Translation science is a relatively young area of investigation that is rapidly growing. Although a number of healthcare practices have an evidence-base to guide care delivery, their use is not a part of routine practice. The gap between the availability of evidence-based practice (EBP) recommendations and application to improve patient care and population health is linked to poor health outcomes. Translation science, also known as implementation science, is testing implementation interventions to improve uptake and use of evidence to improve patient outcomes and population health. It also helps clarify what implementation strategies work for whom, in what settings, and why. This scientific field emerged to investigate which implementation strategies work to promote use of EBPs, and uncover the mechanisms by which they work. Advancements in translation science can expedite and sustain the successful integration of evidence in practice to improve care delivery, population health, and health outcomes. This article offers an introductory overview of translation science and addresses issues in this field of science such as variation in terminology; theories and models; implementation strategies; and context and implementation related to EBPs.
Key words: Translation science, models and theories, terminology, implementation science
The gap between the availability of evidence and application in care delivery contributes to poor health outcomes...Translation science is a rapidly growing area of investigation. A number of healthcare practices have an evidence-base but they are not yet a part of routine care. The gap between the availability of evidence and application in care delivery contributes to poor health outcomes such as obesity, healthcare-acquired infections, and injurious falls (Centers for Disease Control and Prevention [CDC], 2016; Conway, Pogorzelska, Larson, & Stone, 2012; Shever, Titler, Mackin, & Kueny, 2011; Sving, Gunningberg, Högman, & Mamhidir, 2012; Titler et al., 2016). Although United States (U.S.) spending in health exceeds that of all developed nations, key measures of health lag behind, particularly for preventable chronic conditions and associated functional decline (Squires & Anderson, 2015).
Multiple opportunities abound for implementation of evidence to improve population health and healthcare delivery (Institute of Medicine [IOM], 2009; IOM, 2011a; IOM, 2011b, IOM, 2012a; IOM, 2012b; IOM, 2013a; National Academies of Sciences, Engineering and Medicine [NAM], 2015). Furthermore, Clinical and Translational Science Award (CTSA) Programs, funded by NIH, are expected to partner with communities, practices, and clinicians in translating findings from research into practices and community programs (IOM, 2013b).
The field of translation science investigates which implementation strategies work to promote use of evidence-based practices...The field of translation science investigates which implementation strategies work to promote use of evidence-based practices (EBPs) for whom, in what types of settings, and uncovers the mechanisms by which they work. Advancements in translation science can expedite integration of evidence in practice to improve care delivery, population health, and health outcomes (Henly et al., 2015). This article offers a basic overview of translation science and issues in the field.
Historical Overview
Nursing has a rich history of using research in practice... Nursing has a rich history of using research in practice pioneered by Florence Nightingale (Nightingale, 1858; 1859; 1863a; 1863b). Evidence-based practice (previously called research utilization) was advanced by several initiatives, including the:
- Conduct and Utilization of Research in Nursing (CURN) project (Horsley, 1983)
- Western Interstate Commission for Higher Education in Nursing (WICHEN) project on nursing research development (Krueger, 1978; Krueger, Nelson, & Wolanin, 1978; Lindeman & Krueger, 1977)
- Nursing Child Assessment Satellite Training project (NCAST) (King, Barnard, & Hoehn, 1981)
- Moving New Knowledge into Practice project (Cronenwett, 1995; Funk, Tornquist, & Champagne, 1989)
- Orange County Research Utilization in Nursing project (Rutledge & Donaldson, 1995)
...diversity of terminology impedes efforts to synthesize, advance, and apply findings from translation science. These seminal projects provided a strong foundation for evidence-based practice (EBP). Today, many nurses lead the healthcare agenda for EBP (Dickinson & Shever, 2012; Kelley, 2010; Kueny, Shever, Lehan Mackin, & Titler, 2015; Mark, Titler & Lattimer, 2014; Shever & Dickinson, 2013; Titler & Moore, 2010; Titler, 2010; Titler, 2011; Titler, 2014; Titler et al., 2017), and translation science (Dobbins et al., 2009; Estabrooks et al., 2008; McCormack et al., 2013; Newhouse, Bobay, Dykes, Stevens, & Titler, 2013; Rycroft-Malone et al., 2012; Shuman, Ploutz-Snyder, & Titler, 2018; Shuman, Xie, Herr, & Titler, 2017; Slaughter & Snelgrove-Clark, 2015; Titler et al., 2009; Titler et al., 2016; Titler et al., 2017; Wilson et al., 2016). As a result, the scientific body of knowledge translation in healthcare is growing (Titler, 2014).
Definition of Terms
Terminology is an issue in translation science (Colquhoun et al., 2014; Lokker, McKibbon, Colquhoun, & Hempel, 2015; McKibbon et al., 2010). For example, McKibbon and colleagues (2010) identified 100 different terms to describe translation research. This diversity of terminology impedes efforts to synthesize, advance, and apply findings from translation science. Lack of a common language makes it difficult for researchers to learn from each other’s studies; to collaborate across geographic boundaries and disciplines; and to search for and synthesize scientific findings (Colquhoun et al., 2014).
One important distinction is the difference between conduct of research and EBP. An overview of terminology is in Table 1. One important distinction is the difference between conduct of research and EBP. Evidence-based practice and conduct of research have distinct purposes, questions, approaches, and evaluation methods. Conduct of research is the systematic investigation of a phenomenon that addresses research questions or hypotheses to create generalizable knowledge and advance the state of the science (LoBiondo-Wood & Haber, 2018). In contrast, EBP is the conscientious and judicious use of current best evidence in conjunction with clinical expertise, patient values, and circumstances to guide healthcare decisions (Straus, Richardson, Glasziou, Richardson, & Haynes, 2011; Titler, 2014).
Another important distinction is the difference between EBP and translation science, also known as implementation science. “Best evidence” includes findings from randomized controlled trials, evidence from other scientific designs such as descriptive and qualitative research, as well as information from case reports and scientific principles. When enough research evidence is available, practice should be guided by research findings in conjunction with clinical expertise and patient values. In some cases, however, a sufficient research base may not be available, and health care decision-making is informed by other evidence sources such as scientific principles, quality improvement data, or quality improvement reports published in peer reviewed journals.
...EBP and translation science, though related, are not interchangeable terms. Another important distinction is the difference between EBP and translation science, also known as implementation science. Translation science is conduct of research. It focuses on testing implementation interventions to improve uptake and use of evidence to improve patient outcomes and population health, as well as to clarify what implementation strategies work for whom, in what settings, and why (Eccles & Mittman, 2006; Titler, 2014). An emerging body of knowledge in translation science provides a scientific base for guiding the selection of implementation strategies to promote adoption of EBPs in real-world settings (Dobbins et al., 2009; Titler, 2010; Titler et al., 2016). Thus EBP and translation science, though related, are not interchangeable terms. EBP is the actual application of evidence in practice (the “doing of” EBP), whereas translation science is the study of implementation interventions, factors, and contextual variables that effect knowledge uptake and use in practices and communities. Translation science is research; various research designs and methods are used to address the research questions or hypotheses (Titler, 2014).
