The concept of being swamped was first described by nurses in a study about hospital nurses’ perceptions of human factors that can contribute to errors by nurses. Being swamped occurs when providers have so much to do that they cannot focus well enough to establish priorities and choose the most important task at hand. In previous studies, being swamped was found to be a primary reason for nurses to make errors. The purpose of this nonexperimental, descriptive study was to explore the experience of swamping in the clinical setting in multiple work units and roles. A survey was developed and tested and data were collected during the fall of 2018. The 13-question survey was distributed via email to employees and providers with inpatient privileges in four large community-based hospitals. Survey findings were evaluated using both quantitative and qualitative analysis methods. A total of 814 participants completed the survey. Only 3.8% of participants noted that they are never swamped, while 11.8% noted that they feel swamped on a daily basis. According to participants, an increase in being swamped leads to missed care, errors, turnover, and delays in care. Being swamped may influence patient satisfaction scores impacting reimbursement and nationally reported data and may result in high turnover because staff feel discouraged and leave.
Key Words: being swamped, patient satisfaction, health workforce, retention, quality of care, patient safety, human subjects, clinical nursing research
The concept of being swamped was first described by nurses in a study about hospital nurses’ perceptions of human factors that can contribute to errors by nurses (Roth et al., 2016). In this study, nurses were asked to identify their beliefs regarding the likelihood, ability to intervene, importance, and commonality of nursing errors. The authors of the study described being swamped as “having so much to do that one is unable to focus on the most important thing” (Roth et al., 2015, p. 177).
Nurses identified swamping in the top two reasons “likely to cause an error,” second only to nurse impaired by a substance. They reported swamping as the number one most important reason and common reason for nursing errors, but the last of 16 reasons in ability for them to intervene.
It is common to hear someone say, “I am swamped,” but use of the term within a clinical context requires investigation.
The Merriam-Webster dictionary (2019) defines “swamp” as a transitive verb meaning (1b) “to overwhelm numerically or by an excess of something: FLOOD.” (paragraph 1). Synonyms include deluge, drown, engulf, inundate, overflow, overwhelm, submerge, and submerse. It is common to hear someone say, “I am swamped,” but use of the term within a clinical context requires investigation. Answers to questions such as what leads to being swamped; how it manifests; how it affects the team members, patients and their families; and what helps when one is feeling swamped, may offer insight in how to improve being swamped in the clinical setting.
Review of Literature
Studies about staff burnout, absenteeism, and poor job performance have been prevalent in the healthcare literature for years (Dyrbye et al., 2019; Shanafelt et al., 2021; Shin et al., 2018). The role of human contributing factors, including fatigue and distress relating to medical errors, has also been studied in nurses (Roth et al. 2016; West et al. 2009). Understanding the part that human factors play in healthcare errors may inform steps to reduce or limit errors. Understanding the part that human factors play in healthcare errors may inform steps to reduce or limit errors.Inattentional blindness (Simons et al. 1999); situational awareness (McManus et al., 2006); missed, delayed, or incomplete care (Simpson et al., 2016); and moral distress (Jameton, 1984) are related to being swamped. Inattentional blindness and situational awareness are the inability to recognize or include factors outside of the primary area of attention; being swamped describes the challenge to establish the area of primary focus among complicating external factors. Being swamped can lead to late or missed elements of care, moral distress, and loss of focus, which may lead to errors and feelings of guilt over what was not accomplished.
being swamped describes the challenge to establish the area of primary focus among complicating external factors.
Various methods have been employed to study the effects of healthcare team members’ workload on the workforce and patient safety with primary emphasis on communication as a mediating factor. Studies that quantified nurse staffing, nurse shifts, and missed care (Simpson et al., 2016; Simpson et al., 2019) found that nurse staffing had significant impact on missed care and patient education. Multiple studies have considered nurse staffing and patient outcomes; findings from these studies have consistently suggested that nurse staffing has a cause and-effect relationship with patient safety (Aiken et al., 2017; Ball et al., 2018; Griffiths et al., 2016; Lake et al., 2017; McHugh et al., 2013; Needleman et al., 2020; Recio-Saucedo et al., 2018; Tubbs-Cooley et al., 2019). The purpose of this study was to explore the experience of swamping in the clinical setting in multiple team roles.
Being swamped in the clinical setting was also studied nationwide for nurse members of the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN) (Roth et al., 2020). This study demonstrated that nurses’ perception of being swamped was significantly decreased in hospital settings where the AWHONN Nurse Staffing Guidelines were followed.
