Incidental findings are commonly found during routine, diagnostic imaging. Prevalence varies widely; but research shows that follow-up of incidental findings is poor. Further, incidental findings that are likely to change clinical outcomes are not necessarily more likely to receive follow-up care. It has also been shown that both lack of management and over-management can lead to poor patient outcomes. Innovative solutions are needed to ensure timely follow-up care and appropriate management of incidental findings. One possible solution to address low clinical follow-up care of incidental findings is to employ advanced practice registered nurses (APRN) as incidental findings coordinators. The coordinator would have the potential to improve communication and defragment care. The aims of this article are to discuss the problem of low follow-up care of clinically relevant incidental findings and to present a recommendation for a new role for APRNs to address the problem. In this article the authors will review the literature, describe the search for answers, present a new role for the APRN as an incidental findings coordinator, and conclude that the APRN incidental findings coordinator role has the potential to solve many problems encountered in current practice.
Key Words: Incidental findings, incidentaloma, advanced practice registered nurse (APRN), coordinator
Incidental findings on imaging, also called incidentalomas, are common.Incidental findings on imaging, also called incidentalomas, are common. Incidental findings may be identified during routine workup, diagnostic imaging, and frequently, in emergency situations in which imaging is done after a traumatic event. A recent study examining the rate of incidental findings on a computed axial tomography scan (CAT or CT scan) after any blunt trauma reported an average of three findings per patient (James, Francois, Yoeli, Doughlin, & Lee, 2017); however, prevalence varies widely (Gibson et al., 2018). Overall, follow-up of incidental findings is poor (Adams, Rakheja, Bryce, & Babyn, 2018; Kwan et al., 2019). Innovative solutions are needed to ensure timely follow-up of incidentalomas. The aim of this article is to discuss the problem of low follow-up of clinically relevant incidentalomas and to present a recommendation for a new role for advanced practice registered nurses (APRNs) to address this problem.
Innovative solutions are needed to ensure timely follow-up of incidentalomas.Presently, there is no general consensus guiding classification of incidental findings found on imaging. Therefore, this article refers to incidental findings as clinically relevant when a study showed that the radiologist or clinician recommended follow-up; treatment specific to the incidentaloma was deemed necessary; or when an investigator determined the findings were clinically significant based on classifications designed specifically for a research project.
Presently, there is no general consensus guiding classification of incidental findings found on imaging.Current practice for follow up on incidental findings varies between institutions. Our institution, the Cleveland Clinic, like many, uses technology to assist in detection and follow-up of incidental findings. Even with numerous processes to ensure adequate follow-up for incidental findings, we have recognized that continued work is needed at our institution to fully address this challenge. To that end, our Enterprise Quality Team has created partnerships both across clinical disciplines and with our information technology teams that are yielding solutions. Our solutions integrate and align clinical workflows and focus on optimizing people, process, and technology to improve patient care. It is our sense that the best practices that emerge from this ongoing work will identify ways to harmonize alerts and decision support within our electronic health system with the actions of our caregiver teams, including mid-level and advanced practitioners.
Review of the Literature
In this section we will discuss current literature related to incidental findings. Additionally, we consider the ongoing dilemma of unaddressed incidental findings and the cost of incidental findings.
Unaddressed Incidental Findings: An Ongoing Dilemma
The reported prevalence of incidental findings in the literature ranges from 20% (Collins et al., 2015; Tuncel et al., 2015) to as high as 98% (Cieszanowski, et al., 2014). The prevalence of incidental findings that are clinically relevant varies widely as well. Clinically relevant incidental findings found on CT in trauma patients have rates ranging from 20% (Yeh et al., 2013) to 52% (Ravindran, Hancox, Barlow, Dunk, & Howlett, 2016). Potentially life-threatening incidental findings have been reported to affect as many as 1 out of 15 trauma patients (Fakler, Ozkurtul, & Josten, 2014).
The proportion of incidental findings that received little or no follow-up has been reported as high as 65%.Patients who had the most severe findings were actually less likely to be informed or receive follow-up for these findings (Al Mutairi, Meyer, Chang, & Singh, 2015). The proportion of incidental findings that received little or no follow-up has been reported as high as 65% (Adams, Rakheja, Bryce, & Babyn, 2018). A 2017 study showed that only 7% of patients with clinically relevant incidental findings in the pre-intervention arm received instructions and had been informed of the findings (Sich et al., 2018). Patients who have findings that are most likely to change their clinical outcome are not necessarily more likely to be informed or receive follow-up. A retrospective chart review showed that patients who were more likely to require follow-up were notified about their finding less than half the time (Collins et al., 2015). In fact, flagging imaging results as “critical” was not enough to ensure timely follow-up, even when the healthcare provider had read the results (Singh et al., 2009).