Table 1. Terms Used in EBP and Translation/Implementation Science
|
Term |
Description |
|
Translational Research |
Translational research is a dynamic continuum from basic research through application of research findings in practice, communities and public health settings to improve health and health outcomes. Translation Research progresses across five phases:
|
|
Conduct of Research |
The systematic investigation of a phenomenon to answer research questions or hypotheses that advances the state of the science (LoBiondo-Wood & Haber, 2018). |
|
Implementation Science (also called translation science) |
A field of science that focuses on testing implementation interventions to promote uptake and use of evidence to improve patient outcomes and population health, and explicate what implementation strategies work for whom, in what settings, and why (Eccles & Mittman, 2006; Titler, 2010; Titler, 2014). |
|
Dissemination Research |
The targeted distribution of information and intervention materials to a specific public health or clinical practice audience with the intent to spread, scale-up, and sustain knowledge use and evidence-based interventions (Department of Health and Human Services, 2018). |
|
Comparative effectiveness research (CER) |
CER is the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat and monitor a clinical condition, or to improve the delivery of care. The purpose of CER is to assist consumers, clinicians, purchasers, and policy makers to make informed decisions that will improve healthcare at both the individual and population levels. This definition implies the direct comparison of two or more effective interventions in patients who are typical of day-to-day clinical care (IOM, 2009). |
|
Knowledge translation |
Knowledge translation is a term primarily used in Canadian implementation research and is defined by the Canadian Institutes for Health Research (CIHR) as “a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically-sound application of knowledge to improve the health of Canadians, provide more effective health services and products and strengthen the health care system” (CIHR, 2017, para. 1). |
|
Knowledge Transfer |
The process of getting knowledge from producers to potential users (Graham et al., 2006). However, knowledge transfer has been criticized for its unidirectional notion and its lack of concern with the implementation of transferred knowledge(Graham et al., 2006). |
|
Evidence Based Practice |
The conscientious and judicious use of current best evidence in conjunction with clinical expertise and patient values to guide healthcare decisions (Straus et al., 2011; Titler, 2014). |
|
Evidence Based Policy |
Evidence-based policy is developed through a continuous process that uses the best available quantitative and qualitative evidence to improve public health outcomes (Brownson, Chriqui, Stamatakis, 2009). |
|
Evidence Informed Decision-making (EIDM) |
EIDM is the process of combining a range of sources of evidence to inform a decision. In practice, this occurs within a political context that requires consideration of a range of other factors including research evidence, community views, budget constraints, and expert opinion (Armstrong et al, 2013). |
|
Policy dissemination & implementation research |
Policy dissemination and implementation research is focused on generating knowledge to effectively spread research evidence among policymakers and integrate evidence-based interventions into policy designs (Purtle, Peters, & Brownson, 2016). |
[Modified from Titler, LoBiondo-Wood, & Haber, J, (in press)]
Theories and Models of Translation Science
There are multiple theories and models in translation science (See Table 2). A recent study of 223 implementation scientists, representing 12 countries, found that they used over 100 different theories spanning multiple disciplines (Birken, Powell, Shea et al., 2017). In a qualitative review of implementation theories, models and frameworks, Nilsen (2015) noted 3 organizing aims for their use: 1) to describe or guide the process of translating research into practice; 2) to understand and/or explain what influences implementation outcomes; and 3) to evaluate implementation. Within the first aim are process models that specify steps for promoting use of research in practice; these models are often called action models of EBP (e.g., Iowa Model, Knowledge to Action model), with most originating from the nursing discipline (Nilsen, 2015).
Classic theories are those derived from other disciplines... Within the second aim (to understand/explain) are determinate frameworks, classic theories, and implementation theories. Determinate frameworks (e.g., Consolidated Framework for Implementation Research) describe domains of factors that influence implementation outcomes such as alignment of practice behaviors with the evidence-base. Classic theories are those derived from other disciplines such as psychology, sociology, and organizational theory that are applied to implementation studies. Examples include the Theory of Planned Behavior and Rogers’ Diffusion of Innovation Theory, which is considered the most influential theory in implementation science. Implementation theories are those that have been developed or adapted by researchers for use in implementation science (e.g., Normalization Process Theory) to guide the understanding and explanation of certain aspects of implementation.
Within the third aim (to evaluate implementation) are those frameworks that provide a structure for evaluating implementation efforts. The RE-AIM framework (Glasgow, Vogt, & Boles, 1999) is an example of a commonly used evaluation framework particularly in public health.
Table 2. Example of Theories, Frameworks and Models in Translation/Implementation Science
|
Theory/Model |
Brief Description and Selected References |
|
Promoting Action on Research Implementation in Health Services (PARIHS)/i-PARIHS |
i-PARIHS is a revision of the original PARIHS framework. In the revised i-PARIHS framework, successful implementation is primarily specified in terms of the achievement of implementation goals and results from the facilitation of an innovation with the recipients in their (local, organizational and health system) context. The core constructs are facilitation, innovation, recipients and context, with facilitation represented as the active element assessing, aligning and integrating the other three constructs (Harvey & Kitson, 2016; Helfrich et al, 2010; Kitson, Harvey, & McCormack, 1998). |
|
Theoretical Domains Framework (TDF) |
Based on psychological theories of behavior change and organizational theories, the TDF sets forth factors that impact decision-making regarding the use of EBPs in clinical care delivery. The TDF is a set of 14 domains covering the main factors influencing practitioner clinical behavior and behavior change (Atkins et al., 2017; Birken et al., 2017; Cane, O’Connor, & Michie, 2012; French et al., 2012). |
|
Normalization Process Theory (NPT) |
A mid-range sociological theory that focuses on the contributions of social action to implementation, embedding and integration of EBPs. The NPT offers a set of mechanism based explanations for processes of implementation, embedding and integration. Practices become routinely embedded – or normalized – in social contexts as the result of people working, individually and collectively, to enact them (May, 2013; May et al., 2009; May, Johnson, & Finch, 2016; McEvoy et al., 2014). |
|
RE-AIM |
The RE-AIM framework was originally designed to plan and evaluate implementation of public health EB programs or interventions. RE-AIM focuses on five dimensions: Reach, Effectiveness, Adoption, Implementation and Maintenance. Today, RE-AIM is used in the planning stages for implementation in diverse areas of healthcare (e.g., health promotion, disease prevention, disease management) and settings (e.g., communities, hospitals, primary care, schools) as well as reporting results of implementing EBPs. (Gaglio, Shoup, & Glasgow, 2013; Glasgow et al., 1999; Kessler et al., 2013). |
|
Knowledge to Action (KTA) Framework |
The KTA Framework is intended to help those concerned with knowledge translation deliver sustainable, evidence-based interventions. Knowledge translation is defined as a process that includes synthesis, dissemination, exchange and ethically sound application of knowledge to improve health, provide more effective health services and products and strengthen the healthcare system. The KTA Framework includes two components: Knowledge Cycle and the Action Cycle. Each component involves several phases which overlap and can be iterative. The Action Cycle represents activities needed for knowledge to be applied in practice (Field, Booth, Ilott, & Gerrish, 2014; Graham et al. 2006). |