Study Methods
Development of the Survey
The Swamping in the Clinical Setting survey was developed following thematic analysis of the narratives of registered nurses (RNs) who participated in focus groups. Nurses who met to discuss being swamped were employed in the intensive care unit (ICU), emergency department (ED), and the labor and delivery unit (L&D). It is important to note that the focus groups, pilot study, and the four-hospital study reported here were done prior to the COVID-19 pandemic, which is well known to have exacerbated a perception of being overwhelmed among healthcare team members (Haidari et al., 2021).
Focus Groups. Focus groups were utilized to understand the phenomenon of being swamped. Listening to the voices of nurses about swamping served to better understand the experience of being swamped, its prevalence, its impact, mitigation techniques, and the perceived impact on staff, providers, patients, and families. Participants felt strongly that their work life was impacted, however they felt impotent to make change.
Participants felt strongly that their work life was impacted, however they felt impotent to make change.
Survey Psychometric Testing. An expert panel of six raters determined the content validity of the survey tool. Using an electronic assessment form, panel members evaluated the degree of relevancy for each item on the scale as follows: 1 = the item is not relevant to the measured domain, 2 = the item is somewhat relevant to the measured domain, 3 = the item is quite relevant to the measured domain, and 4 = the item is highly relevant to the measured domain. Universal agreement, item level, and scale level content validity index (CVI) scores were calculated.
Raters evaluated items on universal agreement (UA); the UA score across all scale items for the six raters was 0.83. The average proportion of items judged as relevant (I-CVI) across the six experts was 0.97. The scale-level content validity index (S-CVI), or average of all item level validity index scores, was 0.97. Thus, the scale exceeded the minimum acceptable CVI value index across six raters (0.83) as defined by Wieck (1996). After the focus group data analysis and psychometric evaluation of the survey instrument, we conducted pilot testing all employees.
Pilot Study. Participants in the focus groups had noted that swamping was not just limited to nurses. They indicated that swamping occurred for all members of the healthcare team. To determine if that was indeed the case, we conducted a pilot study at one hospital. This hospital had 427 beds and included medical surgical units, intensive care, emergency services, a high-risk labor and delivery unit and neonatal intensive care. All members of the healthcare team, including physicians with inpatient privileges, were invited to take the survey emailed to them with a link. There were 451 participants.
Participants in the focus groups had noted that swamping was not just limited to nurses.
The pilot study responses from the other members of the healthcare team were remarkably similar to those of the nurse focus group participants. This similarity in response led to the more inclusive study reported below that involved other providers and tested results in multiple hospitals. To this end, following the pilot study, we modified the survey to reflect this in the demographic information collected. Our goal was to widen the scope of our work to include a more diverse population of hospital employees who may perceive swamping.
Methods
Population, Setting, and Sample
The population studied was employees and providers in select community-based hospitals in the fall of 2018. The settings included one 120-bed hospital providing medical, surgical and emergency care; one 204-bed hospital offering inpatient and outpatient surgical services, intensive care and emergency services; and two Level I Trauma community hospitals, one with 262 beds and one with 325 beds. All of the hospitals were Magnet designated. A convenience sample of 814 participants completed the survey (11.6% return rate).
Data Collection and Analysis
Approval for this non-experimental descriptive research study was obtained from the hospital system Institutional Review Board. An email survey was distributed to all employees and select external providers (approximately 7000 employees with slight daily variation) in four large community-based hospitals. Department directors were encouraged to forward the email to staff email addresses used for routine communication. The medical staff office sent an invitation email with a link to the survey to all external providers with inpatient privileges.
An informed consent statement opened the study and respondents indicated willingness to participate by continuing with the survey. All answers were anonymous and identified only by a number generated by the study instrument. Participants were invited to enter their email address (not linked to survey responses) for a drawing for one of four iPads (one per hospital) after the survey was completed. No ethical issues arose during the study.
A two-week period was allowed for responses, and reminder emails were sent on days 7 and 13. The survey was comprised of demographic items and 13 survey questions, most of which allowed participants to add comments (Table 1). The scoring for the survey items varied, for instance, question 1 scores ranged from 1 (never, the lowest available option) to 5 (multiple times per day, the highest available option). Scores of 4 indicated feeling swamped on a daily basis, while scores of 3 suggested this feeling on a weekly basis, and a score of 2 indicated feeling swamped monthly.