...flagging imaging results as “critical” was not enough to ensure timely follow-up...In 2010, in an effort to address the ongoing challenge of managing incidental findings, the American College of Radiology set goals that included reducing risks (e.g., radiation), limiting costs, and improving consistency in management, including consistent definitions of terms such as unanticipated or incidental (Berland et al., 2010). Providers, however, may not always follow radiologists’ recommendations (Rosenkrantz, Xue, Gyftopoulos, Kim, & Nicola, 2018a). Providers may over-test or over-treat patients who have an incidental finding, for fear of litigation or to allay patient fears (Berland et al., 2010). On the other hand, many clinically relevant incidental findings do not receive any follow-up at all.
Paying the Price for Incidental Findings
The cost of incidental findings to patients, hospitals, and providers comes in many forms. The presence and management of incidental findings alone affects patient outcomes by increasing length of hospital stay (Andrawes et al., 2017) and delaying other necessary treatments (Showkathali et al., 2015). Lack of management of incidental findings has the potential to affect outcomes when ignored or over-managed, resulting in failure to rescue scenarios or delayed management of the primary disease. Lack of follow-up can also result in patient harm (Hickner et al., 2008). While outcomes and management are infrequently reported in the literature (Gibson et al., 2018), it was found that 14% of cases flagged as suspicious for malignancy did not receive follow-up (Murphy, Thomas, Meyer, & Singh, 2015). Unfortunately, some types of incidentalomas are malignant as often as 42% of the time (O’Sullivan, Muntinga, Grigg, & Ioannidis, 2018).
Providers frequently depend on a patient follow-up visit as a reminder for further imaging and treatment.Adding to the problem of low provider follow-up rates is the fact that patients may not follow-up with appointments, tests, or treatment. Providers frequently depend on a patient follow-up visit as a reminder for further imaging and treatment (Al Mutairi et al., 2015). When they do not keep the appointment or transfer care, there is a risk of loss of follow-up. Follow-up time has been shown to be delayed (Raich, Whitley, Thorland, Valverde, & Fairclough, 2012) and outcomes poorer (Wheeler & Bryant, 2017) in underserved populations, making management solutions even more urgent. Moreover, patients may not have the opportunity to participate in their own care if they are not notified of the incidental finding.
Over-management of incidental findings brings risk as well.Over-management of incidental findings brings risk as well. A cascade of testing sometimes results, increasing patient risk (Lumbreras, Donat, Hernandez-Aquado, 2010), including unnecessary exposure to radiation. The literature also suggests that poor outcomes may result from delaying treatment of the primary disease process in order to investigate incidentalomas (Adams, Rakheja, Bryce, & Babyn, 2018).
Healthcare costs can be affected by incidental findings. Agarwal, Talia, Liu, Momoh, and Kozlow (2016) found an additional mean cost increase of 32% for patients due to incidental findings. Providers who order follow-up tests impact costs when they do not follow radiologists’ recommendations or over-manage the incidental finding (Rosenkrantz et al., 2018b), due in part to unnecessary follow-up scans (Rosenkrantz et al, 2018a). Lack of follow-up and patient notification carries significant costs as well, not the least of which is litigation (Paluska et al., 2007). Follow-up that does take place, but is not documented, represents additional legal risk (Paluska et al., 2007).
A Search for Answers
In many cases it is not clear which provider is responsible for follow-up of incidental findings.In many cases it is not clear which provider is responsible for follow-up of incidental findings. For example, if a CT is done in the emergency department (ED), the abnormal results may be received by the ED physician. The ED physician is responsible for the imminent health threat; therefore, results may need to be sent to the primary care provider or addressed by another specialist (James et al., 2017). Unfortunately, when more than one provider receives results there can be diffusion of responsibility and a lower likelihood of follow-up (Singh et al., 2009).