|
Diffusion of Innovations |
A classic sociological-cognitive theory of mechanisms of adoption and use of innovations by individuals and groups. This theory has informed many models of EBP and implementation science (Rogers, 2003; Dearing, 2009). |
|
Behavior Change Wheel (BCW) Framework |
Developed from critical analysis of 19 frameworks of behavior change. At the hub/center of the BCW is a behavior system involving 3 essential conditions: capability, opportunity, and motivation. Surrounding the hub are nine intervention functions (e.g. education, persuasion) that are aimed to address the deficits in one or more of these conditions. The outer wheel surrounds the intervention functions and consists of seven categories of policy (e.g. communication/marketing, fiscal) that could enable those interventions to occur (Hendriks et al., 2013; Mangurian et al., 2017; Michie, van Stralen, & West, 2011). |
|
Consolidated Framework for Implementation Research (CFIR) |
A meta-theoretical framework of 39 implementation-related constructs organized across five major domains (intervention, inner setting, outer setting, individuals, process) which interact to influence implementation and implementation effectiveness (Birken et al., 2017; Damschroder et al., 2009; Kirk et al., 2016). |
|
Context and Implementation of Complex Interventions (CICI) framework |
The CICI framework comprises three dimensions—context, implementation and setting—which interact with one another and with the health/clinical intervention dimension. Context comprises seven domains such as socio-cultural, socio-economic, and ethical. Implementation consists of five domains such as strategies and outcomes, and setting refers to the specific physical location in which the intervention is put into practice. The intervention and the way it is implemented in a given setting and context can occur on a micro, meso, and macro level (Pfadenhauer et al., 2017). |
|
Translation Research Model |
An implementation model based on Rogers' (2003) seminal work on diffusion of innovations, to guide selection of implementation strategies for testing the effectiveness of single or multifaceted implementation interventions. The TRM focuses on characteristics of the innovation and how the innovation is communicated to users in their social context (Titler et al., 2009; Titler, 2010; Titler et al., 2016). |
|
Iowa Model of EBP to Improve the Quality of Care |
An action oriented model to guide clinicians in the steps of evidence-based practice from selection of a clinical focus through evaluation (Titler et al., 2001). |
An issue in translation science is how these theories are applied.An issue in translation science is how these theories are applied. Application of these theories is meant to facilitate the identification of determinants of implementation, guide the selection of implementation strategies, and inform all phases of the research, including the constructs to be measured and the relationships among constructs to be tested (Birken, Powell, Shea et al., 2017). Several implementation scientists have noted, however, that these theories are not used, are used superficially, or are misused in translation science (Birken, Powell, Shea et al., 2017; Davies, Walker & Grimshaw, 2010; Gaglio et al., 2013; Kirk et al., 2016; Tinkle, Kimball, Haozous, Shuster, & Meize-Grochowski, 2013). This poses a substantial challenge for generalizing findings across diverse settings.
Implementation Strategies
There are multiple implementation strategies that have been tested and/or used for promoting adoption of EBPs. Implementation is a dynamic, iterative process. There are multiple implementation strategies that have been tested and/or used for promoting adoption of EBPs (Colquhoun et al., 2014; Colquhoun, Squires, Kolehmainen, Fraser, & Grimshaw, 2017; Grimshaw, Eccles, Lavis, Hill, & Squires, 2012; Lokker et al., 2015; McCormack et al., 2013; Michie, Atkins & West, 2014; Rycroft-Malone et al., 2012; Scott et al., 2012). The Translation Research Model (TRM), based on Rogers’ (2003) seminal work on diffusion of innovations, is useful for guiding selection of implementation strategies (Titler & Everett, 2001; Titler et al., 2009; Titler et al., 2016). According to this model (see Figure 1), adoption of EBPs is influenced by four key areas:
- The nature of the innovation (e.g., the type and strength of evidence, the clinical topic)
- The manner in which the innovation is communicated
- To members (e.g., clinicians; users of the EBPs)
- In the social system (organization, patient care unit)
Successful implementation requires strategies to address each of these four areas (Titler, 2010; Titler et al., 2016). Table 3 provides examples of implementation strategies organized by the four components of the TRM.
Figure 1. Translation Research Model (Figure used with permission)
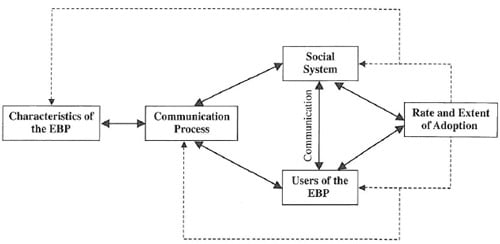
Table 3. Examples of Implementation Strategies for each Component of the Translation Research Model
|
TRM Component: Characteristics of the Innovation/Clinical Topic |
||
|
Implementation Strategy |
Description |
Considerations |
|
Quick Reference Guides (QRGs) |
QRGs give targeted, concise information designed to help practitioners make decisions & perform specific tasks. Examples: checklists; wallet cards |
If the new EBP is complex, QRGs can be used to reduce the complexity which may contribute to slow adoption. Characteristics of good QRGs include clarity, accuracy and accessibility. Careful editing is needed to distill the necessary information for clinicians. |
|
Clinical decision-support tools |
Visual representation of the EB care processes with decision points and information to guide decision-making. Example: Algorithms |
A variety of CDS tools can be imbedded in the EHR, including alerts, reminders, orders sets or care plans. Empirical support for the effectiveness of CDS tools embedded in electronic health records is mixed |
|
Key messages at the point of care delivery |
Reminders about an EBP posted at the point of care. Distilling the essence of the EBP to a few key points on signs, posters. Examples: posters, infographics, visual abstracts. |
Selection of key messages to ease adoption includes consideration of the knowledge of the end users, & the context in which they will be used. |
|
TRM Component: Users of the EBP |
||
|
Implementation Strategy |
Description |
Considerations |
|
Performance gap assessment |
Baseline practice performance indicators/metrics that provides information about the state of current practices at the beginning of a practice change. |
Practice indicators are derived from the EBP recommendations for the specified topic & should include process & outcome indicators |
|
Audit and feedback |
Ongoing auditing of performance indicators, aggregating data into reports, and discussing the findings with practitioners on a regular basis during the practice change. |
Select performance indicators to be audited, data sources, methods for displaying data & providing feedback to staff, frequency of data feedback, and venue for discussing reports. |
|
TRM Component: Communication |
||
|
Implementation Strategy |
Description |
Considerations |
|
Education |
Education of clinicians about the EBPs is necessary but not sufficient to change practice and didactic continuing education alone does little to change practice behaviors. |
It is essential that clinicians delivering the EBPs have the knowledge and skills necessary to deliver the EBPs. |
|
Opinion leaders (OLs) |
OLs are individuals from the local peer group who are viewed as a respected source of influence, considered by their peer group as competent, & trusted to judge the fit between the EBPs and the local practice setting |
OLs are informal leaders who are able to influence other individuals’ attitudes or overt behavior in a desired way with relative frequency. They are visible and communicate with others via their interpersonal networks. |
|
Change champions (CCs) |
Change champions are practitioners within the patient care unit/clinic who are expert clinicians and have positive working relationships with their peers. |
Interpersonal communication with colleagues is a preferred source of practice knowledge for staff. Actions of CC include 1:1 education and mentoring, auditing EBP performance indicators, making changes in organizational documents to incorporate EBP recommendations |