Table 1. Being Swamped in the Clinical Setting Survey Question Overview
|
Question |
Answer Options |
|---|---|
|
1. How often are you swamped? |
a) 1-2 times/month |
|
2. Is there a certain time of the day that you feel swamped the most often? |
Various times of the day generalized and in two-hour blocks of time. |
|
3. When you are swamped, what percent of the time can you identify before it occurred that you were getting swamped? |
Free text, entered percent. |
|
4. Which of these (signs/symptoms) occur when you are feeling swamped? Multiple answers allowed. |
a) Sweating |
|
5. Rate on a scale of 1-10 (not swamped to severely swamped) how swamped you typically feel when these situations occur? |
a) Fatigue |
|
6. When you are swamped, what percent of the time do you feel others recognize that you are swamped without you saying you are? |
Free text, entered percent. |
|
7. When you are swamped, what percent of the time do you receive help? |
Free text, entered percent. |
|
8. Who helps you when you get swamped? |
a) Another member of the team (RN:MD, Dietary:RN, Housekeeper:Nurse Tech) |
|
9. Rate on a scale of 1-10 what helps you when you are swamped. |
Sliding scale from 1-10 (not swamped to severely swamped) with free text option. |
|
10. What behaviors tell you that others are swamped? Multiple choices allowed |
a) They are not around the desk |
|
11. What is the impact of being swamped on your team? Multiple choices allowed. |
Seven options and free text: |
|
12. What is the impact of being swamped on your patients or families? Multiple choices allowed. |
Nine options and free text allowed |
|
13. Is there anything you would like to add? |
Free text, optional |
Note: Being swamped is defined as when you are so overwhelmed by the circumstances that you are unable to focus on the most important thing (a human factor).
Survey findings were evaluated using both quantitative and qualitative strategies for analysis. Data from the survey were analyzed using SPSS version 25 (IBM Corp, Armonk NY). Means, standard deviations, and frequency counts (percentages) were calculated as appropriate. If response data were skewed, medians and inter-quartile ranges were considered. Thematic content analysis was used to describe emerging themes from open ended responses (Polit et al., 2017).
Results
Only 3.8% of participants noted that they are never swamped, while 11.8% noted they feel swamped on a daily basis.
Results were evaluated by the study team, comprised of two doctorally prepared advanced practice registered nurses (APRNs) and two statisticians. Participants (n = 814) included: administrators (n = 29), case managers/social workers (n = 15), support staff (e.g., internet technology, laboratory, pharmacy, radiology; n = 364), RNs (n = 340), licensed vocational nurses (n = 2), supervisors (n = 70), physicians (n = 38), physician assistants (n = 2), and advanced practice nurses (n = 8). Only 3.8% of participants noted that they are never swamped, while 11.8% noted they feel swamped on a daily basis.
Unit Specific Data
In nursing units, areas with rapid turnover and unexpected volume changes or patient status changes tended to have the higher levels of being swamped. These included ICU (Mean = 2.3, SD = 1.1), ED (Mean = 2.5, SD = 1.1), and Labor & Delivery (Mean = 2.3, SD = 1.1); each of these scores suggests daily swamping Medical Surgical units ranged from mean scores of 1.8(SD = 0.8) to 2.7(SD = 2.1), suggesting weekly to daily perceptions of swamping. Areas of more predictable volume (i.e., where patients are seen on a scheduled basis (e.g., Pre-op, Post-Anesthesia Care Units, Operating Rooms, Outpatient Surgery, and Radiology) tended to have lower scores that averaged 1.8(SD = 1.1), an indicator of weekly swamping. Dialysis and Endoscopy areas, although often scheduled, reported scores that suggested daily swamping, with means of 2.1(SD = 1.1) and 2.4(SD = 1.2), respectively. Nursing educators averaged a daily swamping mean score of 2.3(SD = 1.0).
areas with rapid turnover and unexpected volume changes or patient status changes tended to have the higher levels of being swamped.