Several approaches have been investigated to address the management of incidental findings, including deliberate and dedicated communication to the primary care provider (Yeh et al., 2013) or the patient (Collins et al., 2015). Use of electronic medical record notification systems (O’Connor, Dalal, Sahni, Lacson, & Khorasani, 2016) have shown promise; however, alert fatigue is a problem for many providers (Singh, Spitzmueller, Petersen, Sawhney, & Sittig, 2013).
...innovations in research are leading to the use of artificial intelligence to increase diagnostic accuracy within radiology.The end result of increased diagnostic accuracy may be an increase in both in number and clarity of incidental findings. Likewise, the aging population will increase the number of incidental findings since more incidentalomas are found in older adults compared to their younger counterparts (Cieszanowski, et al., 2014). A provider will be necessary to lead a team of incidental findings coordinators to address this growing management problem.
A New Role for the APRN: The Incidental Findings Coordinator
The literature shows that both mid-level practitioners (Huynh et al, 2008) and resident physicians (Sperry et al., 2010) have been used to manage incidental findings. While studies have demonstrated the usefulness of an incidental findings coordinator role, there is little or no evidence to suggest that such a role has been widely implemented. An approach that addresses the low clinical follow-up of incidental findings, with clearly defined roles of responsibility to improve coordination and communication (Adams, Babyn, & Danilkewich, 2016), is needed.
...both mid-level practitioners and resident physicians have been used to manage incidental findings.Establishing APRNs as incidental findings coordinators would put qualified providers in a role responsible for filling the gaps and human errors in communication. Additionally, placing a provider in this role will be essential prior to adopting software algorithms that increase diagnostic accuracy, but do not have the human experience of filling gaps in communication, at several steps within healthcare. For example, the possibility exists that artificial intelligence will augment diagnostic accuracy to the point that a greater number of incidental findings will be detected, thus increasing the need for better coordination and communication.
A coordinator role for APRNs would be an innovative use of personnel and resources to address the problem of inconsistent management of incidental findings...A coordinator role for APRNs would be an innovative use of personnel and resources to address the problem of inconsistent management of incidental findings, potentially reducing preventable patient harm. Researchers have recommended liaisons to ensure follow-up of incidental findings (Andrawes et al., 2017) because the current state of inconsistently addressing these findings is not sustainable. The individual in a coordinator role would need to have clinical expertise, the authority to place orders, patient counselling skills, and the ability to work inter-professionally. The introduction of this new role for APRNs as incidental findings coordinators can maximize the clinical skill set of the APRN while taking advantage of the holistic approach used by nurses for patient care.
In many states, APRNs have full practice authority; however, the APRN incidental findings coordinator would work in collaboration with at least one physician. In fact, the coordinator’s primary role would be to improve value and outcomes by working collaboratively with the ordering provider, specialists, and radiologists. As APRNs strive to practice at the top of their licensure, new and innovative roles, such as an APRN incidental findings coordinator role, have the potential to increase patient safety and resources, and to improve patient outcomes. The end result of the full extent of practice for APRNs is improved care coordination (Yang & Meiners, 2014).
Care Coordination
Incidental finding management requires ongoing coordination of care.Incidental finding management requires ongoing coordination of care. Lay patient navigators have been used successfully to improve time to follow-up testing (Raich et al., 2012); however, care coordination goes beyond simply ensuring patients keep their appointments. Care coordinators provide continuity of care, coordinate the efforts of healthcare team members (Holliday, Samanta, Budinger, Hardway, & Bethea, 2017), manage care (Nelson, Bobade, Hunt, & Mundi, 2018), identify needs, provide patient education, and ensure follow-up (Dunn & Rogers, 2016). A model of care that includes an APRN as incidental findings coordinator would be a new way to utilize care coordination (see Table).
Table. The APRN Incidental Findings Coordinator Role.
|
|
Concerns with current practice |
Advantages of an APRN incidental findings coordinator |
|
Coordination |
|
|
|
Communication |
|
|
|
Long term follow-up |
|
|
APRNs are poised to identify gaps in care (Hurlock-Chorostecki & McCallum, 2016), and as a result they can successfully coordinate patient care. There are numerous reports of effective models using APRNs and other mid-level practitioners to coordinate patient care, resulting in fewer admissions (Holliday et al., 2017), improved glycemic control (Nelson et al., 2018), and timely discharges (Dunn & Rogers, 2016; Holliday et al., 2017). Thus, care coordination, working directly with patients, and collaborating with physicians, is already part of the APRN role.