|
Educational outreach/academic detailing |
Face-to-face interaction with clinicians in their practice setting by an individual (usually a clinician) with expertise about the EBPs. Academic detailers are able to explain the research base for the EBPs & respond convincingly to clinician questions, & challenges. |
Consider who will perform this role and the frequency of outreach during implementation. The person performing this role should be consistent – a consistent individual with a consistent message. |
|
TRM Component: Social System |
||
|
Implementation Strategy |
Description |
Considerations |
|
Environmental scan |
Assessment of internal strengths and challenges for implementation of EBPs. Environmental scans include the structure and function of the organization. |
Consider the governance structure & function with respect to the committees that govern standards of practice & quality improvement. Delineate how the EBPs contribute to the organizational strategic initiatives. |
|
Engagement with key leaders |
Meet with senior organizational leaders to describe the EBPs & the contribution to improving quality of care. Include nurse managers &/or medical directors of sites where EBPs will be implemented. |
Decide on methods for keeping senior leaders informed throughout implementation. Seek their input to overcome challenges. |
|
Standards of practice & documentation systems |
Revisions in standards of practice & documentation systems may be needed to reflect the changes in practice & the evidence-base. |
Documentation systems that fail to readily support the EBPs thwart change. Standards of practice should reflect the evidence references. |
|
Recognition |
Formal or informal actions that recognize staff for their efforts with implementing EBPs. Examples: Highlighting work in local newsletter; personnel thank you notes. |
Consider nominating individuals or teams for practice excellence awards offered by the health system, or professional organizations. |
|
Rewards |
Some form of monetary compensation. Examples: bonus payments, salary increases, provision of educational funds. |
Consider providing financial support for an individual or team to attend a regional or national conference to present their work. |
Issues regarding implementation strategies in translation science include lack of agreement about naming of the implementation intervention and/or strategy (ontology); inconsistencies in the descriptions of interventions and their content; lack of an agreed upon classification system or taxonomy of implementation interventions; lack of clarity regarding the target of the intervention (e.g., organization, clinicians, teams of practitioners, or some combination thereof); description of the intervention dose; and selection and measurement of the primary end-points for determining effectiveness (Alexander & Hearld, 2012; Bornbaum, Kornas, Peirson, & Rosella 2015; Colquhoun et al., 2014; Grimshaw et al., 2012; Lokker et al., 2015; Martinez, Lewis, & Weiner, 2014; Titler & Shuman, 2017). These issues continue to be debated among investigators and are not uncommon in a young, transdisciplinary area of science.
Context and Implementation
Context matters and is widely acknowledged as an important influence on implementation outcomes.Context matters and is widely acknowledged as an important influence on implementation outcomes (Birken et al., 2016; Jacobs, Weiner, & Bunger, 2014; May, 2013; May et al., 2016). Context for implementation of EBPs has traditionally been defined as the physical setting, with little attention to the dynamics of the practice environment (Chambers, Glasgow, & Stange, 2013; May, Johnson, & Finch, 2016). Context refers to the characteristics of the setting of implementation and the social dynamic factors in which implementation processes occur (May et al., 2016; Squires et al., 2015). Setting encompasses the structural factors, such as the physical or operational characteristics of the setting (e.g., staffing, unit size, types of patients) (Birken, Powell, Presseau et al., 2017; May et al., 2016). Social dynamic factors pertain to the roles, relationships, and dynamics of the individuals and groups within a practice setting (Birken, Powell, Presseau et al., 2017; May et al., 2016). Context factors that impact implementation include:
- Organizational capacity for EBP
(Birken, Bungner, Powell et al., 2017; Doran et al., 2012; French et al., 2009; Kueny et al., 2015; May, et al., 2016; Stetler, Ritchie, Rycroft-Malone, Schultz, & Charns 2009; Yamada et al., 2017); - Leadership support
(Aarons, Ehrhart, Farahnak, & Sklar, 2014; Birken et al., 2016; Hauck, Winsett, & Kuric, 2012; Jun, Kovner, & Stimpfel, 2016; Richter et al., 2016; Wong & Giallonardo, 2013); - Practice climates for use of EBPs
(Jacobs et al., 2014; Shuman, Powers, Liu, & Titler, 2018; Yamada et al., 2017); and - EBP competencies of staff and nurse managers
(Gifford, Davies, Edwards, Griffin, & Lybanon, 2007; Shuman et al., 2017; Shuman, Powers et al., 2018)
Investigators studying implementation should incorporate these dynamic context factors into their research. Implementation studies have traditionally included structural factors that influence adoption of EBPs but few studies have included the social dynamic factors, such as organizational capacity, EBP leadership behaviors, and climate for EBP implementation (Shuman, Powers et al., 2018). Instruments are available to assess a variety of context factors (Chaudoir, Dugan, & Barr, 2013; Titler & Anderson, in press). For example, the Implementation Climate Scale (ICS) is a reliable and valid instrument consisting of 18 items that evaluates the extent (1= slight extent to 4 = very great extent) that the unit/practice setting prioritizes and values EBP. All items are anchored to a specific practice setting as a point of reference (Ehrhart, Aarons, & Farahnak, 2014).
Investigators studying implementation should incorporate these dynamic context factors into their research. Incorporating measures such as these into implementation studies will provide insights into why some implementation strategies work in some settings and not others, and the mechanisms underlying the effectiveness of these strategies. We are unlikely to close the critical gap between research and practice if studies do not examine the interplay between dynamic context factors and the implementation strategies used to promote uptake of EBPs.
Results of the assessment can be examined for opportunities to strengthen organizational capacity for EBP and to guide organizational interventions/programs... In addition, context factors that impact implementation should be routinely assessed by healthcare systems to build strong organizational capacity for adoption of EBPs. Results of the assessment can be examined for opportunities to strengthen organizational capacity for EBP and to guide organizational interventions/programs to address these areas of opportunity. For example, if scores for hiring staff that value EBP are low, an organization may want to examine hiring practices and interview questions used in selection of staff.
Conclusion
Translation science is a relatively new area of investigation and nurse scientists are setting directions in this field. Nurse scientists have a rich history and are making major contributions to EBP and translation science. Translation science is a relatively new area of investigation and nurse scientists are setting directions in this field. An overview of terminology, examples of theories and models of translation science, descriptions of various implementation strategies, and the importance of context in implementation science have been presented. Challenges noted include diversity of terminology associated with translation science, multiple theoretical models with inconsistent or underuse to guide implementation research, lack of agreement of an ontology and taxonomy of implementation strategies, underdeveloped methods for calculating implementation intervention dose, and controversies regarding methods for measurement of implementation effectiveness. Dynamic context factors are emerging as an important area to address in implementation research. This field of investigation continues to provide multiple opportunities for nurse scientists and practicing clinicians to address application of evidence in practice to improve care delivery, patient outcomes, and population health.
