereotype of one’s culture of origin, but rather a unique blend of the diversity found within each culture, an accumulation of life experiences, and the process of acculturation to other cultures.
The infusion of cultural humility into cultural knowledge allows meaningful and deliberate cultural encounters to connect with the patient as a unique, individual person, and not a stereotype of the patient’s cultural group. Cultural competemility necessitates a consciousness of the limits of one's knowledge, including sensitivity to circumstances in which one's native egocentrism is likely to function self-deceptively and limit one's viewpoint (Foundation for Critical Thinking, 1996).
Healthcare professionals must be willing to be informed/taught by their patients and others...The attribute of teachableness is necessary as cultural humility enters the component of cultural knowledge (Campinha-Bacote, 2013). Teachableness is the intellectual virtue that exudes the quality of being capable of receiving instruction and a willingness or readiness to be informed and instructed. Healthcare professionals must be willing to be informed/taught by their patients and others, for a teachable spirit allows HCP to recognize that they can learn not only from their colleagues, but also from their patients and other people (cultural informants), regardless of the person’s status or achievement.
Cultural skill is the ability to conduct a cultural assessment to collect relevant cultural data regarding the patients whom one serves (Campinha-Bacote, 2011). Cultural humility is infused into this construct by conducting a cultural assessment that requires more than selecting a tool and asking the patient questions listed. The healthcare professional’s approach must be done in a culturally sensitive manner. To infuse cultural humility into cultural skill, it is suggested that HCPs listen with interest and remain non-judgmental about what they hear. Boesen (2012) offers the following acronym as a guide to ‘ASSESS’ how to develop consistent cultural humility: Ask questions in a humble, safe manner; Seek self-awareness; Suspend judgment; Express kindness and compassion; Support a safe and welcoming environment; and Start where the patient is at.
...it is suggested that HCPs listen with interest and remain non-judgmental about what they hear. Another approach to gain insight and understand another’s culture is the process of ‘passing over and coming back’ (Dunne, 1972). ‘Passing over’ refers to shifting to the standpoint of another culture, another way of life, another way of seeing an issue. It is followed by an equal and opposite process of ‘coming back’ with new insight. We enter (pass over) into the feelings of our patients by allowing them to share their cultural traditions. We then come back to the world of our own cultural traditions with new insight into the patient’s worldview, thus allowing us to formulate a mutually acceptable and culturally relevant treatment regimen. Dunne (1972) noted that the process of passing over rests on the recognition that no matter what one already knows, there is always more to know, for no standpoint can be the endpoint. Thus, passing over to another world is possible for us because we share common experiences of being humans.
Cultural encounters encourage the HCP to directly engage in face-to-face interactions and other types of encounters with patients from culturally diverse backgrounds to modify existing beliefs about a cultural group and prevent possible stereotyping (Campinha-Bacote, 2011). Continuous cultural encounters are needed to acquire cultural awareness, cultural knowledge, cultural skill, and cultural desire. Cultural humility permeates the cultural encounter as the HCP becomes mindful both that every encounter is an opportunity for inquisitiveness, self-reflection, critique, and life-long learning, and also that maintaining an open heart and mind are necessary (Fahlberg, Foronda, & Baptiste, 2016).
...infusion of cultural humility into the component of cultural encounters is more about “being” than about “doing” and flows from a quality of presence that we then extend to others. Key aspects of cultural humility during the cultural encounter are availability and presence, with the realization that presence is more than the physical presence of the HCP with patients, but rather a matter of being available or open to patients (Marsden, 1990; Paterson & Zderad, 1976). Thus, infusion of cultural humility into the component of cultural encounters is more about “being” than about “doing” and flows from a quality of presence that we then extend to others. We must meet patients where they are and take the time to listen and learn who they are, what they need, and what they bring to the clinical encounter. In this encounter, we must ‘hold space’ for patients. Holding space means that the HCP is willing to walk alongside patients without judging them and requires the HCP to be totally present, attentive to what is said and not said, and what is happening and not happening (Hauka, 2017). With the HCP holding the space, patients are more free to participate in planning their care.