...coordinating care for patients with incidental findings would include working directly with the patient and appropriate inter-professional providers.Coordination includes caring for and communicating with patients to “defragment care, reduce patient burden and smooth transitions,” vital roles of the APRN (Hurlock-Chorostecki & McCallum, 2016, p. 85) and an important aspect of the incidental findings coordinator role. Similar to other types of care coordination, coordinating care for patients with incidental findings would include working directly with the patient and appropriate inter-professional providers, from the point of notification about the finding, to establishing a plan for testing, appropriate treatment, and/or referral when indicated.
Additionally, coordination of care would include leading a team of nurses as needed, to meet the unique needs of each institution. Larger hospitals may need incidental findings coordinators and other team members for each institute or department, thus taking advantage of areas of specialty for each APRN and addressing the large volume of imaging at these institutions. Likewise, small institutions may have one or two APRNs who coordinate all incidental findings for the hospital. In either case, the coordinator or team, would likely be employed by the radiology department; however, models using outside contractors could also be considered.
...an APRN-led team to address incidental findings has the potential to reduce inefficiencies and improve patient outcomes.Ultimately, an APRN-led team to address incidental findings has the potential to reduce inefficiencies and improve patient outcomes. As noted earlier, incidental findings are costly (Agarwal et al., 2016). The incidental findings coordinator role brings value to a process of follow-up that has not been meeting patient or provider needs.
Communication
Historically, communication about incidental findings has been less than optimal. This may be in part due to a lack of closed-loop communication (Kwan, 2017), which includes sending and receiving of the incidental finding alert, as well as evidence of follow-up. Even in cases when the radiologist sends an alert to the ordering provider, this alert is not always acknowledged. APRNs are well-equipped to be the communicator between patients, radiologists, primary care providers, ordering providers, and specialists.
The current role of the hospital APRN includes inter-professional practice and team work (Hurlock-Chorostecki & McCallum, 2016). The APRN as incidental findings coordinator could be compared to the interdisciplinary rounding teams developed in the last decade, which successfully included pharmacists to decrease medication errors (Kucukarslan, Peters, Mlynarek, & Nafziger, 2003).
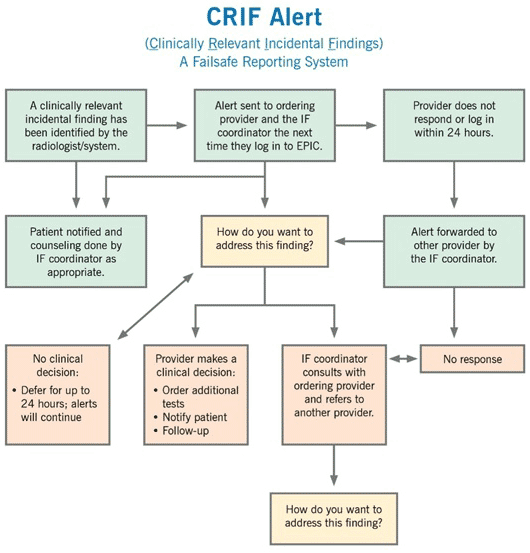
An alert algorithm embedded into the electronic medical record is proposed as an important adjunct to the incidental findings coordinator role.As the incidental findings coordinator, the APRN would receive communication from the radiologist via an automated alert, email, or phone call, depending on the situation and the dynamics of the department. An alert algorithm embedded into the electronic medical record is proposed as an important adjunct to the incidental findings coordinator role. The Figure is an example of a possible algorithm that could be used for the purposes of alerting providers, and to further defragment care. The radiologist would ultimately be the one to determine the urgency of notification but the incidental findings coordinator, and other nurses as needed, would be involved from the very beginning. Providers report receiving dozens of alerts per day (Singh et al., 2013), so it is not surprising that many incidental finding alerts go unacknowledged. As a facilitator of communication, the incidental findings coordinator would fill this gap, utilizing alert systems, and enabling closed-loop communication between radiologist, provider, and patient.
Figure. Clinically Relevant Incidental Findings: A Failsafe Reporting System (CRIF Alert ©). (Reprinted with Permission)
Patients trust that their providers will keep them informed and provide appropriate follow-up care.The incidental findings coordinator may frequently need to counsel patients on both benign and life threatening test results. Recognizing that patients have the right to know, and their autonomy must be respected, coordinators need to balance patient notification with the potential for psychological harm (Schaefer & Savulesca, 2018). Patients trust that their providers will keep them informed and provide appropriate follow-up care. APRNs, having had a background in bedside nursing, are practiced in the art of quickly developing rapport while supporting trust in the relationship between patient and provider. APRNs offer patient communication and counseling, while at the same time, maintaining inter-professional relationships, collaboration, and trust with other practitioners involved in patient care.