Role Specific Data
Data were evaluated from the category of job role, using the same scale. Participants self-identified their roles and area separately, so results varied between the two questions. For instance, a person working in the Pharmacy would report Pharmacy as their department, while under job role, a Pharmacy tech might be in a different category than a Pharmacist. Pharmacy and laboratory personnel had the highest scores (i.e., daily swamping) with means of 2.6(SD = 1.1) and 2.8(SD = 1.0), respectively. Also reporting being swamped on a daily basis were Administration (M = 2.2, SD = 1.1), Case Management/Social Worker (M = 2.5, SD = 1.2), Medical Technologist (M = 2.7; SD = 1.2), Nurse Tech (M = 2.2, SD = 1.0), Respiratory Therapy (M = 2.5, SD = 1.2), RN (M = 2.2, SD = 1.0), APRNs (M = 2.5, SD = 1.4), Physicians (M = 2.4, SD = 1.4), Information Technology (M = 2.5, SD = 1.4), and Supervisor (M = 2.2, SD = 1.0). Those who reported being swamped weekly were Dietary (the lowest at mean of 1.3, SD of 0.5) and PT/OT/Speech Therapy (M = 1.7, SD =0.6).
Survey Item Responses
Each question on the survey was evaluated individually. Responses to survey items are summarized below by frequency percentages or mean/standard deviations, as appropriate.
How often are you swamped?
Answers were assigned a score of 0 = Never, 1 = Weekly, 2 = Daily, 3 = Multiple times per day. The most common response to this question was, “1-2 times per week,“ (35.8%, n = 289); followed by “1-2 times per month,” at 29.2% (n = 236). Being swamped “multiple times per day” was indicated by 11.6% of participants (n = 96). Most responses to this question concerned heavy assignments or dealing with a sudden unexpected turn of events with a patient. Comments included:
- Always, I’m always swamped to the point that it is my new norm.
- A way of life, it’s just accepted 100%.
- Usually things start to pile up and you think you can manage…then a few more tasks or events happen, and you get so far behind your mind can’t manage all the tasks and prioritize anymore.
Is There a Certain Time of the Day that You Feel Swamped Most Often?
Allowable options included both general times and two-hour increments of times; participants could select more than one choice. Although 38.0% (n = 309) of participants noted that being swamped can occur anytime, it most commonly occurred at the beginning of the shift (26.9%, n = 219) and the end of the shift (17.3%, n = 141). Only 2.8% (n = 23) of participants noted feeling most swamped between 11 PM and 5 AM.
When You Are Swamped, What Percent of the Time Could You Identify Before It Occurred that You Were Getting Swamped?
The option, “Can never tell when I am getting swamped” was selected by 29% (n = 236) of respondents. Slightly over 22% (n = 180) felt they could tell they are getting swamped 40-60% of the time, and only 16.9% (n = 138) could tell they are becoming swamped 80-100% of the time.
Which of the Following (Signs or Symptoms) Occur When You Are Swamped?
This question listed seven common signs/symptoms that people might feel when they were getting swamped. The most common signs were “feel anxious” at 62.5% (n = 509), “trouble prioritizing tasks” at 35.6% (n = 290), and “feel angry” at 32.9% (n = 267). Also endorsed were “sweating”, “feeling jittery”, “heart races”, and “face flushes/feel hot.” Comments for this question included:
- Difficulty articulating what another staff member can assist with
- Shut down of emotion and task orient mode until the situations are resolved
- Frustrated
- Feel incompetent that I can’t keep up
Rate on a Scale of 1 to 10 How Swamped You Typically Feel When These Situations Occur
Eleven situations were provided, using a Likert response scale from 1 (least) to 10 (most). The highest rated were “assignment too heavy/unbalanced” with a mean response of 7.1(SD = 2.6) and “interruptions” at 6.1(SD = 2.8). “Patient deteriorating/critical”, “communication issues”, “lack of supplies”, and “unexpected occurrences” were rated with means from 5.3(SD = 3.0) to 5.4(SD =2.9). “Working ill,” “new processes/procedures”, and “fatigue” were rated 4.9(SD = 2.8), 4.5(SD = 2.7), and 4.4(SD = 2.6) respectively. The lowest rated was “stress at home” (Mean = 3.8, SD = 2.7).
When You Are Swamped, What Percent of the Time Do You Feel Others Recognize that You Are Swamped Without You Saying You Are?
Among 814 participants providing estimates, the median (i.e., interquartile range/IQR) estimate was 30% (n=731); 7.5% (n = 61) reported “0%,” and 2.6% (n = 22) reported “100%.”
When You Are Swamped, What Percent of the Time Do You Receive Help?
Of 814 participants who responded, the median (IQR) estimate was 30% of the time (n = 743); 6.0% (n = 49) reported “0%,” and 2.6% (n = 22) reported “100%.”