Cultural desire is the motivation of the HCP to ‘want to’ (as opposted to 'have to') engage in the process both of becoming culturally aware, culturally knowledgeable, culturally skillful, and also seeking cultural encounters (Campinha-Bacote, 2011). This form of motivation requires passion. Wilkerson (2002) asserted that true passion is born of anguish and added that “Anguish means extreme pain and distress; The emotions so stirred that it becomes painful, acute deeply felt inner pain, because of conditions about you, in you, or around you” (p. 7). Healthcare professionals must become anguished at the social justice issues facing our growing culturally diverse world and the severe inequalities that exist in healthcare. We must not forget the Institute of Medicine’s landmark report (Smedley, Stith, & Nelson, 2002) which revealed that ethnic minorities in the United States are less likely to receive medical care and experience lower quality of healthcare services .
Similarly, in 2001, the Surgeon General’s report on race, culture and ethnicity and mental health documented racial and ethnic disparities in mental healthcare surrounding issues of misdiagnosis, underutilization, overrepresentation, and improper treatment (U.S. Department of Health and Human Services, 2001). Explanations are multifaceted; however, there is evidence to support (Beach, Rosner, Cooper, Duggan, & Shatzer, 2007; Betancourt, Corbett, & Bondaryk, 2014) that these racial and ethnic disparities are related to the lack of cultural competemility among HCPs. These landmark reports must evoke in us enough passion to ‘want to’ engage in the process of cultural competemility. However, passion must be tempered with a cultural humility lens. Passion drives us forward, and a lens of cultural humility will keep us focused.
A cultural humility lens of cultural desire dictates an understanding of social inequalities and how they affect individuals. When cultural humility saturates the cultural desire of HCPs, there becomes a profound commitment to social justice actions. Healthcare professionals will then realize that views they hold about patients and their everyday interactions with patients and with one another can either contribute to socially just actions or reproduce social injustices (Anderson et al., 2009). Research continues to demonstrate a direct correlation between inequality and negative health outcomes. It is because of this link that healthcare professionals must consciously connect cultural competemility with social justice.
Conclusion
The literature has argued that a focus on developing a culturally competent healthcare workforce, though well intended, has resulted in an unintentional over-emphasis on shared group characteristics; an undervaluing of unique differences of individuals; a failure to address the privilege and power imbalances between providers and clients; an unbalanced focus on knowledge acquisition; and a misuse of the concept of culture as a substitution for minority and/or racial/ethnic group identity(Fisher-Borne et al., 2015; Prasad et al, 2016; Tervalon & Murray-Garcia, 1998). Strategies to address these issues have revolved around introducing the concept of cultural humility and its various relationships with cultural competence. This article offers new insight into this relationship by proposing a synergistic relationship between cultural competence and cultural humility to create the process of cultural competemility. This approach has the potential to further contribute to this body of literature.
To advance the concept of cultural competemility, an application of this conceptual framework is needed. In an upcoming article in this journal, authors Elizabeth Fitzgerald and Josepha Campinha-Bacote will utilize cultural competemility as the framework for becoming culturally competent at both the individual and organizational level. Utilizing an intersectionality approach to cultural competemility, this article will offer salient strategies in which nurses in practice, education, research and/or administrative positions can engage to actively challenge and address inequalities as they journey towards cultural competemility. Additional studies are needed, however, to determine valid methods to assess the development of cultural competemility, to assess client perceptions of providers who practice it, and to evaluate whether cultural competemility affects client outcomes (Davis, Worthington, & Hook, 2010; Davis et al. 2011; Worthington, Davis, & Hook, 2017).
Author
Josepha Campinha-Bacote, PhD, MAR, PMHCNS-BC, CTN-A, FAAN
Email: meddir@aol.com
Dr. Campinha-Bacote is President of Transcultural C.A.R.E. Associates. She has published extensively on issues concerning transcultural healthcare. Dr. Campinha-Bacote is certified by the Transcultural Nursing Society (TCNS) as an Advanced Certified Transcultural Nurse and has been inducted into the TCNS as a Transcultural Nursing Scholar. She been the recipient of several national and international honors and awards, including the Transcultural Nursing Society Leadership Award, the Ethnic/Racial Minority Fellowship Award from the National Institute of Mental Health, the Lifetime Achievement Diversity Award from the University of Rhode Island, and the Minority Health Knowledge Award from the Ohio Commission on Minority. Dr. Campinha-Bacote, a Fellow of the American Academy of Nursing, has served on the National Advisory Committee to the United States Department of Health and Human Services Office of Minority Health to develop standards for Culturally and Linguistically Appropriate Services in Health Care.