Long term follow-up
There are many gaps in current practice that need to be addressed to ensure that there is seamless communication and careful tracking of patients who are transferred or discharged. Patients who have a clinically relevant incidental finding may be lost to follow-up if there is not a deliberate effort to schedule timely testing and treatment. When patients do not attend follow-up appointments or go to another facility for care, they are vulnerable to becoming lost to follow-up.
In addition, patients are sometimes discharged from the ED after an initial reading of the CT scan, which is later amended to reveal an incidental finding (Andrawes et al., 2017). In these situations, patients need another contact. The APRN incidental findings coordinator or team member would have the role of counseling patients before discharge to assure appointments are made; patients understand the importance of follow-up; and contact information is correct.
Long term follow-up of abnormal results is recommended (Al Mutairi et al., 2015) and would be an appropriate role for the incidental findings coordinator. APRNs have the advanced training necessary to follow test results, order additional tests, treat within the APRN scope of practice, and collaborate and refer as necessary.
Conclusion
The current processes to address incidental findings is inconsistent at best and dangerous at its worst.The APRN incidental findings coordinator role has the potential to solve many problems encountered in current practice. Patient notification, appropriate counseling, and follow-up is likely to increase, as well as patient involvement in their own care. An APRN could reduce costs and patient risk as a result of treating clinically significant incidental findings and employing watchful waiting as needed, thus avoiding unnecessary testing and over-treatment. The APRN incidental findings coordinator would contribute clinical expertise to refer to the appropriate specialist, and collaborate to order tests and treat as needed or recommended by the specialist. Well-documented notification, follow-up, and appropriate treatment could easily reduce potential litigation.
The current processes to address incidental findings is inconsistent at best and dangerous at its worst. Ultimately, the implementation of a new role for the APRN as incidental findings coordinator could make missed or delayed follow-up a thing of the past. However, research is needed to examine the effectiveness of the role and its effect on patient outcomes. Innovative solutions are long overdue. An APRN incidental findings coordinator, working at the full scope of licensure, could improve care quality and patient safety.
Authors
Lee Anne Siegmund, PhD, RN, ACSM-CEP
Email: siegmul@ccf.org
Lee Anne Siegmund is a nurse scientist in Cleveland Clinic’s Office of Nursing Research and Innovation. She has an ongoing desire to improve clinical practice so as to prevent disease and complications resulting from non-optimized behaviors. She chairs Cleveland Clinic’s Annual Nursing Innovation Summits and seeks innovative ways to improve patient outcomes. As the nursing research mentor to Cleveland Clinic’s Quality and Patient Safety and Radiology Institutes, she has developed an interest in addressing clinically relevant incidental findings using innovative approaches. Dr. Siegmund has clinical experience in various inpatient and outpatient settings and has published research on adherence to exercise, use of social media to increase motivation in cardiac rehabilitation, and functional capacity in patients with metabolic syndrome. She has taught at Lorain County Community College in Elyria, Ohio, and at Calvin University in Grand Rapids, Michigan.
Aaron Hamilton, MD
Email: hamilta3@ccf.org
Aaron Hamilton is a practicing hospitalist and also serves as the Associate Chief Quality Officer for the Cleveland Clinic Health System. In this role, he has been involved in setting strategic direction and creating focus to advance improvement related to quality and safety for the health system. One specific focus area has been setting and driving the Cleveland Clinic Health System culture with a focus on eliminating all preventable harm within the healthcare system. He and his team have worked to tie these efforts to high reliability principles with a specific focus on 'Listening, Learning and Leading.' He also has a keen interest in better understanding the relationship between a culture of safety and direct patient outcomes, while advocating for and engaging patients and their family. He is a grant-funded researcher and has active studies looking at venous thromboembolism (VTE) prevention, inpatient pneumonia care, and the impact of mobility on medical patients.