Authors
Marita G. Titler, PhD, RN, FAAN
Email: mtitler@med.umich.edu
Dr. Marita G. Titler is a Professor, the Rhetaugh G. Dumas Endowed Chair, and the Department Chair of Systems, Populations and Leadership in the University of Michigan, School of Nursing. Her program of research is in outcomes effectiveness and implementation science and is supported by federal and foundation funding. She has been PI on five funded translation and outcomes effectiveness studies, and co-investigator on numerous other funded investigations. Dr. Titler is the PI of the T32 institutional training grant Complexity: Innovations in Promoting Health and Safety (T32 NR016914). She has published over 150 papers in referred journals including Medical Care, Health Services Research, and Implementation Science. She has served on national committees including the National Advisory Council for AHRQ, and the Committee on Standards for Developing Trustworthy Clinical Practice Guidelines for the Institute of Medicine. She is a member of the National Academy of Medicine and has received numerous awards for her work including the American Organization of Nurse Executives National Researcher Award, the Sigma Theta Tau International Elizabeth McWilliams Miller Award, and the President’s award from the Friends of NINR.
References
Aarons, G.A., Ehrhart, M.G., Farahnak, L.R., & Sklar, M. (2014). Aligning leadership across systems and organizations to develop a strategic climate for evidence-based practice implementation. Annual Review of Public Health, 35, 255–274. doi:10.1146/annurev-publhealth-032013-182447
Alexander, J.A., & Hearld, L.R. (2012). Methods and metrics challenges of delivery-system research. Implementation Science, 7(15). doi:10.1186/1748-5908-7-15
Armstrong, R., Waters, E., Dobbins, M., Anderson, L., Moore, L., Petticrew, M., … Swinburn, B. (2013). Knowledge transition strategies to improve the use of evidence in public health decision making in local government: Intervention design and implementation plan. Implementation Science, 8(1), 121–131. doi:10.1186/1748-5908-8-121
Atkins, L., Francis, J., Islam, R., O’Connor, D., Patey, A., Ivers, N., … Michie, S. (2017). A guide to using the Theoretical Domains Framework of behavior change to investigate implantation problem. Implementation Science, 12(77). doi:10.1186/s13012-017-0605-9
Birken, S.A., Bunger, A.C., Powell, B.J., Turner, K., Clary, A.S., Klaman, S.L., … Weiner, B.J. (2017). Organizational theory for dissemination and implementation research. Implementation Science 12(62). doi:10.1186/s13012-017-0592-x
Birken, S.A., DiMartino, L.D., Kirk, M.A., Lee, S.Y.D., McClelland, M., & Albert, N.M. (2016). Elaborating on theory with middle managers’ experience implementing healthcare innovations in practice. Implementation Science, 11(2). doi:10.1186/s13012-015-0362-6
Birken, S.A., Powell, B.J., Presseau, J., Kirk, M.A., Lorencatto, F., Gould, N.J., … Damschroder, L.J. (2017). Combined use of the Consolidated Framework for Implementation Research (CFIR) and the Theoretical Domains Framework (TDF): A systematic review. Implementation Science, 12(2). doi:10.1186/s13012-016-0534-z
Birken, S.A., Powell, B.J., Shea, C.M., Haines, E.R., Kirk, M.A., Leeman, J., … Presseau, J. (2017). Criteria for selecting implementation science theories and frameworks: Results from an international survey. Implementation Science, 12(124). doi:10.1186/s13012-017-0656-y
Bornbaum, C.C., Kornas, K., Peirson, L., & Rosella, L.C. (2015). Exploring the function and effectiveness of knowledge brokers as facilitators of knowledge translation in health-related settings: A systematic review and thematic analysis. Implementation Science, 10(162). doi:10.1186/s13012-015-0351-9
Brownson, R.C., Chriqui, J.F., & Stamatakis, K.A. (2009). Understanding the evidence-based public health policy. American Journal of Public Health, 99(9), 1576–1583. doi:10.2105/AJPH.2008.156224
Canadian Institutes of Health Research (CIHR). (2017). Knowledge translation. Retrieved from http://www.cihr-irsc.gc.ca/e/29529.html
Cane, J., O’Connor, D., & Michie, S. (2012). Validation of the theoretical domains framework for use in behavior change and implementation research. Implementation Science, 7(37). doi:10.1186/1748-5908-7-37
Centers for Disease Control and Prevention (CDC). (2016, May 2). Centers for Disease Control and Prevention. Retrieved from http://www.cdc.gov
Chambers, D.A., Glasgow, R.E., & Stange, K.C. (2013). The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implementation Science, 8(1), 117. doi:10.1186/1748-5908-8-117
Chaudoir, S.A., Dugan, A.G., & Barr, C.H. (2013). Measuring factors affecting implementation of health innovations: A systematic review of structural, organizational, provider, patient, and innovation level measures. Implementation Science, 8(22). doi: https://doi.org/10.1186/1748-5908-8-22
Colquhoun, H., Leeman, J., Michie, S., Lokker, C., Bragge, P., Hempel, S., … Grimshaw, J. (2014). Towards a common terminology: A simplified framework of interventions to promote and integrate evidence into health practices, systems, and policies. Implementation Science, 9(781). doi:10.1186/1748-5908-9-51
Colquhoun, H.L., Squires, J.E., Kolehmainen, N., Fraser, C., & Grimshaw, J.M. (2017). Methods for designing interventions to change healthcare professionals’ behaviour: A systematic review. Implementation Science, 12(1), 30. doi:10.1186/s13012-017-0560-5
Conway, L.J., Pogorzelska, M., Larson, E., & Stone, P.W. (2012). Adoption of policies to prevent catheter-associated urinary tract infections in United States intensive care units. American Journal of Infection Control, 40(8), 705–710. doi:10.1016/j.ajic.2011.09.020
Cronenwett, L.R. (1995). Effective methods for disseminating research findings to nurses in practice. Nursing Clinics of North America, 30(3), 429–438.
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4(50). doi:10.1186/1748-5908-4-50
Davies, P., Walker, A.E., Grimshaw, J.M. (2010). A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations.Implementation Science, 5(1), 14. doi:10.1186/1748-5908-5-14
Dearing, J.W. (2009). Applying diffusion of innovation theory to intervention development. Research on Social Work Practice, 19(5), 503–518. doi:10.1177/1049731509335569
Department of Health and Human Services (2018). Dissemination and implementation research in health. Retrieved from https://grants.nih.gov/grants/guide/pa-files/par-16-238.html
Dickinson, S., & Shever, L.L. (2012). Evidence-based nursing innovations. Critical Care Nursing Quarterly, 35(1), 1. doi:10.1097/CNQ.0b013e31823d6d3f
Dobbins, M., Hanna, S.E., Ciliska, D., Manske, S., Cameron, R., Mercer, S.L., … Robeson, P. (2009). A randomized controlled trial evaluating the impact of knowledge translation and exchange strategies. Implementation Science, 4(1), 61–77.
Doran, D., Haynes, B.R., Estabrooks, C.A., Kushniruk, A., Dubrowski, A., Bajnok, I., … Bai, Y.Q. (2012). The role of organizational context and individual nurse characteristics in explaining variation in use of information technologies in evidence based practice. Implementation Science, 7(122). doi:10.1186/1748-5908-7-122
Eccles, M.P., & Mittman, B.S. (2006). Welcome to implementation science. Implementation Science, 1(1), 1–3.