References
Alsharif, N.Z. (2012). Cultural humility and interprofessional education and practice: A winning combination. American Journal of Pharmaceutical Education, 76 (7), 120. doi:10.5688%2Fajpe767120
Anderson, M., Rodney, P., Reimer-Kirkham, S., Browne, A., Khan, K. & Lynam, J. (2009). Inequities in health and healthcare viewed through the ethical lens of critical social justice: Contextual knowledge for the global priorities ahead. Advances in Nursing Science, 32(4), 282–294. doi:10.1097/ANS.0b013e3181bd6955
Beach, M., Rosner, M., Cooper, L., Duggan, P., and Shatzer, J. (2007). Can Patient-Centered Attitudes Reduce Racial and Ethnic Disparities in Care? Academic Medicine, 82(20), 193-198.
Betancourt, J., Corbett, J. & Bondaryk, M. (2014). Addressing disparities and achieving equity: Cultural competence, ethics, and health-care transformation. Chest, 145, 143–148.
Boesen. L. (January 17, 2012). Creating connections through cultural humility. [web log comment]. Retrieved from http://www.lisaboesen.com/creating-connections-through-cultural-humility/
Campinha-Bacote, J. (2011). Coming to know cultural competence: An evolutionary process. International Journal for Human Caring, 15(3), 42-48. doi:10.20467/1091-5710.15.3.42
Campinha-Bacote. J. (2013). A biblically based model of cultural competence in the delivery of healthcare services: Seeing “Imago Dei” (2nd ed.). Cincinnati, OH: Transcultural C.A.R.E. Associates.
Chiarenza, A. (2012). “Developments in the concept of ‘cultural competence.’” In D. Ingleby, A. Chiarenza, W. Devillé, and I. Kotsioni (Eds.), Inequalities in health care for migrants and ethnic minorities (pp. 66-81). Antwerp: Garant
Danso, R. (2016). Cultural competence and cultural humility: A critical reflection on key cultural diversity concepts. Journal of Social Work 18(4), 410-430. doi:10.1177/1468017316654341
Davis, D.E., Hook, J.N, Worthington, E.L., Van Tongeren, D.R.., Gartner, A.L., Jennings, D.J., & Emmons, R. A. (2011). Relational humility: Conceptualizing and measuring humility as a personality judgment. Journal of Personality Assessment, 93(3), 225-234. doi:10.1080/00223891.2011.558871.
Davis, D.E., Worthington, E.L., & Hook, J.N. (2010). Humility: Review of measurement strategies and conceptualization as personality judgment. Journal of Positive Psychology, 5(4), 243-252. doi:10.1080/17439761003791672
Dunne, J. (1972). The way of all the earth. New York, NY: Macmillan.
Ells, A. (n.d.) What does the bible say about humility? Counselor's Corner, 2(12). Retrieved from https://bibleresources.org/humility/
Fahlberg, B., Foronda, C., & Baptiste, D. (2016). Cultural humility: The key to patient/family partnerships for making difficult decisions. Nursing2016, 46(9): 14-16. doi:10.1097/01.NURSE.0000490221. 61685.e1
Fisher-Borne, M, Cain, J.M., & Martin, S. L. (2015). From mastery to accountability: Cultural humility as an alternative to cultural competence. Social Work Education, 34 (2), 165-181. doi:10.1080/02615479.2014.977244
Foundation for Critical Thinking. (1996). Valuable intellectual virtues. Tomales, CA:Author. Retrieved from http://www.criticalthinking.org/pages/valuable-intellectual-traits/528
Foronda, C., Baptiste, D., Reinhold, M.M., & Ousmane, K. (2016). Cultural humility: A concept analysis. Journal of Transcultural Nursing, 27(3), 201-217. doi:10.1177/1043659615592677
Gallaher, D. (April 5, 2007). Polishing the heart. Journal of Sacred Work. [journal online]; Retrieved from http://journalofsacredwork.typepad.com/journal_of_sacred_work/2007/04/polishing_the_h.html
Gallegos, J., Tindall, C. & Gallegos, S. (2008). The need for advancement in the conceptualization of cultural competence. Advances in Social Work, 9(1), 51-62.