Others who helped included supervisors, managers, specialty resources and other hospital resources.
Who Helps You When You Get Swamped?
The most common response was, team members in the same job role (e.g., RN: RN) at 53.3% (n = 434) and other team members who were not the same job role (e.g., MD: RN), at 47.4% (n = 386). Others who helped included supervisors, managers, specialty resources and other hospital resources.
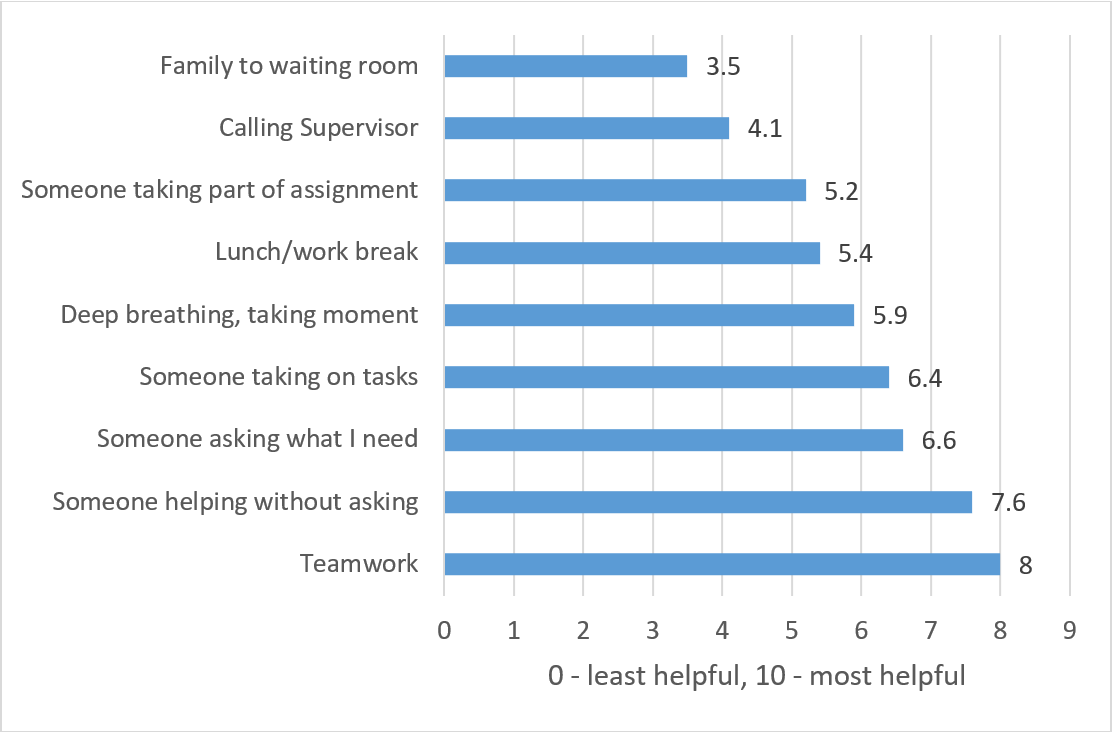
Rate on a Scale of 1-10 What Helps You When You Are Swamped
Nine options were listed for this item with an open-ended text box. (See Figure). The highest score (scale of 1-10) for what helps was “teamwork” with a mean of 8.0(SD = 2.2) closely followed by “Someone helping without asking what I need” at mean of 7.6(SD = 2.6). The mean for the response “Calling the supervisor” was 4.1(SD = 2.9), and “sending the family to the waiting room” was the lowest mean at 3.5(SD = 3.2). There were many comments that included “appropriate staffing.” Other common comments included “prayer”, “acknowledgement”, “feeling supported by administration” and “stop unnecessary interruptions.”
Figure. What Helps When You are Swamped?
What Behaviors Tell You that Others Are Swamped?
Eleven choices were provided, with multiple choices allowed and a text box option. The three most frequent responses were, “they look frustrated” (87.5%, n = 712), “they are running around as fast as possible” (74.9%, n = 610), and “they have not taken a break” (70%, n = 570). Also endorsed (in descending order of response) were “they say so”, “they look angry”, “they are short-tempered”, “they are crying”, “they are not chatting with others”, “they are very quiet or focused”, “they are not around the desk” and “they are not charting.” One person commented “we become frustrated with each other and say things that we normally would not.”
What is the Impact on Your Team, Patients, and Families?