Ehrhart, M.G., Aarons, G.A., & Farahnak, L.R. (2014). Assessing the organizational context for EBP implementation: The development and validity testing of the Implementation Climate Scale (ICS). Implementation Science, 9(157). doi:10.1186/s13012-014-0157-1
Estabrooks, C.A., Derksen, L., Winther, C., Lavis, J.N., Scott, S.D., Wallin, L., & Profetto-McGrath, J. (2008). The intellectual structure and substance of the knowledge utilization field: A longitudinal author co-citation analysis, 1945–2004. Implementation Science, 3(1), 49–70.
Field, B., Booth, A., Ilott, I., & Gerrish, K. (2014). Using the knowledge to action framework in practice: A citation analysis and systematic review. Implementation Science, 9(172). doi:10.1186/s13012-014-0172-2
French, B., Thomas, L.H., Baker, P., Burton, C.R., Pennington, L., & Roddam, H. (2009). What can management theories offer evidence-based practice? A comparative analysis of measurement tools for organisational context. Implementation Science, 4(28). doi:10.1186/1748-5908-4-28
French, S.D., Green, S.E., O’Connor, D.A., McKenzie, J.E., Francis, J.J., Michie, S., … Grimshaw, J.M. (2012). Developing theory-informed behaviour change interventions to implement evidence into practice: A systematic approach using the Theoretical Domanis Framework. Implementation Science, 7(38). doi:10.1186/1748-5908-7-38
Funk, S.G., Tornquist, E.M., & Champagne, M.T. (1989). A model for improving the dissemination of nursing research. Western Journal of Nursing Research, 11(3), 361–367.
Gaglio, B., Shoup, J.A., & Glasgow, R.E. (2013). The RE-AIM framework: A systematic review of use over time. American Journal of Public Health, 103(6), e38–e46. doi:10.2105/AJPH.2013.301299
Gifford, W., Davies, B., Edwards, N., Griffin, P., & Lybanon, V. (2007). Managerial leadership for nurses' use of research evidence: An integrative review of the literature. Worldviews on Evidence-Based Nursing, 4(3), 126–145. doi:10.1111/j.1741-6787.2007.00095.x
Glasgow, R.E., Vogt, T.M., & Boles, S.M. (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89(9), 1322–1327. doi:10.2105/AJPH.89.9.1322
Graham, I.D., Logan, J., Harrison, M.B., Straus, S.E., Tetroe, J., Caswell, W., & Robinson, N. (2006). Lost in knowledge translation: Time for a map? Journal of Continuing Education in the Health Professions, 26(1), 13–24. doi:10.1002/chp.47
Grimshaw, J.M., Eccles, M.P., Lavis, J.N., Hill, S.J., & Squires, J.E. (2012). Knowledge translation of research findings. Implementation Science, 7(1), 50. doi: http://dx.doi.org/10.1186/1748-5908-7-50
Harvey, G., & Kitson, A. (2016). PARIHS revisited: From heuristic to integrated framework for successful implementation of knowledge into practice. Implementation Science, 11(33). doi:10.1186/s13012-016-0398-2.
Hauck, S., Winsett, R.P., & Kuric, J. (2012). Leadership facilitation strategies to establish evidence-based practice in an acute care hospital. Journal of Advanced Nursing, 69(3), 664–674. doi:10.1111/j.1365-2648.2012.06053.x
Helfrich, C.D., Damschroder, L.J., Hagedorn, H.J., Daggett, G.S., Sahay, A., Ritchie, M., … Stetler, C.B. (2010). A critical synthesis of literature on the promoting action on research implementation in health services (PARIHS) framework. Implementation Science, 5(82). doi:10.1186/1748-5908-5-82
Hendriks, A.-M., Jansen, M.W.J., Gubbels, J.S., De Vries, N.K., Paulussen, T., & Kremers, S.P.J. (2013). Proposing a conceptual framework for integrated local public health policy, applied to childhood obesity—The behavior change ball. Implementation Science, 8, 46–62. doi:10.1186/1748-5908-8-46
Henly, S., McCarthy, D., Wyman, J., Heitkemper, M., Redeker, N., Titler, M.G., … Dunbar-Jacob, J. (2015). Emerging areas of science: Recommendations for nursing science education from the Council for the Advancement of Nursing Science Idea Festival. Nursing Outlook. 63(4), 398–407. doi:10.1016/j.outlook.2015.04.007
Horsley, J.A. (1983) Using research to improve nursing practice: A guide. Austin, TX: Pro-Ed.
IOM (Institute of Medicine). (2013a). Establishing transdisciplinary professionalism for improving health outcomes: Workshop summary. Washington, D.C.: The National Academies Press. Retrieved from http://dept-wp.nmsu.edu/geriatriceducation/files/2014/03/Workshop-Summary.pdf
IOM (Institute of Medicine). (2013b). The CTSA program at NIH: Opportunities for advancing clinical and translational research. Washington, D.C.: The National Academies Press. Retrieved from http://www.nationalacademies.org/hmd/Reports/2013/The-CTSA-Program-at-NIH-Opportunities-for-Advancing-Clinical-and-Translational-Research.aspx
IOM (Institute of Medicine). (2012a). For the public’s health: Investing in a healthier future. Washington, D.C.: The National Academies Press. Retrieved from https://www.nap.edu/catalog/13268/for-the-publics-health-investing-in-a-healthier-future
IOM (Institute of Medicine). (2012b). Living well with chronic illness: A call for public health action. Washington, D.C.: The National Academies Press. Retrieved from http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2012/Living-Well-with-Chronic-Illness/livingwell_chronicillness_reportbrief.pdf
IOM (Institute of Medicine). (2011a). Clinical practice guidelines we can trust. Washington, D.C.: The National Academies Press. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK209539/
IOM (Institute of Medicine). (2011b). The future of nursing: Leading change, advancing health. Washington, D.C.: The National Academies Press. Retrieved from https://www.nap.edu/catalog/12956/the-future-of-nursing-leading-change-advancing-health
IOM (Institute of Medicine). (2009). Initial national priorities for comparative effectiveness research. Washington, D.C.: The National Academies Press. Retrieved from https://www.nap.edu/catalog/12648/initial-national-priorities-for-comparative-effectiveness-research
Jacobs, S.R., Weiner, B.J., & Bunger, A.C. (2014). Context matters: Measuring implementation climate among individuals and groups. Implementation Science, 9(1), 46. doi:10.1186/1748-5908-9-46
Jun, J., Kovner, C.T., & Stimpfel, A.W. (2016). Barriers and facilitators of nurses’ use of clinical practice guidelines: An integrative review. International Journal of Nursing Studies, 60, 54–68. doi:10.1016/j.ijnurstu.2016.03.006
Kelley, P.W. (2010). Research to practice in the military healthcare system. Nursing Research, 59(1), S1. doi:10.1097/NNR.0b013e3181c9764d
Kessler, R.S., Purcell, E.P., Glasgow, R.E., Klesges, L.M., Benkeser, R.M., & Peek, C.J. (2013). What does it mean to “employ” the RE-AIM model? Evaluation and the Health Professions, 36(1). doi:10.1177/0163278712446066
King, D., Barnard, K.E., and Hoehn, R. (1981). Disseminating the results of nursing research. Nursing Outlook, 29(3), 164–169.