Thaddeus Nespeca, RN, MSN, C-FNP
Email: nespect@ccf.org
Thaddeus Nespeca is an advanced practice registered nurse at the Cleveland Clinic Epilepsy Center. He has worked in various roles as a nurse practitioner in the Epilepsy Center, with each role being an innovative approach to fill a gap in the patient experience. These roles include: inpatient nurse practitioner providing psychiatric interviews; nurse practitioner for established patient, same-day appointments; and ambulatory nurse for preliminary clinical assessment, and triaging of outside hospital records for patients who live far from the Cleveland Clinic Epilepsy Center and are living with a chronic condition. These roles sparked an avid curiosity for unique approaches to improving quality of life, the patient experience, and access to healthcare for people living with chronic and acute conditions. He continues to be involved in APRN advocacy with the Cleveland Clinic APRN Council.
References
Adams, S. J., Rakheja, R., Bryce, R., & Babyn, P. S. (2018). Incidence and economic impact of incidental findings on 18F-FDG PET/CT imaging. Canadian Association of Radiologists Journal, 69(1), 63-70. doi: 10.1016/j.carj.2017.08.001
Adams, S. J., Babyn, P.S., & Danilkewich, A. (2016). Toward a comprehensive management strategy for incidental findings in imaging. Canadian Family Physician, 62(7), 541-543.
Agarwal, S., Talia, J., Liu, P., Momoh, A., & Kozlow, J. (2016). Determining the cost of incidental findings for patients undergoing preoperative planning for abdominally based perforator free flap breast reconstruction with computed tomographic angiography. Plastic and Reconstructive Surgery, 138(5), 804e-810e. doi: 10.1097/PRS.0000000000002621
Al Mutairi, A. Meyer, A. N., Chang, P., & Singh, H. (2015). Lack of timely follow-up of abnormal imaging results and radiologists' recommendations. Journal of the American College of Radiology, 12(4), 385-389. doi: 10.1016/j.jacr.2014.09.031
Andrawes, P., Picon, A. I., Shariff, M. A., Azab, B., von Waagner, W., Dimissie, S., & Fasanya, C. (2017). CT scan incidental findings in trauma patients: does it impact hospital length of stay? Trauma Surgery and Acute Care Open, 2(1), e000101. doi: 10.1136/tsaco-2017-000101
Berland, L. L., Silverman, S. G., Gore, R. M., Mayo-Smith, W. W., Megibow, A. J., Yee, J., Brink, J. A., Baker, M. E., Federle, M. P., Foley, W. D., Francis, I. R., Herts, B. R., Israel, G. M., Krinsky, G., Platt, J. F., Shuman, W. P., & Taylor, A. J. (2010). Managing incidental findings on abdominal CT: White paper of the ACR incidental findings committee. Journal of the American College of Radiology, 7(10), 754-773. doi: 10.1016/j.jacr.2010.06.013
Cieszanowski, A., Maj, E., Kulisiewicz, P., Grudzinski, I. P., Jakoniuk-Glodala, K., Chlipala-Nitek, I., Kaczynski, B., & Rowinski, O. (2014). Non-contrast-enhanced whole-body magnetic resonance imaging in the general population: The incidence of abnormal findings in patients 50 years old and younger compared to older subjects. PLoS One, 9(9), e107840. doi: 10.1371/journal.pone.0107840
Collins, C. E., Cherng, N., McDade, T., Movahedi, B., Emhoff, T. A., Whalen, G. F., LaFemina J., & Dorfman, J. D. (2015). Improving patient notification of solid abdominal viscera incidental findings with a standardized protocol. Journal of Trauma Management and Outcomes, 9(1), 1-6. doi: 10.1186/s13032-014-0022-x
Dunn, K., & Rogers, J. (2016). Discharge facilitation: An innovative PNP role. Journal of Pediatric Health Care, 30(5), 499-505. doi: 10.1016/j.pedhc.2015.10.004
Fakler, J. K., Ozkurtul, O., & Josten, C. (2014). Retrospective analysis of incidental non-trauma associated findings in severely injured patients identified by whole-body spiral CT scans. Patient Safety in Surgery, 8, 36. doi: 10.1186/s13037-014-0036-3