The highest level of impact on patients and families was that patient care is perceived as poorResponses are listed in Table 2. Of note is that 60-68% of nurses surveyed felt that the effects of being swamped included: errors happen, things don’t get done or are missed, and things get done, but not on time. These factors could lead to job dissatisfaction and ultimately to staff leaving their jobs, also indicated by 63.4% (n = 516) of respondents. The highest level of impact on patients and families was that patient care is perceived as poor, selected by 76.5% (n = 623) and long delays to answer call lights at 55.2% (n = 449).
Table 2. Perceived Impact of Being swamped on Healthcare Team, Patient and Families
|
Nurses estimate of effect of being swamped on: |
Impact |
N |
% |
|---|---|---|---|
|
Healthcare Team (more than one answer allowed) |
|||
|
|
Errors occur |
553 |
67.9 |
|
|
Things don't get done/missed |
536 |
65.8 |
|
|
Staff get frustrated and quit |
516 |
63.4 |
|
|
Things get done, but not on time |
490 |
60.2 |
|
|
Multiple phone calls |
320 |
39.3 |
|
|
Supervisors get frustrated and quit |
142 |
17.4 |
|
Patient & Families (more than one answer allowed) |
|||
|
|
Patient care is perceived as poor |
623 |
76.5 |
|
|
Long delays to answer call lights |
449 |
55.2 |
|
|
Discharge information gets missed |
376 |
31.4 |
|
|
Delayed discharge times |
351 |
43.1 |
|
|
Poor pain control |
309 |
38.0 |
|
|
Missed medications |
298 |
36.6 |
|
|
Falls |
267 |
32.8 |
|
|
Wrong orders get entered |
231 |
28.4 |
|
|
Poor care coordination |
217 |
26.7 |
Is There Anything You Would Like to Add?
Using the open-ended question format, participants were able to respond with their own words and from their own perceptions. This question generated 137 comments. Themes that emerged from these comments generally concerned timing of being swamped, budget issues related to being swamped, chronically being swamped, and coping mechanisms utilized. Selected representative comments included:
- The worst swamping occurs when multiple staff get swamped at the same time then no one can help each other….
- Being swamped occurs when budget becomes more important than safe staffing
- Swamping hours usually center around shift change. Administrators and leaders need to be more involved with staff support and patient care at these times
- This is something we deal with in healthcare on a daily basis and isn't easily avoidable. As long as the mindset of knowing you are going to be swamped at any given time is a good coping mechanism for me, mentally and physically.
- I think this Hospital as a whole is really great at not getting swamped. Everyone here works well with each other. Every now and then I will go to a floor that gets swamped but we all as a team work together.
- When the RN/patient ratio is not right for acuity nobody wins…except maybe the budget. Does anyone put a price on nurse burnout, high turnover, and poor patient outcomes?
- Feeling swamped is demoralizing; you want to be the best you can be and take care of everyone's needs and meet unit time goals, etc., but when the workload is too high you must prioritize, usually leaving people in pain and delaying treatment and discharges and call-light responsiveness. Now patients and family are angry at you, even though you're doing the very best you can to manage everyone's needs while ignoring your own, not eating lunch until after 4pm and hardly having time to even pee. We are by nature caregivers, and we give of ourselves until we break.
Discussion
Being swamped in the clinical setting is a real phenomenon. The strength of this study was in hearing the voices of all members of the healthcare team in an anonymous setting where they were free to give their opinions. Data categorized by area worked revealed interesting patterns. Participants from all areas in the hospital reported being swamped at a weekly or daily level, as did respondents in all job roles. Findings presented from this study, and those of our pilot study as well, confirmed the nurses’ opinions in the AWHONN study (Roth et al., 2020). Both studies found that swamping occurs in almost every area of the hospital, irrespective of unit or specific role, across multiple hospitals.
As budgets and staffing grow tighter, being swamped increases (Roth et al., 2015). This study found that increases in being swamped lead to missed care, errors, turnover, and delays in care (Simpson et al., 2016.). Patients and families are also affected when the staff is swamped, perceiving their care as poor, experiencing delays in answers to call lights and discharge, and incomplete discharge teaching which may lead to readmissions (Simpson et al., 2016.).