Harrison, G. & Turner, R. (2010). Being a ‘culturally competent’ social worker: Making sense of a murky concept in practice. British Journal of Social Care, 41(2), 1-18.
Hauka, L. (2017, Dec 6). The sweetness of holding space for another. HuffPost. Retrieved from https://www.huffingtonpost.com/lynn-hauka/the-sweetness-of-holding-_b_9558266.html
Hook, J.N., Davis, D.E., Owen, J., Worthington, E.L. & Utsey, S. O. (2013). Cultural humility: Measuring openness to diverse clients. Journal of Counseling Psychology, 60 (3), 353-366. doi:10.1037/a0032595
Howard, G, (2003). Speaking of difference: Reflections on the possibility of culturally competent conversation. New Horizons for Learning Online Journal, 9(2). Retrieved from http://www.ghequityinstitute.com/gh_articles/speaking_of_difference.pdf
Isaacson, M. (2014). Clarifying concepts: Cultural humility or competency. Journal of Professional Nursing, 30(3), 251-258.
Koehn, P. & Swick, H. (2006). Medical education for a changing world: Moving beyond cultural competence into transnational competence. Academic Medicine, 81(6), 548-556.
Lavizzo-Mourey, R. (1996). Cultural competence: Essential measurements of quality or managed care organizations. Annals of Internal Medicine, 124(10), 919-921.
Marsden, C. (1990). Real presence. Heart & Lung, 19, 540-541.
Ortega, R.M, & Faller, K.C. (2011). Training child welfare workers from an intersectional cultural humility perspective: A paradigm shift. Child Welfare, 90 (5), 27-49.
Paterson, J., and Zderad, L. (1976). Humanistic nursing. New York: John Wiley & Sons.
Powell, D. (2016). Social determinants of health: Cultural competence is not enough. Creative Nursing, 22(1), 5-10. doi:10.1891/1078-4535.22.1.5
Prasad, S., Nair, P., Gadhvi, K., Barai, I., Danish, H. & Philip, A. (2016). Cultural humility: Treating the patient, not the illness. Med Educ Online. 2016: 21. doi:10.3402/meo.v21.30908.
Robinson, B. and Alfano, M. (2016). I know you are, but what am I? Anti-individualism in the development of intellectual humility and Wu-wei. Logos and Episteme, 7(4), 435-459.
Smedley, B., Stith, A., and Nelson, A. (2002). Unequal treatment: Confronting racial and ethnic disparities in health care. Board on Health Sciences Policy. Institute of Medicine. Washington, DC: National Academic Press.
Shaw, S. (2016, Dec 27). Practicing cultural humility. Counseling Today. Retrieved from http://ct.counseling.org/2016/12/practicing-cultural-humility/
Tervalon, M. & Murray-Garcia, J. (1998). Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. Journal of Health Care for the Poor and Underserved, 9(2), 117-25.
U.S. Department of Health and Human Services. (2001). Mental health: Culture, race, and ethnicity—A supplement to mental health: A report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services.
Warren, R. (2012).The purpose driven life: What on earth am I here for? Grand Rapids, MI: Zondervan.
Wilkerson, D. (2002). A call to anguish (text transcription). SermonIndex.net, pp, 1-7. Retrieved from http://img.sermonindex.net/modules/articles/article_pdf.php?aid=32622
Wong, W., LaVeist, T. and Sharfstein, J. (2015). Achieving health equity by design. JAMA, 313(14), 1417-1418. doi:10.1001/ jama.2015.2434
Worthington, E., Davis, D. & Hook, J. (2017). Handbook of cultural humility. NY: Routledge.
Yancu, C. & Farmer, D. (2017). Product or process: Cultural competence or cultural humility? Palliative Medicine and Hospice Care Open Journal, 3(1), e1-e4. doi:10.17140/PMHCOJ-3-e005