Kirk, M.A., Kelley, C., Yankey, N., Birken, S.A., Abadie, B., Damschroder, L. (2016). A systematic review of the use of the consolidated framework for implementation research. Implementation Science, 11(72). doi:10.1186/s13012-016-0437-z
Kitson, A., Harvey, G., & McCormack, B. (1998). Enabling the implementation of evidence based practice: A conceptual framework. Quality in Health Care, 7(3), 149–158. doi:10.1136/qshc.7.3.149
Krueger, J.C. (1978). Utilization of nursing research: The planning process. Journal of Nursing Administration, 8(1), 6–9.
Krueger, J.C., Nelson, A.H., & Wolanin, M.O. (1978). Nursing research: Development, collaboration, and utilization. Germantown, MD: Aspen.
Kueny, A., Shever, L., Lehan Mackin, M., & Titler, M.G. (2015). Facilitating the implementation of evidence-based practice through contextual support for nursing leadership. Journal of Healthcare Leadership, 7, 29–39. doi:10.2147/JHL.S45077
Lindeman, C.A., & Krueger, J.C. (1977). Increasing the quality, quantity, and use of nursing research. Nursing Outlook, 25(7), 450–454.
LoBiondo-Wood, G., & Haber, J. (2018). Integrating research, evidence-based practice, and quality improvement processes. In G. LoBiondo-Wood & J. Haber (Eds.), Nursing research: Methods and critical appraisal for evidence-based practice (9th edition, pp. 5–22). St. Louis, MO: Elsevier.
Lokker, C., McKibbon, K.A., Colquhoun, H., & Hempel, S. (2015). A scoping review of classification schemes of interventions to promote and integrate evidence into practice in healthcare. Implementation Science, 10, 27–39. doi:10.1186/s13012-015-0220-6
Mangurian, C., Niu, G.C., Schillinger, D., Newcomer, J.W., Dilley, J., & Handley, M.A. (2017). Utilization of the behavior change wheel framework to develop a model to improve cardiometabolic screening for people with severe mental illness. Implementation Science, 12(134). doi:10.1186/s13012-017-0663-z
Mark, D.B., Titler, M.G., & Latimer, R.W. (Eds.). (2014). Integrating evidence into practice for impact. Nursing Clinics of North America, 49(3), 269–452. Retrieved from https://www.sciencedirect.com/journal/nursing-clinics-of-north-america/vol/49/issue/3
Martinez, R.G., Lewis, C.C., & Weiner, B.J. (2014). Instrumentation issues in implementation science. Implementation Science, 9(118). doi:10.1186/s13012-014-0118-8
May, C. (2013). Towards a general theory of implementation. Implementation Science, 8(18). doi:10.1186/1748-5908-8-18
May, C.R., Johnson, M., & Finch, T. (2016). Implementation, context and complexity. Implementation Science, 11(1), 141. doi:10.1186/s13012-016-0506-3
May, C.R., Mair, F., Finch, T., MacFarlane, A., Dowrick, C., Treweek, S., … Victor, M. (2009). Development of a theory of implementation and integration: Normalization process theory. Implementation Science, 4(29). doi:10.1186/1748-5908-4-29
McCormack, B., Rycroft-Malone, J., DeCorby, K., Hutchinson, A.M., Bucknall, T., Kent, B., Schultz, A., … Wilson, V. (2013). A realist review of interventions and strategies to promote evidence-informed healthcare: A focus on change agency. Implementation Science, 8(107). doi:10.1186/1748-5908-8-107
McEvoy, R., Ballini, L., Maltoni, S., O’Donnell, C.A., Mair, F.S., & MacFarlane, A. (2014). A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implementation Science, 9(2). doi:10.1186/1748-5908-9-2
McKibbon, K.A., Lokker, C., Wilczynski, N.L., Ciliska, D., Dobbins, M., Davis, D.A., Haynes, R.B., & Straus, S.E. (2010). A cross-sectional study of the number and frequency of terms used to refer to knowledge translation in a body of health literature in 2006: A Tower of Babel? Implementation Science, 5, 16–27. doi:10.1186/1748-5908-5-16
Michie, S., Atkins, L., & West, R. (2014). The behavior change wheel: A guide to designing interventions. London, UK: Silverback Publishing.
Michie, S., van Stralen, M.M., & West, R. (2011). The behaviour change wheel: A new method for characterizing and designing behavior change interventions. Implementation Science, 6(42). doi:10.1186/1748-5908-6-42
National Academies of Sciences, Engineering and Medicine (NAM). (2015). Assessing progress on the Institute of Medicine report: The future of nursing. Washington, DC: The National Academies Press. Retrieved from https://www.nap.edu/catalog/21838/assessing-progress-on-the-institute-of-medicine-report-the-future-of-nursing
Newhouse, R., Bobay, K., Dykes, P.C., Stevens, K.R., & Titler, M.G. (2013). Methodology issues in implementation science. Medical Care, 51(4), S32–S40.
Nightingale, F. (1863a). Notes on hospitals. London, UK: Longman, Green, Roberts, & Green.
Nightingale, F. (1863b). Observation on the evidence contained in the statistical reports submitted by her to the Royal Commission on the sanitary state of the army in India. London, UK: Edward Stanford.
Nightingale, F. (1859). A contribution to the sanitary history of the British Army during the late war with Russia.London: John W. Parker & Sons.
Nightingale, F. (1858). Notes on matters affecting the health, efficiency, and hospital administration of the British Army. London: Harrison & Sons.
Nilsen, P. (2015). Making sense of implementation theories, models and frameworks. Implementation Science, 10(53). doi:10.1186/s13012-015-0242-0
Pfadenhauer, L.M., Gerhardus, A., Mozygemba, K., Lysdahl, K.B., Booth, A., Hofmann, B., … Rehfuess, E. (2017). Making sense of complexity in context and implementation: The Context and Implementation of Complex Interventions (CICI) framework. Implementation Science, 12(1), 21. doi:10.1186/s13012-017-0552-5
Purtle, J., Peters, R., & Brownson, R.C. (2016). A review of policy dissemination and implementation research funded by the National Institutes of Health, 2007–2014. Implementation Science, 11(1), 1–8. doi:10.1186/s13012-015-0367-1
Richter, A., von Thiele Schwarz, U., Lornudd, C., Lundmark, R., Mosson, R., & Hasson, H. (2016). iLead—A transformational leadership intervention to train healthcare managers’ implementation leadership. Implementation Science, 11(1), 108. doi:10.1186/s13012-016-0475-6
Rogers, E.M. (2003). Diffusion of innovations (5th edition). New York, NY: The Free Press.
Rutledge, D.N. & Donaldson, N.E. (1995). Building organizational capacity to engage in research utilization. Journal of Nursing Administration, 25(10), 12–16.
Rycroft-Malone, J., McCormack, B., Hutchinson, A.M., DeCorby, K., Bucknall, T.K., Kent, B., … Wilson, V. (2012). Realist synthesis: Illustrating the method for implementation research. Implementation Science 7(33). doi:10.1186/1748-5908-7-33.