Participants reported that teamwork and another team member helping them without asking what they need is the most beneficial response to being swamped. Someone to take on tasks and ask what is needed or give a moment to take a breath is also helpful. The findings in this study supported existing studies in the nursing literature that have indicated that being swamped can have implications for patient satisfaction scores that impact reimbursement and nationally reported data. (AACN, 2019; Recio-Saucedo et al., 2018) In addition, perceptions of being swamped, especially on a daily basis, can possibly result in high turnover as staff feel discouraged and leave. (Simpson et al., 2016)
Someone to take on tasks and ask what is needed or give a moment to take a breath is also helpful.
This study had several limitations. The study was completed in Magnet designated hospitals using a convenience sample and may not be generalized to all hospital settings. Bias may have been a factor for those who made comments.
Conclusion: Implications for Practice
Failure to address frequent feelings of being swamped in a timely manner may lead to problems with staff retention. Identifying ways to quickly recognize the feelings of being swamped and determining the most effective steps for intervention is the next area of exploration. In times of critical staffing needs, healthcare leaders must acknowledge and find ways to mitigate being swamped in the clinical setting. The findings from this study have suggested actions identified by the healthcare team members themselves, including additional support persons with experience who are able to step in to help in critical situations, or give breaks at critical times. Thus, one potential solution might be the use of experienced senior staff who are nearing retirement or have already retired as helpers during times when the chance of being swamped is high. Other creative ways to assign staff may enable them to maintain the ability to think critically in these high stress situations.
In times of critical staffing needs, healthcare leaders must acknowledge and find ways to mitigate being swamped in the clinical setting.
Acknowledgement: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors
Cheryl Roth, PhD, WHNP-BC, RNC-OB, RNFA
Email: croth@honorhealth.com
ORCID ID: 0000-0001-8394-8793
Dr. Cheryl Roth is a Nurse Practitioner in a High-Risk Obstetrics Setting. Her PhD work on “Human Factors Contributing to Nursing Errors” led her to the identification of “being swamped” as a significant factor and has been part of her program of research. She is a member of the hospital IRB.
Melanie A. Brewer, DNSc, RN, FNP-BC, NEA-BC, FAANP
Email: mbrewer@honorhealth.com
ORCID ID: 0000-0003-3117-5340
Dr. Melanie Brewer is the Director, Research and Academic Partnerships, Center for Clinical Excellence, for HonorHealth and has a rich background of research and evidence-based practice. She is Chair of the Nursing Research Council and sits on the hospital IRB.
Kevin P. Gosselin, PhD
Email: Aritexllc@gmail.com
ORCID ID: 0000-0002-6212-4784
Dr. Kevin Gosselin is a statistician with a strong background in graduate level nursing education and research. At the time of the study, he worked in the HonorHealth Research Institute and was a member of the hospital IRB.
Curtis Bay, PhD
Email: cbay@atsu.edu
ORCID ID: 0000-0003-3525-9269
Dr. R. Curtis Bay is a professor at A.T. Still University, in the Biostatistics, Department of Interdisciplinary Health Sciences. He chairs the IRB at A.T. Still University and is a member of the HonorHealth IRB.
References
AACN. (2019). Fact Sheet: nursing shortage. American Association of Colleges of Nursing. https://www.aacnnursing.org/Portals/42/News/Factsheets/Nursing-Shortage-Factsheet.pdf
Aiken, L. H. et al. for the RN4CAST Consortium (2017). Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Quality and Safety. 26(7), 559-568. https://www.doi.org/10.1136/bmjqs-2016-005567
Ball, J. E., et al. for the RN4Cast Consortium. (2018). Post-operative mortality missed care and nurse staffing in nine countries: A cross-sectional study. International Journal of Nursing Studies, 78, 10-15. https://www.doi.org/10.1016/j.ijnurstu.2017.08.004
Dyrbye, L.N. et al. (2019). A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nursing, 18:57, 1-8. https://www.doi.org/10.1186/s12912-019-0382-7
Griffiths P. et al. (2016). Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: a cross-sectional study. BMJ Open, 6(2), e008751. https://www.doi.org/10.1136/bmjopen-2015-008751
Haidari, E. et al. (2021). Maternal and neonatal health care worker well-being and patient safety climate amid the COVID-19 pandemic. Journal of Perinatology, 41(5), 961-969. https://www.doi.org/10.1038/s41372-021-01014-9
Jameton, A. (1984). Nursing practice: The ethical issues. Englewood Cliffs, NJ: Prentice-Hall.