Gibson, L. M., Paul, L., Chappel, F. M., Macleod, M., Whiteley, W. N., Salman, R. A., Wardlaw, J. M., & Sudlow, C. L. M. (2018). Potentially serious incidental findings on brain and body magnetic resonance imaging of apparently asymptomatic adults: Systematic review and meta-analysis. British Medical Journal, 363, k4577. doi: 10.1136/bmj.k4577
Hickner, J., Graham, D. G., Elder, N. C., Brandt, E., Emsermann, C. B., Dovey, S., & Phillips, R. (2008). Testing process errors and their harms and consequences reported from family medicine practices: A study of the American Academy of Family Physicians National Research Network. Quality and Safety in Health Care, 17(3), 194-200. doi: 10.1136/qshc.2006.021915
Holliday, J., Samanta, D., Budinger, J., Hardway, J., & Bethea, A. (2017). An outcome analysis of nurse practitioners in acute care trauma services. Journal of Trauma Nursing, 24(6), 365-370. doi: 10.1097/JTN.0000000000000327
Hurlock-Chorostecki, C., & McCallum, J. (2016). Nurse practitioner role value in hospitals: New strategies for hospital leaders. Nursing Leadership, 29(3), 82-92. doi: 10.12927/cjnl.2016.24895
Huynh, T. T., Moran, K. R., Blackburn, A. H., Jacobs, D. G., Thomason, M. H., & Sing, R. F. (2008). Optimal management strategy for incidental findings in trauma patients: An initiative for midlevel providers. Journal of Trauma, 65(2), 331-334. doi: 10.1097/TA.0b013e31817e5153
James, M. K., Francois, M. P., Yoeli, G., Doughlin, G. K., & Lee, S. W. (2017). Incidental findings in blunt trauma patients: Prevalence, follow-up documentation, and risk factors. Emergency Radiology, 24(4), 347-353. doi: 10.1007/s10140-017-1479-5
Kucukarslan, S. N., Peters, M., Mlynarek, M., & Nafziger, D. A. (2003). Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Archives of Internal Medicine, 163(17), 2014-2018. doi: 10.1001/archinte.163.17.2014
Kwan, J. L, Yermak, D., Markell, L., Paul, N. S., Shojania, K. G., & Cram, P. (2019). Follow up of incidental high-risk pulmonary nodules on computed tomography pulmonary angiography at care transitions. Journal of Hospital Medicine, 14(6), 349-352. doi: 10.12788/jhm.3128
Kwan, J. L. (2017). Assigning responsibility to close the loop on radiology test results. Diagnosis, 4(3), 173–177. doi: 10.1515/dx-2017-0019
Lumbreras, B., Donat, L., Hernandez-Aquado, I. (2010). Incidental findings in imaging diagnostic tests: A systematic review. British Journal of Radiology, 83(988), 276-289. doi: 10.1259/bjr/98067945
Murphy, D. R., Thomas, E. J., Meyer, A. N., & Singh, H. (2015). Development and validation of electronic health record-based triggers to detect delays in follow-up of abnormal lung imaging findings. Radiology, 277(1), 81-87. doi: 10.1148/radiol.2015142530
Nelson, E., Bobade, R., Hunt, V., & Mundi, M. S. (2018). Optimizing adult diabetes care in community health. Journal of the American Association of Nurse Practitioners, 30(8), 443-449. doi: 10.1097/JXX.0000000000000042
O’Connor, S. D., Dalal, A. K., Sahni, V. A., Lacson, R., & Khorasani, R. (2016). Does integrating nonurgent, clinically significant radiology alerts within the electronic health record impact closed-loop communication and follow-up? Journal of the American Medical Informatics Association, 23(2), 333-338. doi: 10.1093/jamia/ocv105
O’Sullivan, J. W., Muntinga, T., Grigg, S., & Ioannidis, J. P. A. (2018). Prevalence and outcomes of incidental imaging findings: Umbrella review. British Medical Journal, 361, k2387. doi: 10.1136/bmj.k2387
Paluska, T. R., Sise, M. J., Sack, D. I., Sise, C. B., Egan, M. C., & Biondi, M. (2007). Incidental CT findings in trauma patients: Incidence and implications for care of the injured. Journal of Trauma, 62(1), 157-61. doi: 10.1097/01.ta.0000249129.63550.cc