Scott, S.D., Albrecht, L., O’Leary, K., Ball, G.D.C., Hartling, L., Hofmeyer, A., … Dryden, D.M. (2012). Systematic review of knowledge translation strategies in the allied health professions. Implementation Science, 7(70). doi:10.1186/1748-5908-7-70
Shever, L.L., & Dickinson, S. (2013). Mobility: A successful investment for critically ill patients. Foreword. Critical Care Nursing Quarterly, 36(1), 1–2. doi:10.1097/CNQ.0b013e3182750631
Shever, L.L., Titler, M.G., Mackin, M.L., & Kueny, A. (2011). Fall prevention practices in adult medical-surgical nursing units described by nurse managers. Western Journal of Nursing Research, 33(3), 385–397. doi:10.1177/0193945910379217
Shuman, C.J., Ploutz-Snyder, R., & Titler, M.G. (2018). Development and testing of the NM EBP Competency Scale. Western Journal of Nursing Research, 40(2), 175-190doi:10.1177/0193945917728249
Shuman, C., Powers, K., Liu, X., & Titler, M.G. (2018). Unit leadership and climates for evidence-based practice implementation in acute care: A cross-sectional descriptive study. Journal of Professional Nursing Scholarship, 13(62). doi:10.1186/s13012-018-0753-6
Shuman, C.J., Xie, J., Herr, K., & Titler, M.G. (2017). Sustainability of evidence-based acute pain management practices for hospitalized older adults. Western Journal of Nursing Research. doi:10.1177/0193945917738781
Slaughter, S.E., Hill, J.N., & Snelgrove-Clarke, E. (2015). What is the extent and quality of documentation and reporting of fidelity to implementation strategies: A scoping review. Implementation Science, 109, 129–141. doi:10.1186/s13012-015-0320-3
Squires, D., & Anderson, C. (2015). U.S. health care from a global perspective: Spending, use of services, prices, and health in 13 countries. Issue Brief (Commonwealth Fund), 15, 1–15. Retrieved from http://johngarven.com/blog/wp-content/uploads/2017/07/Spending-Use-of-Services-Prices-and-Health-in-13-Countries-The-Commonwealth-Fund.pdf
Squires, J.E., Graham, I.D., Hutchinson, A.M., Michie, S., Francis, J.J., Sales, A., … Grimshaw, J.M. (2015). Identifying the domains of context important to implementation science: A study protocol. Implementation Science, 10(1), 135. Doi:10.1186/s13012-015-0325-y
Stetler, C.B., Ritchie, J.A., Rycroft-Malone, J., Schultz, A.A., & Charns, M.P. (2009). Institutionalizing evidence-based practice: An organizational case study using a model of strategic change. Implementation Science, 4(1), 78. doi:10.1186/1748-5908-4-78
Straus, E., Richardson, R.B., Glasziou, P., Richardson, W.S., & Haynes, R.B. (2011). Evidence-based medicine: How to practice and teach (4th edition). New York, NY: Elsevier.
Sving, E., Gunningberg, L., Hogman, M., & Mamhidir, A.-G. (2012). Registered nurses’ attention to and perceptions of pressure ulcer prevention in hospital settings. Journal of Clinical Nursing, 21(9–10), 1293–1303. doi:10.1111/j.1365-2702.2011.04000.x
Tinkle, M., Kimball, R., Haozous, E.A., Shuster G., Meize-Grochowski, R. (2013). Dissemination and implementation research funded by the US National Institutes of Health, 2015-2012. Nursing Research and Practice, 2013. doi:10.1155/2013/909606
Titler, M.G. (2014). Overview of evidence-based practice and translation science. Nursing Clinics of North America, 49(3), 269–274. doi:10.1016/j.cnur.2014.05.001
Titler, M.G. (2011). Nursing science and evidence-based practice. Western Journal of Nursing Research, 33(3), 291–295. doi:10.1177/0193945910388984
Titler, M.G. (2010). Translation science and context. Research and Theory for Nursing Practice, 24(1), 35–55.
Titler, M.G. & Anderson, C. (in press). Implementation strategies for stakeholders. In G. Lobiondo-Wood, J. Haber, & M.G. Titler (Eds). Evidence-Based Practice for Nursing and Health Care Quality Improvement. Amsterdam, Netherlands: Elsevier.
Titler, M.G., Conlon, P., Reynolds, M.A., Ripley, R., Tsodikov, A., Wilson, D.S., & Montie, M. (2016). The effect of a translating research into practice intervention to promote use of evidence-based fall prevention interventions in hospitalized adults: A prospective pre-post implementation study in the U.S. Applied Nursing Research, 31, 52–59. doi:10.1016/j.apnr.2015.12.004
Titler, M.G., & Everett, L.Q. (2001). Translating research into practice: Considerations for critical care investigators. Critical Care Nursing Clinics of North America. 13(4), 587–604.
Titler, M.G., Herr, K., Brooks, J., Xie, X-J., Ardery, G., Schilling, M., … Clarke, W. (2009). Translating research into practice intervention improves management of acute pain in older hip fracture patients. Health Services Research, 44(1), 264–287.
Titler, M.G., Kleiber, C., Steelman, V., Rakel, B., Budreau, G., Everett, L.Q., Buckwalter, K.C., Tripp-Reimer, T., & Goode, C. (2001). The Iowa model of evidence-based practice to promote quality care. Critical Care Nursing Clinics of North America. 13(4), 497–509.
Titler, M.G., LoBiondo-Wood, G., & Haber, J. (In press) Evidence-based practice overview. In G. LoBiondo-Wood, J. Haber, & M.G. Titler (Eds.), Evidence-based practice for nursing and health care quality improvement. Amsterdam, Netherlands: Elsevier.
Titler, M.G. & Moore, J. (2010). Evidence-based practice: A civilian perspective [Editorial]. Nursing Research, 59(1), S2–S6.
Titler, M.G., & Shuman, C.S. (2017). Implementation science. In P.A. Grady & A.S. Hinshaw (Eds.), Using nursing research to shape health policy (pp.33-54). New York, NY: Springer Publishing Company.
Titler, M.G., Visovatti, M., Shuman, C., Ellis, K.R., Banerjee, T., Dockham, B., … Northouse, L. (2017). Effectiveness of implementing a dyadic psychoeducational intervention for cancer patients and family caregivers. Supportive Care in Cancer, 25(11), 3395–3406. doi:10.1007/s00520-017-3758-9
Wilson, D.S., Montie, M., Conlon, P., Reynolds, M.A., Ripley, R., & Titler, M.G. (2016). Nurses’ perceptions of implementing fall prevention interventions to mitigate patient-specific fall risk factors. Western Journal of Nursing Research, 38(8), 1012–1034. doi:10.1177/0193945916644995
Wong, C.A., & Giallonardo, L.M. (2013). Authentic leadership and nurse'assessed adverse patient outcomes. Journal of Nursing Management, 21(5), 740–752. doi:10.1111/jonm.12075
Yamada, J., Squires, J.E., Estabrooks, C.A., Victor, S., Stevens, B., & CIHR Team in Children’s Pain. (2017). The role of organizational context in moderating the effect of research use on pain outcomes in hospitalized children: A cross sectional study. BMC Health Services Research, 17(1), 68. doi:10.1186/s12913-017-2029-2