Lake, E. T. et al. (2017). Missed nursing care in pediatrics. Hospital Pediatrics, 7(7), 378-384. https://www.doi.org/10.1542/hpeds.2016-0141
McHugh, M. D., Berez, J., & Small, D.S. (2013). Hospitals with higher nurse staffing had lower odds of readmissions penalties than hospitals with lower staffing. Health Affairs (Millwood), 32(10), 1740-1747. https://www.doi.org/10.1377/hlthaff.2013.0613
McManus, J., Huebner, K., & Scheulen, J. (2006), The science of surge: Detection and situational awareness. Academic Emergency Medicine, 13(1), 1179-1182. https://www.doi.org/10.1197/j.aem.2006.06.038
Needleman, J. et al. (2020). Association of registered nurse and nursing support staffing with inpatient hospital mortality. BMJ Quality and Safety, 29(1),10-18. https://www.doi.org/10.1136/bmjqs-2018-009219
Ogrinc, G. et al. (2015). Standards for Quality Improvement Reporting Excellence (Squire 2.0). BMJ Quality and Safety 0:1–7. https://www.doi.org/10.1136/bmjqs-2015-004411
Polit D.F. & Beck C.T. (2017). Nursing Research: Generating and Assessing Evidence for Nursing Practice (Tenth Ed.). Philadelphia: Wolters Kluwer.
Recio-Saucedo, A. et al. (2018). What impact does nursing care left undone have on patient outcomes? Review of the literature. Journal of Clinical Nursing, 27(11-12), 2248-2259. https://www.doi.org/10.1111/jocn.14058
Roth, C., Brewer, M.A., Bay, R.D., & Gosselin, K.P. (2020). Nurses’ experiences of “being swamped” in the clinical setting and association with adherence to AWHONN Nurse Staffing Guidelines. MCN, The American Journal of Maternal/Child Nursing, 45(4) 271-279. https://www.doi.org/10.1097/NMC.0000000000000643
Roth, C.K., Brewer, M., & Wieck, K.L. (2016). Using a Delphi method to identify human factors contributing to nursing errors. Nursing Forum. https://www.doi.org/10.1111/nuf.12178
Roth, C., Wieck, K.L., Fountain, R., Haas, B.K. (2015). Hospital nurses' perceptions of human factors contributing to nursing errors. Journal of Nursing Administration,45(5), 263-9. https://www.doi.org/10.1097/NNA.0000000000000196
Shanafelt, T.D. et al. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18):1377–85. https://www.doi.org/10.1001/archinternmed.2012.3199
Shin, S., Park, J.H., & Bae, S.H. (2018). Nurse staffing and nurse outcomes: A systematic review and meta-analysis. Nursing Outlook, 66(3):273–82. https://www.doi.org/10.1016/j.outlook.2017.12.002
Simons, D. J., & Chabris, C. F. (1999). Gorillas in our midst: Sustained inattentional blindness for dynamic events. Perception, 28(9), 1059–1074. https://www.doi.org/10.1068/p281059
Simpson, K.R., Lyndon, A., & Ruhl, C. (2016). Consequences of inadequate staffing include missed care, potential failure to rescue, and job stress and dissatisfaction. Journal of Obstetric Gynecologic & Neonatal Nursing, 45(4):481-90. https://www.doi.org/10.1016/j.jogn.2016.02.011
Simpson, K. R. et al. (2019). Adherence to the AWHONN Staffing Guidelines as perceived by labor nurses. Nursing for Women's Health, 23(3), 217-223. https://www.doi.org/10.1016/j.nwh.2019.03.003
The Merriam-Webster.com Dictionary. (2019). Swamp. Merriam-Webster Inc. https://www.merriam-webster.com/dictionary/swamping?src=search-dict-box
Tubbs-Cooley, H. L. et al. (2019). Association of nurse workload with missed nursing care in the neonatal intensive care unit. Journal of the American Medical Association Pediatrics, 173(1), 44–51. https://www.doi.org/10.1001/jamapediatrics.2018.3619
West, C.P. et al. (2009). Association of resident fatigue and distress with perceived medical errors. Journal of the American Medical Association; 302(12), 1294-1300. https://www.doi.org/10.1001/jama.2009.1389
Wieck K. L. (1996). Diagnostic language consistency among multicultural English-speaking nurses. Nursing diagnosis : ND : the official journal of the North American Nursing Diagnosis Association, 7(2), 70–78. https://doi.org/10.1111/j.1744-618x.1996.tb00295.x