Raich, P. C., Whitley, E. M., Thorland, W., Valverde, P., & Fairclough, D. (2012). Patient navigation improves cancer diagnostic resolution: an individually randomized clinical trial in an underserved population. Cancer Epidemiology, Biomarkers & Prevention 21(10), 1629-1638. doi: 10.1158/1055-9965.EPI-12-0513
Ravindran, S. Hancox, S. H., Barlow, N., Dunk, A., & Howlett, D. (2016). Unexpected findings in magnetic resonanceenterography and their clinical significance. Canadian Journal Of Gastroenterology & Hepatology, 4020569. doi: 10.1155/2016/4020569
Rosenkrantz, A. B., Xue, X., Gyftopoulos, S., Kim, D. C., & Nicola, G. N. (2018a). Downstream costs associated with incidental pulmonary nodules detected on CT. Academic Radiology, 26(6),798-802. doi: 10.1016/j.acra.2018.07.005
Rosenkrantz, A. B., Xue, X., Gyftopoulos, S., Kim, D. C., & Nicola, G. N. (2018b). Downstream costs associated with incidental pancreatic cysts detected at MRI. American Journal Of Roentgenology, 211(6), 1278-1282. doi: 10.2214/AJR.18.19885
Schaefer, G. O., & Savulesca, J. (2018). The right to know: A revised standard for reporting incidental findings. Hastings Center Report, 48(2), 22-32. doi: 10.1002/hast.836
Showkathali, R., Sen, A., Brickham, B., Dworakowski, R., Wendler, O., & MacCarthy, P. (2015). "Incidental findings" during TAVI work-up: More than just an inconvenience. EuroIntervention, 11(4), 465-9. doi: 10.4244/EIJY14M06_04
Sich, N., Rogers, A., Bertozzi, D., Sabapathi, P., Alswealmeen, W., Lim, P., Sternlieb, J., Gartner, L., Yuschak, J., Kirton, O., & Shadis, R. (2018). Filling the void: A low-cost, high-yield approach to addressing incidental findings in trauma patients. Surgery, 163(4), 657-660. doi: 10.1016/j.surg.2017.09.043
Singh, H., Thomas, E. J., Mani, S., Sittig, D., Arora, H., Espadas, D., Khan, M. M., & Petersen, L. A. (2009). Timely follow up of abnormal diagnostic imaging test results in an outpatient setting: are electronic medical records achieving their potential? Archives of Internal Medicine, 169(17), 1578–1586. doi:10.1001/archinternmed.2009.263
Singh, H., Spitzmueller, C., Petersen, N. J., Sawhney, M. K., & Sittig, D. H. (2013). Information overload and missed test results in electronic health record-based settings. Journal Of The American Medical Association Internal Medicine, 173(8), 702-704. doi: 10.1001/2013.jamainternmed.61
Sperry, J. L., Massaro, M. S., Collage, R. D., Nicholas, D. H., Forsythe, R. M., Watson, G. A., Marshall, G.T., Alarcon, L. H., Billiar, T. R., & Pietzman, A.B. (2010). Incidental radiographic findings after injury: Dedicated attention results in improved capture, documentation, and management. Surgery, 148(4), 618-624. doi: 10.1016/j.surg.2010.07.017
Thrall, J. H., Li, X., Li, Q., Cruz, C., Do, S., Dreyer, K., & Brink, J. (2018). Artificial intelligence and machine learning in radiology: Opportunities, challenges, pitfalls, and criteria for success. Journal of the American College of Radiology, 15(3 Pt B), 504-508. doi: 10.1016/j.jacr.2017.12.026
Tuncel, S. A., Çaglı, B., Tekatas, A., Kırıcı, M. Y., Ünlü, E., & Gençhellaç, H. (2015). Extraspinal incidental findings on routine MRI of lumbar spine: Prevalence and reporting rates in 1278 patients. Korean Journal of Radiology, 16(4), 866-873. doi: 10.3348/kjr.2015.16.4.866
Wheeler, S. M., & Bryant, A. S. (2017). Racial and ethnic disparities in health and health care. Obstetrics And Gynecology Clinics Of North America, 44(1), 1-11. doi: 10.1016/j.ogc.2016.10.001
Yang, Y. T., & Meiners, M. R. (2014). Care coordination and the expansion of nursing scopes of practice. Journal of Law, Medicine & Ethics, 42(1), 93-103. doi: 10.1111/jlme.12122
Yeh, D. D., Imam, A. M., Truong, S. H., McLaughlin, E. L., Klein, E. N., Avery, L. L., & Velmahos, G. C. (2013). Incidental findings in trauma patients: Dedicated communication with the primary care physician ensures adequate follow-up. World Journal of Surgery, 37(9), 2081-2085. doi: 10.1007/s00268-013-2092-8

